Our heart is an incredible engine, tirelessly pumping blood, beating over 100,000 times a day to keep us moving. But imagine if this vital organ, which works so hard for us, suddenly found itself in a vise, unable to fully expand and do its job. That’s essentially what happens with constrictive pericarditis, a rare but significant chronic heart condition.
In simple terms, constrictive pericarditis occurs when the pericardium, the protective, double-layered sac surrounding our heart, becomes inflamed, thickens, and loses its natural elasticity over time. Instead of acting as a flexible shield, it transforms into a stiff, unyielding casing. This thickening of the heart membrane puts immense pressure on the heart, restricting its ability to fill properly with blood during each beat. The result? Symptoms that often mimic heart failure and, if left unaddressed, can lead to serious long-term complications.
Understanding this condition, recognising its subtle signs, and seeking timely medical care are crucial. Let’s dive deeper into what constrictive pericarditis is, its underlying causes, the tell-tale symptoms, and how it can be effectively treated.
Synopsis
- What Exactly is Constrictive Pericarditis?
- Spotting the Signs: Symptoms of Constrictive Pericarditis
- Unraveling the Root: Causes of Constrictive Pericarditis
- The Diagnostic Journey: Pinpointing Constrictive Pericarditis
- Paving the Path to Recovery: Treatment of Constrictive Pericarditis
- Proactive Steps: Preventing Constrictive Pericarditis
- When to Consult a Cardiologist
- Conclusion
What Exactly is Constrictive Pericarditis?
The meaning of "constrictive" in constrictive pericarditis is key. Due to persistent inflammation, scarring, and sometimes even calcium deposits, the normally pliable pericardium becomes rigid. Think of it like a straitjacket around the heart. This "stiff casing" prevents the heart chambers from fully expanding and relaxing as they should to receive blood, particularly during the diastolic phase (when the heart fills). This limited movement directly impacts blood flow, especially when the body is under physical activity or stress, as the heart simply can’t keep up with the demand for increased blood supply.
Spotting the Signs: Symptoms of Constrictive Pericarditis
The symptoms of constrictive pericarditis can be a bit of a chameleon, often mimicking other heart or lung conditions, which can make diagnosis challenging. However, certain signs tend to be consistently present in patients. If you notice these, especially in combination, it’s a strong signal to seek medical advice:
-
Shortness of breath (Dyspnea): This is a hallmark symptom, often worsening with exertion or when lying flat. You might find yourself propping up pillows at night to breathe more easily.
-
Swelling: Fluid retention is common, leading to noticeable swelling in the legs, ankles (edema) and sometimes even the abdomen (ascites), causing a feeling of bloating.
-
Fatigue and reduced stamina: Because the heart isn't efficiently pumping blood, your organs and muscles may not receive enough oxygen, leading to persistent tiredness and a significant drop in your energy levels.
-
Palpitations: Some individuals report a fluttering feeling or an awareness of their heartbeat in their chest.
-
Chest discomfort or tightness: While not always severe, a feeling of pressure or tightness in the chest can occur.
-
Weight gain: This is often due to fluid retention rather than an increase in body fat.
These can often be early symptoms of heart inflammation, especially if you have a history of certain infections, surgeries, or autoimmune diseases. Don't ignore these signals; getting them checked out sooner rather than later can make all the difference.
Unraveling the Root: Causes of Constrictive Pericarditis
Understanding the cause of constrictive pericarditis is vital, as it can significantly influence the treatment approach. While sometimes the exact cause remains elusive, some of the leading culprits include:
-
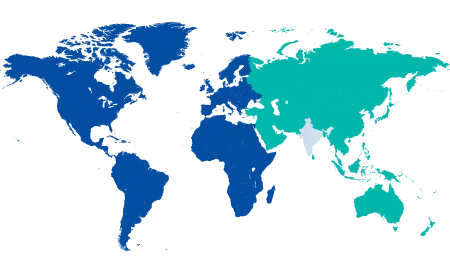
Pericarditis from infection: In countries like India, tuberculosis is still a prevalent cause of long-standing pericardial inflammation, which can eventually lead to constriction. Other viral or bacterial infections can also trigger it.
-
Pericarditis after heart surgery: Open-heart surgeries, valve replacements, or even coronary artery bypass grafts can sometimes lead to post-operative pericarditis that, in a subset of patients, progresses to constriction.
-
Radiation therapy to the chest: For individuals who have undergone radiation treatment for cancers in the chest area (like breast cancer or lymphoma), pericardial damage can occur years later, leading to constriction.
-
Autoimmune diseases: Systemic inflammatory conditions such as lupus or rheumatoid arthritis can sometimes affect the pericardium, leading to chronic inflammation and eventual constriction.
-
Trauma to the chest: Significant chest injuries can cause pericardial damage that may heal with scarring and lead to constriction over time.
