-
Book Appointments & Health Checkup Packages
- Access Lab Reports
-
-
Book Appointments & Health Checkup Packages
-
Centre of
Excellence
Centre of Excellence
- Bariatric Surgery - MIBS
- Accident and Emergency Care
- Cardiology
- Cardiothoracic Vascular Surgery
- Diabetes and Endocrinology
- Gastrointestinal Science
- General Surgery
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Medical Gastro
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Orthopaedics
- Renal Sciences
- Spine Care
- Surgical Gastro
- Urology
Other Specialities
- Anesthesiology
- Bariatric Surgery
- Cancer Care
- Dental Medicine
- Dermatology
- Ear Nose Throat
- Fetal Medicine
- Hemato Oncology
- ICU and Critical Care
- Internal Medicine
- Interventional Radiology
- IVF and Infertility
- Laboratory Medicine
- Medical Oncology
- Microbiology
- Neonatology & NICU
- Nocturnal Dialysis
- Nutrition And Dietetics
- Ophthalmology
- Paediatric And Child Care
- Paediatric Surgery
- Pain Medicine
- Pathology
- