Facing a serious medical condition can be overwhelming, and for women who dream of becoming mothers someday, the possibility of losing fertility can add an extra layer of anxiety. Thankfully, fertility preservation offers hope. It allows women to safeguard their ability to have biological children, even if their treatment plans or diagnoses pose a threat to their reproductive health.
Whether it’s understanding what fertility preservation is, exploring the best methods for preserving eggs for fertility, or learning about the latest fertility preservation guidelines, being informed can help you make empowered decisions. This guide explores everything you need to know about fertility preservation procedures, especially when dealing with critical health challenges like cancer or autoimmune diseases.
Synopsis
- What is Fertility Preservation?
- Why Should Women Consider Fertility Preservation During Medical Treatments?
- Best Fertility Preservation Options for Women Facing Medical Conditions
- Special Focus: Fertility Preservation in Breast Cancer Patients
- Fertility Preservation Guidelines: What You Should Know?
What is Fertility Preservation?
In simple terms, fertility preservation refers to the various medical techniques used to protect a woman's ability to conceive in the future. If you're diagnosed with a health condition that could affect your reproductive system, such as cancer, lupus, or endometriosis, you might want to consider options for preserving eggs for fertility or even freezing embryos.
Understanding what fertility preservation is becomes crucial when your medical journey might impact your future family plans. With advancements in reproductive medicine, there are now safe and effective ways to preserve fertility, even during challenging health battles.
Why Should Women Consider Fertility Preservation During Medical Treatments?
Medical treatments like chemotherapy, radiation therapy, and some surgeries can significantly reduce ovarian reserve or even cause infertility. For instance, fertility preservation in breast cancer patients has become an important focus because certain chemotherapy regimens are known to damage the ovaries.
Women who have genetic risks for early menopause, or those who have to undergo surgeries like ovarian cyst removal, are also excellent candidates for fertility preservation procedures. Planning early ensures you have options later when you’re ready to start or expand your family.
If you're wondering whether you should consider fertility preservation, here’s a simple guideline: if your upcoming treatment or medical condition might affect your ovaries or uterus, it’s worth discussing fertility preservation with your doctor.
Best Fertility Preservation Options for Women Facing Medical Conditions
Choosing the right method of fertility preservation depends on your age, health status, time available before starting treatment, and personal preferences. Here are the most recommended options:
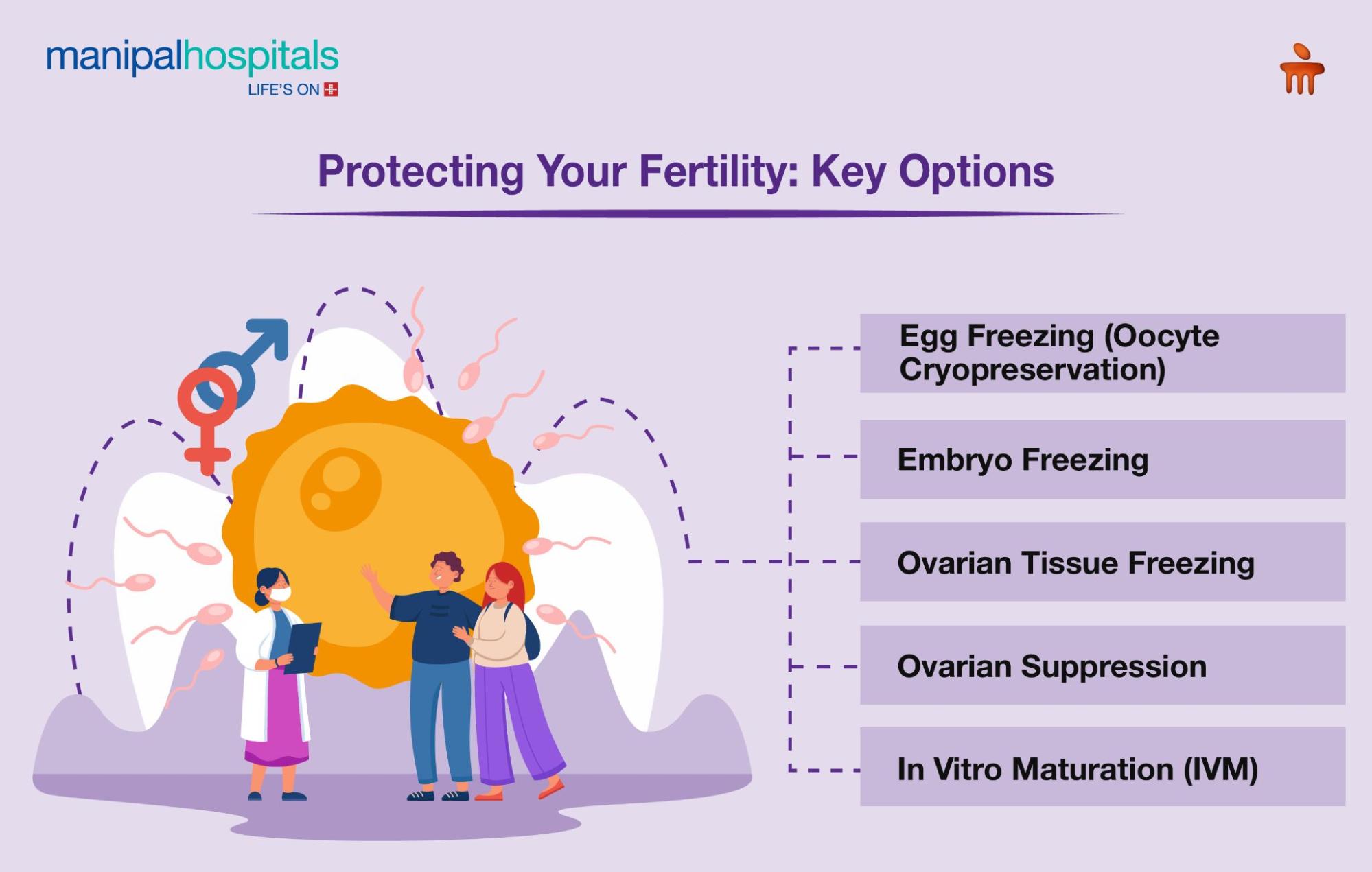
1. Egg Freezing (Oocyte Cryopreservation)
One of the most popular and successful methods, egg freezing, involves stimulating the ovaries to produce multiple eggs, retrieving them, and then freezing them unfertilized for future use.