-
Repeated inflammation episodes: Even if the initial cause isn't severe, recurrent bouts of acute pericarditis can eventually lead to chronic changes and thickening.
Knowing your medical history and any past events that might have affected your heart is crucial for your doctor in connecting the dots and arriving at an accurate diagnosis.
The Diagnostic Journey: Pinpointing Constrictive Pericarditis
Getting a clear diagnosis of constrictive pericarditis requires a meticulous approach, combining a detailed clinical evaluation with advanced imaging techniques. Doctors usually begin with:
-
Detailed history and physical examination: They'll ask about your symptoms and medical background and listen for specific signs like distended neck veins (due to increased pressure) or a characteristic "pericardial knock" sound during auscultation of the heart.
-
Echocardiogram (Echo): This is typically the first imaging test. It uses sound waves to create images of your heart and helps detect pericardial thickening, assess how well the heart fills during diastole, and look for specific signs of constriction like septal bounce (a paradoxical motion of the wall between the heart's pumping chambers).
-
Cardiac MRI (Magnetic Resonance Imaging): In more complex or unclear cases, a cardiac MRI of the pericardium can offer high-resolution images of the thickened membrane, showing any inflammation, scarring, or fluid accumulation. It's excellent for visualising the pericardium directly.
-
CT Scans (Computed Tomography): A cardiac CT scan can also be very useful, particularly for identifying calcium deposits within the pericardium, which are a strong indicator of chronic constriction.
-
Cardiac Catheterisation: This invasive procedure measures pressures within the heart chambers and can provide definitive evidence of the restrictive physiology characteristic of constrictive pericarditis.
Paving the Path to Recovery: Treatment of Constrictive Pericarditis
When it comes to constrictive pericarditis treatment, the approach is largely determined by the severity of the condition and its underlying cause.
-
Medications: In early or mild cases, or when there's still active inflammation, medications for pericarditis such as Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), corticosteroids, or colchicine may be prescribed to reduce inflammation and potentially slow the progression of thickening. Diuretics might also be used to manage fluid retention.
-
Pericardiectomy: For many patients, particularly those with advanced or persistent symptoms, surgical intervention is the primary and most effective treatment. The sed centremain procedure is a pericardiectomy—the surgical removal of the rigid, thickened pericardium. This "stripping" of the constricting sac allows the heart to expand properly again, significantly relieving symptoms and restoring heart function. While it's a major operation, the outcomes are generally favourable when performed by experienced cardiac surgeons at specialised centres.
Proactive Steps: Preventing Constrictive Pericarditis
While not every case of constrictive pericarditis can be prevented, early intervention and diligent management of initial pericardial inflammation remain the best strategies.
-
If you've ever had acute pericarditis due to infection or surgery, it’s vital to follow your doctor’s instructions meticulously and complete all prescribed courses of medication, such as antibiotics, to prevent chronic inflammation.
-
Wondering how to avoid pericarditis in the first place? Beyond immediate medical adherence, adopting simple heart inflammation prevention tips can contribute: maintain a healthy weight, engage in regular physical activity, manage stress effectively, and ensure any infections are treated promptly and thoroughly.
-
If you have an autoimmune condition, good management of your underlying disease can help reduce the risk of pericardial involvement.
When to Consult a Cardiologist
Knowing when to seek specialised medical attention can truly be life-saving. If you notice persistent or recurring symptoms like:
-
Unexplained shortness of breath (especially worsening with activity or when lying down)
-
New or worsening swelling in your legs, ankles, or abdomen.
-
Unexplained fatigue that limits your daily activities.
-
Persistent chest discomfort or tightness.
Especially if you have a history of heart issues, chest surgery, radiation, or chronic inflammatory conditions, do not delay. Our qualified cardiologists can conduct the necessary investigations, provide an accurate diagnosis, and guide your treatment plan effectively. It's always better to consult a heart doctor early and rule out complications than to wait for symptoms to escalate into an emergency.
Conclusion
In summary, comprehensive constrictive pericarditis care hinges on a timely and accurate diagnosis, a multidisciplinary approach involving cardiologists and cardiac surgeons, and, in many cases, surgical management. Whether you're in the early stages or dealing with the long-term effects, there are effective options available to help you lead a healthier, more active life. The key lies in awareness, prompt action, and access to experienced cardiac care.
With an early diagnosis of a heart condition like constrictive pericarditis and timely intervention, you can significantly improve your quality of life and protect your heart for the future. Book an appointment today!
FAQ's
No, it usually develops slowly over time following prolonged inflammation or untreated pericarditis.
Not always. Early cases may respond to anti-inflammatory medications before surgery is considered.
Recovery varies but typically takes 4–6 weeks, depending on overall health and complications.
If untreated, it can lead to heart failure, but timely treatment significantly improves outcomes.
Recurrence is rare, especially when the entire thickened pericardium is successfully removed.





















 4 Min Read
4 Min Read