Diabetes Mellitus stems from a combination of genetics and lifestyle factors. Major cornerstones of management in diabetes are:
-
Nutrition therapy
-
Physical activity
-
Blood glucose monitoring
-
Psychological wellbeing
-
Medications
Controlling blood sugar is important for avoiding diabetes-related complications such as nerve damage, kidney disease, and heart disease. You might also think that diet is the key to balancing glucose levels, as what you eat directly affects your blood sugar. But can you reverse or reduce blood sugar levels just by changing your diet alone? The relationship between diabetes and diet is complex, and while food choices play a major role in diabetes control, diet alone may not always be sufficient. Read on to explore how diet can help manage and reduce blood sugar levels.
Synopsis
- The Role of Diet in Blood Sugar Control
- Insulin Sensitivity and Diet
- The Glycemic Index (GI) Debate
- The Role of Medical Nutrition Therapy (MNT)
- Can Fasting Diets Solve the Problem?
- The Emotional Toll of Restrictive Eating
- Limits of Dietary Intervention
- The Need for Medication and Combined Therapies
- The Gut Microbiome Connection
- Conclusion
The Role of Diet in Blood Sugar Control
Every time you eat, your blood glucose levels change. The breakdown of carbohydrates, proteins, and fats affects glucose and insulin differently. Simple sugars quickly convert to glucose, causing a spike in your blood sugar. Whole grains are complex carbs, which means they take a bit longer to digest and don’t release glucose into your bloodstream that fast.
Other things to consider are fats and proteins. Proteins break down into amino acids that affect glucose minimally. Fats increase gastric emptying time and may slow carbohydrate absorption and reduce glucose spikes. It shows that your macronutrient balance has a huge impact on reducing blood sugar levels.
Carbohydrate is a readily used source of energy and the primary dietary influence on postprandial blood glucose. The quality of carbohydrate food selected should be ideally rich in fibre, vitamins, and minerals, and low in added sugars, fat, and salt.
Read our blog: How to Know If You Have Diabetes: The Symptoms, Causes and Treatment
Insulin Sensitivity and Diet
Your body’s ability to use glucose depends on insulin sensitivity and how well the body functions.
Insulin sensitivity refers to how effectively your cells respond to insulin, a hormone that facilitates glucose transport into cells, where it is utilised for energy. A state in which a normal amount of insulin produces a subnormal response is called insulin resistance.
Insulin resistance, or low sensitivity, results in your pancreas producing more insulin in attempts to overcome it, usually resulting in type 2 diabetes over time. Some of the improvements in your diet can help your insulin sensitivity. Eating a high-fibre plant-based diet is beneficial. Leafy greens and legumes are high in fibre and slow down how quickly glucose gets absorbed, making insulin work more efficiently.
Reduce your intake of saturated fats, which include animal fat, beef, pork, lamb, and chicken, high-fat dairy foods like butter, full-fat milk, and cheese, and oils such as coconut oil and palm oil. Replacing these saturated fats with monounsaturated fats may improve insulin resistance. Eating foods that are rich in omega-3 fatty acids, such as salmon and walnuts, helps reduce inflammation, which is a key driver of insulin resistance.
Poor food choices, however, are not the only cause of insulin resistance. Physical inactivity, genetics, and visceral fat accumulation are also hugely important. Staying active helps your cells react to insulin more effectively and lowers your blood sugar levels.
The Glycemic Index (GI) Debate
The Glycemic index (GI) is a ranking system for foods based on their potential to raise blood glucose levels.
Low-GI foods, such as sweet potatoes and lentils, cause gradual blood sugar rises, while high-GI foods, like white bread, lead to rapid spikes.
The Glycemic load of a food item/meal is the product of the amount of available carbohydrates and the glycemic index of the food.
Food factors that influence the glycemic response include:
-
Amount of carbohydrate
-
Nature of the carbohydrate (simple or complex)
-
Eating time
-
Pairing with other food components like fat, protein, and dietary fibre
For example, watermelon has a high GI but a low glycemic load because it contains relatively little carbohydrate per serving. Moreover, the GI of a food changes when combined with other macronutrients, making real-life applications tricky.
Instead of fixating on GI alone, focus on portion sizes, overall carbohydrate intake, and the nutrient density of your meals. Pairing carbohydrates with proteins or fats can further mitigate blood sugar spikes.
