Hypertension, commonly known as high blood pressure, is one of the most significant risk factors for heart disease. While it might seem like a standalone condition, hypertension often acts as a silent trigger, gradually damaging the heart and blood vessels over time. Understanding the connection between these two conditions is essential for effective prevention and management.
Hypertension occurs when the force of blood against the walls of the arteries remains consistently high. It is measured using two key numbers:
Systolic Pressure (the pressure when the heart beats)
Diastolic Pressure (the pressure when the heart rests between beats)
Blood pressure is typically expressed as systolic over diastolic (e.g., 120/80 mmHg). A reading of 140/90 mmHg or higher is generally considered hypertensive.
Synopsis
Why is Hypertension Dangerous?
High blood pressure strains the heart and arteries, increasing the risk of heart attack, stroke, and other cardiovascular diseases. Over time, it can lead to:
-
Arterial Damage and Narrowing: High pressure can cause the arteries to harden and narrow (atherosclerosis), reducing blood flow to the heart.
-
Enlarged Heart (Left Ventricular Hypertrophy): The heart has to work harder to pump blood, leading to thickened heart muscle that struggles to pump efficiently.
-
Heart Failure: If the heart cannot pump enough blood to meet the body’s needs, heart failure can develop.
-
Aneurysm: Increased pressure can weaken artery walls, forming a bulge (aneurysm) that can rupture, causing life-threatening bleeding.
More Reads: Types of Heart Block and How Electrophysiologists Manage Them
How Hypertension Leads to Heart Disease
The relationship between hypertension and heart disease is complex, involving several mechanisms:
|
Impact of Hypertension on the Heart |
Description |
|
Hypertensive heart disease |
Forces the heart to work harder, leading to muscle thickening and heart failure. |
|
Hypertensive disease |
Causes atherosclerosis, restricting blood flow to the heart muscle. |
|
Hypertensive heart disease without heart failure |
Narrowed or blocked arteries limit the heart’s oxygen supply, increasing the risk of a heart attack. |
|
Hypertensive heart failure |
It can cause the heart valves to function improperly, leading to further cardiac complications. |
Signs and Symptoms to Watch Out For
Hypertension is often called a “silent killer” because it can progress without noticeable symptoms in the early stages. However, as it advances, it can lead to:
-
Persistent Headaches: High blood pressure can trigger severe, throbbing headaches, often described as a pressure-like pain.
-
Chest Pain or Discomfort: Known as angina, this can feel like pressure, tightness, or squeezing in the chest, indicating reduced blood flow to the heart muscle.
-
Shortness of Breath: As the heart weakens, fluid can build up in the lungs, making it difficult to breathe, especially during physical activity or while lying flat.
-
Irregular Heartbeat (Palpitations): Hypertension can disrupt the heart's electrical signals, leading to skipped beats or rapid heart rates.
-
Fatigue and Confusion: Reduced heart function can limit oxygen-rich blood to the brain, causing confusion, memory problems, and extreme tiredness.
-
Vision Problems: High blood pressure can damage the blood vessels in the eyes, leading to blurred or reduced vision.
-
Pounding Sensation in the Chest, Neck, or Ears: This sensation often indicates that the heart is working harder than normal to pump blood.
Diagnosis and Monitoring
Accurate diagnosis and regular monitoring are essential for managing hypertension effectively. Some common methods include:
-
Home Blood Pressure Monitoring: Convenient and practical, this method allows patients to track their blood pressure regularly, providing a more comprehensive picture of their cardiovascular health. It helps detect early signs of hypertension and assess the effectiveness of ongoing treatment.
-
Ambulatory Blood Pressure Monitoring (ABPM): This 24-hour monitoring technique provides a detailed blood pressure profile throughout the day and night. It helps identify white-coat hypertension (elevated readings in clinical settings) and masked hypertension (normal readings in the clinic but high outside).
-
Routine Clinical Check-ups: Regular visits to a healthcare professional ensure the timely detection and management of hypertension. These check-ups often include blood pressure measurements, physical examinations, and lifestyle assessments.
-
Electrocardiogram (ECG) and Echocardiography: ECG measures the electrical activity of the heart, helping detect irregular heart rhythms and heart strain. Echocardiography uses ultrasound to visualise heart structures and assess its function, revealing thickening of the heart muscle and other signs of hypertensive heart disease.
More Reads: Warning Signs and Symptoms of Congestive Heart Failure
Managing and Preventing Hypertension-Related Heart Disease
Managing hypertension can significantly reduce the risk of heart disease. Key strategies include:
-
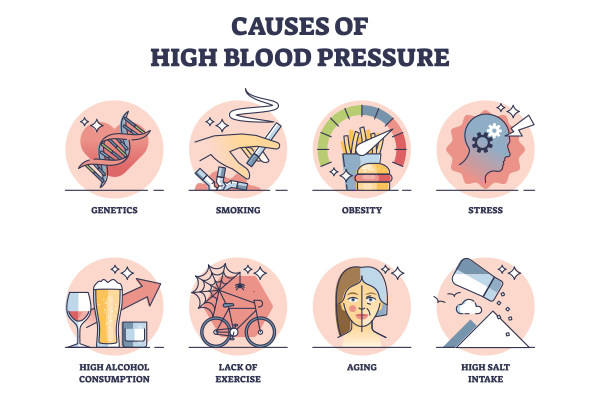
Lifestyle Changes: Healthy diet (DASH diet), regular exercise, reducing salt intake, and quitting smoking.
-
Medications: ACE inhibitors, beta-blockers, diuretics, and calcium channel blockers.
-
Regular Monitoring: Keeping a close check on blood pressure levels.
-
Stress Management: Mindfulness, yoga, and meditation can help lower blood pressure.
Conclusion
Understanding the link between hypertension and heart disease is crucial for early intervention and prevention. Regular health check-ups, a balanced lifestyle, and timely medical care can go a long way in protecting your heart health.
To learn more about managing hypertension and reducing your heart disease risk, consult the expert cardiologists at Manipal Hospitals Dwarka. With cutting-edge diagnostic technology, experienced cardiologists, and comprehensive heart care services, Manipal Hospitals Dwarka is dedicated to helping you take control of your heart health. Schedule a consultation today to take the first step towards a healthier heart.
FAQ's
While it may not be entirely reversible, effective lifestyle changes and medication can significantly control and reduce blood pressure.
Yes, genetics can play a role, but lifestyle factors also significantly influence blood pressure levels.
Regular checks are recommended, especially if you have a family history or other risk factors for heart disease.
Early signs include fatigue, shortness of breath, chest pain, and swelling in the legs or ankles.
Yes, if left untreated, chronic high blood pressure can weaken the heart and lead to heart failure over time.





















 5 Min Read
5 Min Read