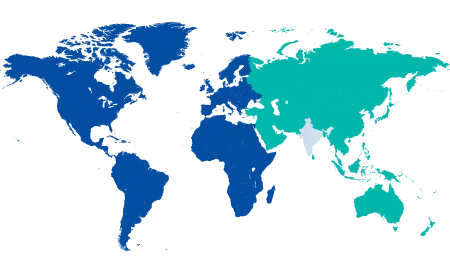
Dyslipidemia is a condition that affects millions of people worldwide, often silently progressing until it leads to serious health problems. Characterised by abnormal levels of lipids (fats) in the blood, including cholesterol and triglycerides, dyslipidemia is a major contributor to cardiovascular diseases (CVDs), which remain the leading cause of death globally.
But dyslipidemia doesn’t occur in isolation. It is often closely associated with endocrine and metabolic disorders, such as diabetes, hypothyroidism, obesity, and polycystic ovarian syndrome (PCOS). Understanding this connection is essential for effective prevention, diagnosis, and management.
In this blog, we’ll explore what dyslipidemia is, how it links with endocrine and metabolic disorders, and what steps you can take to manage it effectively.
Synopsis
What is Dyslipidemia?
Dyslipidemia refers to an abnormal amount of lipids in the blood. These abnormalities typically involve:
-
High levels of total cholesterol
-
High levels of low-density lipoprotein (LDL) cholesterol (often called “bad cholesterol”)
-
Low levels of high-density lipoprotein (HDL) cholesterol (“good cholesterol”)
-
High levels of triglycerides
A person may have one or more of these lipid abnormalities. Dyslipidemia disease can be primary (genetic) or secondary, resulting from lifestyle factors or other medical conditions.
How Do Endocrine and Metabolic Disorders Influence Lipid Levels?
The endocrine system regulates hormones, which in turn control many body functions, including metabolism—the process by which the body uses food for energy and growth. When this system is disrupted, it can lead to metabolic changes that affect how lipids are produced, processed, and eliminated from the body.
Here’s how common endocrine and metabolic disorders are linked to dyslipidemia:
1. Diabetes Mellitus (Type 2 and Type 1)
Dyslipidemia is very common in individuals with diabetes, especially Type 2 Diabetes. This is largely due to insulin resistance, which impairs the normal processing of lipids.
-
Typical lipid profile in diabetes:
-
Increased triglycerides
-
Increased LDL cholesterol (small, dense particles)
-
Decreased HDL cholesterol
This pattern, often referred to as diabetic dyslipidemia, increases the risk of atherosclerosis, a condition where arteries become clogged with fatty deposits, leading to heart attacks and strokes.

2. Hypothyroidism
The thyroid gland regulates metabolism, and low thyroid hormone levels (hypothyroidism) slow down many body processes, including lipid metabolism.
In hypothyroidism, the liver’s ability to clear LDL cholesterol is reduced, leading to:
-
Increased LDL cholesterol
-
Increased total cholesterol
Untreated hypothyroidism can significantly raise the risk of cardiovascular problems.
3. Obesity and Metabolic Syndrome
Obesity, especially when concentrated around the abdomen, is strongly associated with insulin resistance and lipid abnormalities.
Metabolic syndrome is a cluster of conditions—including abdominal obesity, high blood sugar, high blood pressure, and dyslipidemia—that together increase the risk of heart disease, stroke, and type 2 diabetes.
Lipid profile in metabolic syndrome typically shows:
-
High triglycerides
-
Low HDL cholesterol
4. Polycystic Ovarian Syndrome (PCOS)
PCOS is a hormonal disorder common in women of reproductive age. Many women with PCOS have insulin resistance, which contributes to both hyperinsulinemia and dyslipidemia.
Lipid abnormalities in PCOS include:
-
Elevated LDL and total cholesterol
-
Elevated triglycerides
-
Decreased HDL cholesterol
This combination increases the risk of cardiovascular disease in young women with PCOS.
5. Cushing's Syndrome and Growth Hormone Disorders
Excess cortisol in Cushing's Syndrome and altered growth hormone levels in conditions like acromegaly can also impact lipid metabolism, leading to increased LDL and triglyceride levels.
Dyslipidemia Symptoms and Diagnosis
Dyslipidemia itself doesn’t usually cause symptoms, which is why regular screening is important, especially for those with existing endocrine or metabolic disorders.
Diagnosis is made through a lipid profile test, which measures:
-
Total cholesterol
-
LDL cholesterol
-
HDL cholesterol
-
Triglycerides
Fasting may be required for the most accurate results, especially for triglyceride levels.
Why It Matters: Complications of Dyslipidemia
If left unchecked, dyslipidemia can lead to:
-
Atherosclerosis: Fatty deposits narrow and harden the arteries.
-
Coronary Artery Disease: Can lead to angina or heart attacks.
-
Stroke: Due to reduced blood flow to the brain.
-
Peripheral artery disease: Causing pain and mobility issues.
-
Pancreatitis: Especially with very high triglyceride levels.
When combined with diabetes or thyroid disorders, these risks are multiplied.
Management and Treatment
1. Lifestyle Changes
These are the first line of defence against dyslipidemia and are often very effective:
-
Healthy diet: Low in saturated fats, trans fats, and cholesterol. Include more fibre-rich foods and healthy fats (like omega-3s).
-
Exercise: At least 150 minutes of moderate aerobic activity per week.
-
Weight loss: Even a 5–10% reduction in body weight can improve lipid levels.
-
Limit alcohol and quit smoking: Both can raise triglyceride levels and worsen outcomes.
2. Medications
If lifestyle changes aren’t enough, doctors may prescribe medications such as:
-
Statins: Lower LDL and reduce cardiovascular risk.
-
Fibrates: Mainly used to reduce triglycerides.
-
Niacin: Helps increase HDL.
-
Ezetimibe: Reduces cholesterol absorption from food.
-
PCSK9 inhibitors: Used in cases where LDL remains high despite statin use.
In patients with endocrine disorders like diabetes or hypothyroidism, treating the underlying condition often helps improve lipid profiles as well.
Regular Monitoring is Key
Patients with diabetes, hypothyroidism, PCOS, or other hormonal imbalances should have their lipid levels checked regularly. Early detection allows for timely intervention and helps prevent long-term complications.
Conclusion
Dyslipidemia disease might not make headlines the way heart attacks or strokes do, but it plays a critical role behind the scenes in causing these life-threatening conditions. For people with endocrine and metabolic disorders, managing lipid levels becomes even more important.
The good news? It’s manageable—with the right blend of lifestyle changes, medical treatment, and regular monitoring.
If you’re living with diabetes, thyroid disorders, PCOS, or struggling with abnormal cholesterol levels, don’t wait for complications to arise. At Manipal Hospitals Jaipur, our expert team of endocrinologists, cardiologists, and internal medicine specialists work together to offer comprehensive screening, diagnosis, and treatment for dyslipidemia and related endocrine disorders.
Book an appointment now!
FAQ's
Dyslipidemia includes any abnormal lipid levels (high LDL, low HDL, high triglycerides), while high cholesterol usually refers to just elevated cholesterol levels.
Yes, hormonal imbalances can disrupt fat metabolism, leading to abnormal cholesterol and triglyceride levels.
Usually no symptoms. It’s often silent and found through routine blood tests.
At least once a year, or more frequently if your doctor advises.
Yes, in mild cases. A healthy diet, exercise, and weight loss can help, though some may still need medication.





















 4 Min Read
4 Min Read