Read our blog: Diabetes in Children: Type 1 and Type 2 Diabetes - Diagnosis and Treatment
The Role of Medical Nutrition Therapy (MNT)
Medical nutrition therapy (MNT) is a process by which nutrition prescription is tailored for people based on medical, lifestyle, and personal factors and is an integral part of diabetes management.
Consulting a registered dietitian trained in MNT can significantly help if you have consistently high blood sugar. They craft an individualized plan to assess your glucose trends, dietary habits, and metabolic markers.
MNT emphasises timing and macronutrient distribution across meals. Consuming smaller, balanced meals every 3–4 hours will help prevent glucose spikes and dips. Additionally, certain micronutrients—such as magnesium, chromium, and alpha-lipoic acid—can enhance insulin action and glucose metabolism. Your dietitian can guide you on incorporating foods rich in these nutrients, such as spinach, nuts, and broccoli.
However, MNT also acknowledges that dietary changes alone are insufficient for effective blood sugar control. Medications, exercise, and behavioral therapy must complement dietary interventions for optimal results.
Can Fasting Diets Solve the Problem?
Intermittent fasting has gained popularity for its potential to improve insulin sensitivity and stabilise blood sugar. Research shows that time-restricted eating can help reduce body weight, decrease fasting glucose levels, and reduce insulin resistance.
While fasting diets are beneficial in the short term, their long-term efficacy and safety have yet to be established. Fasting can also pose risks of hypoglycemia, especially if you are taking medications for diabetes, and if the fasting durations are extreme.
The Emotional Toll of Restrictive Eating
Focusing solely on diet can take an emotional toll. Constantly counting carbs, avoiding favourite foods, or eating differently from family members can feel isolating. This emotional stress can elevate cortisol and blood sugar levels, creating a vicious cycle.
It is important to realise that a “diabetic diet” is not a complete deviation from a normal diet.
Instead of overly restrictive diets, aim for flexibility within your medical guidelines. Incorporate occasional indulgences in controlled portions. This not only sustains long-term adherence but also reduces stress, a hidden contributor to high blood sugar.
Limits of Dietary Intervention
Although diet plays a pivotal role in reducing blood sugar levels, it can’t completely counteract all challenges associated with diabetes. Type 2 diabetes is a multifactorial condition influenced by stress, sleep, genetics, and physical activity. If you only change your diet plan for diabetes, you risk ignoring these equally critical factors.
Take physical activity as an example. Exercise enhances glucose uptake by muscle cells independent of insulin. Without it, even a flawless diet for diabetes may fail to control your blood sugar effectively. Similarly, chronic stress elevates cortisol, a hormone that raises blood sugar. You can eat perfectly, but chronic stress could sabotage your progress.
This underscores a hard truth: dietary strategies, while powerful, must complement a broader lifestyle approach.
The Need for Medication and Combined Therapies
Dietary intervention helps some people in diabetes management. For some, the pancreas has already lost the ability to produce sufficient insulin. No diet can regenerate beta cells, the insulin-producing cells in your pancreas.
Medications like metformin improve insulin sensitivity and help the liver regulate glucose production. Injectable options, such as GLP-1 receptor agonists, mimic natural hormones that curb appetite and slow digestion, enhancing blood sugar control. Combining these therapies with a tailored diabetes diet often results in the best outcomes for reducing blood sugar levels and improving overall health.
For better management of blood sugar levels, consult an expert diabetes specialist near you.
The Gut Microbiome Connection
Emerging research highlights the role of the gut microbiome in blood sugar regulation. The trillions of bacteria in your intestines influence glucose metabolism, insulin sensitivity, and even inflammation.
A fibre-rich diet fosters beneficial bacteria that produce short-chain fatty acids (SCFAs). These SCFAs enhance insulin sensitivity and lower inflammation. Foods like artichokes, asparagus, and fermented products (e.g., yoghurt and kefir) can diversify your gut microbiota.
However, gut health isn’t solely determined by food. Antibiotics, stress, and insufficient sleep also impact your microbiome. If you neglect these factors, dietary efforts may fall short.