This fertility preservation procedure is ideal for women who want to delay pregnancy or need urgent medical treatments. Especially for young women, preserving eggs for fertility before chemotherapy or surgery offers a higher chance of a successful pregnancy later on.
Egg freezing is particularly crucial for fertility preservation in breast cancer patients, where the timing between diagnosis and the start of chemotherapy is tight.
2. Embryo Freezing
If you have a partner or are open to using donor sperm, embryo freezing can be an excellent option. In this process, eggs are fertilised with sperm to create embryos, which are then frozen.
Following standard fertility preservation guidelines, embryo freezing often offers slightly higher success rates than egg freezing. It’s a more established fertility preservation procedure, but it does require future decisions about the embryos, especially if circumstances change.
3. Ovarian Tissue Freezing
Ovarian tissue freezing is a newer technique where a surgeon removes and freezes part of the ovarian tissue. Later, the tissue can be transplanted back into the body to restore hormonal function and fertility.
This option is often used when immediate treatment is needed, leaving no time for traditional egg stimulation cycles. It’s also a good choice for prepubescent girls who are not yet producing mature eggs.
For women needing urgent cancer therapy, this fertility preservation procedure can be a real game-changer in efforts to preserve fertility.
4. Ovarian Suppression
Another approach under fertility preservation guidelines is using hormone therapy to temporarily "put the ovaries to sleep" during chemotherapy. Medications called GnRH agonists are given to protect the ovaries.
While ovarian suppression is not as reliable as egg or embryo freezing, it can serve as an additional layer of protection, particularly when combined with other fertility preservation methods.
5. In Vitro Maturation (IVM)
In this emerging field, doctors collect immature eggs and mature them in the lab before freezing.
IVM is a promising solution for women who cannot undergo the hormonal stimulation required for traditional egg freezing, for example, certain fertility preservation in breast cancer patients who are sensitive to hormone fluctuations.
Although success rates are currently lower than standard egg freezing, ongoing advancements continue improving outcomes.
Special Focus: Fertility Preservation in Breast Cancer Patients
Fertility preservation in breast cancer patients deserves particular attention because the need to start cancer treatment quickly can limit fertility preservation options.
Typically, oncologists recommend preserving eggs for fertility or freezing embryos before starting chemotherapy. Some breast cancer treatments can lower hormone levels, affecting fertility even after remission. Therefore, early referral to a reproductive specialist is crucial to explore safe fertility preservation procedures without delaying essential cancer care.
Moreover, many hospitals now follow dedicated fertility preservation guidelines for oncology patients, ensuring that fertility conversations are integrated early into the cancer care plan.
Fertility Preservation Guidelines: What You Should Know?
Following proper fertility preservation guidelines can make a significant difference in outcomes. Here are some key takeaways:
-
Act early: Ideally, meet with a fertility specialist soon after diagnosis and before starting any gonadotoxic treatment.
-
Assess your options: Not every woman’s situation is the same. A personalised fertility preservation plan based on your age, diagnosis, and treatment timeline is essential.
-
Understand the process: Knowing what to expect — from ovarian stimulation to egg retrieval — can help you feel more confident.
-
Be emotionally prepared: Fertility preservation is empowering, but it can also be emotionally complex. Seeking counselling or support groups can be very helpful.
-
Know your coverage: Some insurance plans cover fertility preservation for medical reasons. Always check beforehand.
By following these fertility preservation guidelines, you can make the best possible decisions for your reproductive future.






















 6 Min Read
6 Min Read