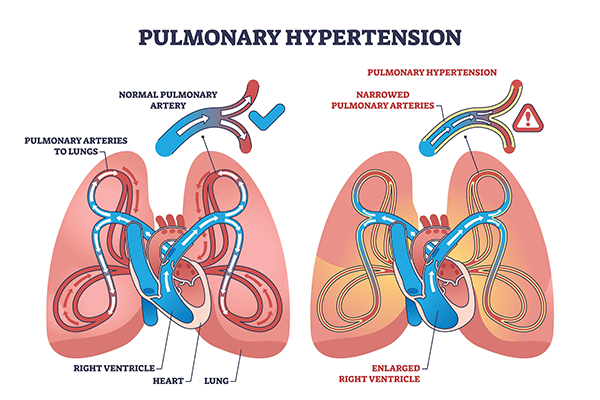
Do you often experience shortness of breath, chest pain, rapid heartbeat and dizziness? This can be a sign of pulmonary hypertension. Pulmonary hypertension (PH) is a serious medical condition which often gets overlooked and unreported until it worsens. To break it down further, it is characterised by abnormally high blood pressure in the arteries of the lungs. However, often subtle at first, manifesting as fatigue or shortness of breath, PH puts extra strain on the right side of the heart, leading to symptoms such as chest pain, swelling, palpitations, and dizziness.
If left unmanaged, this pressure overload can progress to right-sided heart failure and significantly impact quality of life. According to the latest reports, this condition affects about 1% of the global population and falls into five distinct categories based on its underlying cause. Though incurable in most forms, early recognition and treatment can slow progression and improve outcomes. This blog is aimed at sharing accurate medical information regarding its forms and symptoms that should be treated as red flags and must be reported immediately.
Synopsis
5 Types of Pulmonary Hypertension
1. Group I – Pulmonary Arterial Hypertension (PAH)
This precapillary form arises from narrowing, stiffening, or thickening of the small pulmonary arteries. Subtypes include idiopathic, heritable (often linked to BMPR2 mutations), drug/toxin‑induced, and those secondary to conditions such as connective tissue disease, congenital heart disease, HIV, cirrhosis/portal hypertension, schistosomiasis. It also includes pulmonary veno‑occlusive disease (PVOD) and persistent pulmonary hypertension of the newborn. These subtypes often require advanced targeted therapies (e.g. prostacyclin analogues, endothelin receptor antagonists).
2. Group II – Pulmonary Hypertension Due to Left Heart Disease
This is the most common type, resulting from elevated pressure in the pulmonary veins due to left-sided heart issues, such as heart failure (systolic or diastolic), mitral or aortic valve disease, or congenital/acquired cardiac defects. Blood backs up into the lung veins, raising pulmonary pressure.
3. Group III – Pulmonary Hypertension Due to Lung Disease and/or Hypoxia
This occurs secondary to chronic lung disorders or long-standing low oxygen levels, such as COPD, interstitial lung disease, sleep apnea, developmental lung disease, or chronic high-altitude exposure. Hypoxia induces pulmonary artery constriction and vascular remodelling. Management focuses on treating lung disease and correcting hypoxia, plus pulmonary rehabilitation.
4. Group IV – Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
In this type, unresolved blood clots—often recurrent or chronic pulmonary emboli—cause obstruction and vascular remodelling. This is the only potentially curable category, frequently treated with pulmonary thromboendarterectomy or balloon pulmonary angioplasty (if surgery is not feasible), plus medical therapy when needed.
5. Group V – Pulmonary Hypertension with Unclear or Multifactorial Mechanisms
This catch-all group includes PH associated with systemic or metabolic conditions that don’t fit the prior categories, such as sarcoidosis, chronic hemolytic anaemia, Gaucher disease, thyroid disorders, lymphangioleiomyomatosis, neurofibromatosis, tumours (mediastinal fibrosis), and chronic renal failure with or without dialysis. Treatment is complex and tailored to the underlying cause.
Classifying PH into these five groups is essential as each has distinct underlying causes, diagnostic approaches, and treatment strategies. Early, accurate diagnosis of pulmonary hypertension guides timely care and improves outcomes.
10 Warning Signs of Pulmonary Hypertension
-
Shortness of Breath (Dyspnea) - Often the earliest and most common sign—initially during exertion (climbing stairs or walking), later even at rest. Nearly all patients experience breathlessness by the time of diagnosis.
-
Unexplained Fatigue or Weakness - Persistent fatigue unrelated to activity level may reflect early cardiac stress from the right ventricle working overtime.
-
Chest Pain or Pressure - Discomfort or tightness in the chest—even without exertion—can result from the heart struggling to pump against high pressure in lung vessels.
-
Palpitations or Rapid Heartbeat - You may feel racing, pounding, or irregular heartbeats as the heart responds to increased strain on the pulmonary system.
-
Dizziness or Fainting (Syncope) - Lightheadedness or passing out—particularly during physical activity—signals dangerously low cardiac output or limited blood flow.
-
Swelling in Ankles, Legs or Abdomen (Oedema) - Fluid retention becomes visible as swelling in the legs or abdomen. Elevated right-heart pressures back up circulation into the veins.
-
Bluish Skin or Lips (Cyanosis) - Reduced oxygen delivery leads to a bluish tinge, especially in the lips and fingertips, reflecting advanced disease.
-
Upper Abdominal Discomfort or Fullness - A swollen or tender upper abdomen may result from liver congestion due to right-heart strain.
-
Dry Cough or Coughing Up Blood - A persistent dry cough—or, more rarely, hemoptysis—can be associated with advanced pulmonary arterial hypertension or vascular changes.
-
Hoarseness or Wheezing - Compression of laryngeal nerves from enlarged heart structures can cause persistent hoarseness, while wheezing may stem from pulmonary congestion.
What to Do If You Notice These Symptoms
If you experience any of these persistent symptoms—especially shortness of breath, swelling, dizziness, or chest pain—consult with our pulmonologist in Delhi today. Evaluation may include an echocardiogram, right heart catheterisation (gold standard), and additional tests like BNP, lung imaging, and sleep studies.
FAQ's
Diagnosis starts with clinical evaluation and echocardiography. Confirmatory tests include right heart catheterisation, imaging (e.g., CT, V/Q scan), pulmonary function testing, blood work, and sometimes a sleep study.
While most types (Groups I, II, III, V) are not curable, PH can be managed. CTEPH (Group IV) is potentially curable via surgery or specialised interventional procedures.
Treatments include pulmonary vasodilators (medicine that widens blood vessels), anticoagulants (in CTEPH), oxygen therapy, lifestyle modification, and surgical options when appropriate.
Risk factors include connective tissue disease, congenital heart disease, chronic lung conditions, HIV, liver disease, genetic predisposition, or prior pulmonary embolism. Women aged 30–60 are more commonly affected.
Management involves regular monitoring (to track functional status, biomarkers, and imaging), medication adherence, avoidance of high altitude, tailored nutrition and exercise, and referral to specialist PH centres.





















 5 Min Read
5 Min Read