Conclusion
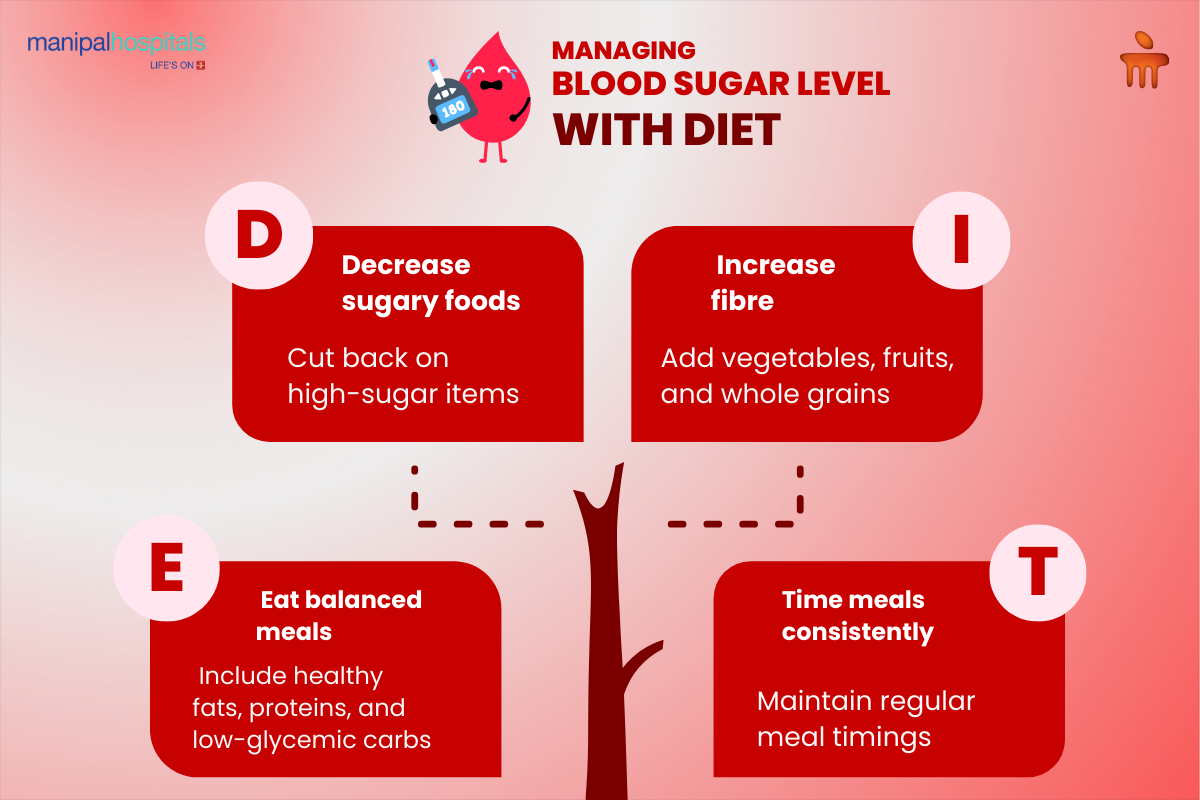
People navigating diabetes are encouraged to eat a well-designed, healthy, balanced meal in moderate amounts and stick to regular meal timings. While mindful eating can stabilise glucose levels, it must be paired with lifestyle changes like regular exercise, stress management, and adequate sleep. Medical interventions often remain necessary for effective control, especially in advanced cases. By combining these strategies, you can take a comprehensive approach to managing blood sugar, reducing risks, and improving your overall health and quality of life.
FAQ's
Intermittent fasting (IF) can improve insulin sensitivity and stabilise blood sugar levels for some individuals. However, it may not be safe for everyone, particularly those taking certain medications, as it could lead to hypoglycemia.
Fatty fish like Salmon contain Omega-3 fatty acids that can help reduce inflammation and other risk factors like heart attack and stroke.
Leafy green vegetables are extremely nutritious, and low in calories, and vitamin C-rich foods like citrus fruits and berries are potent antioxidants and have anti-inflammatory properties.
High-fibre options like legumes, whole grain cereals, and magnesium-rich choices like nuts and seeds enhance insulin sensitivity, reduce inflammation, and support glucose metabolism.
The glycemic index is useful, but should not be the sole focus. Low-GI foods can help stabilise blood sugar, but factors like portion size, nutrient density, and meal composition also play critical roles in effective glucose control.





















 8 Min Read
8 Min Read

.png)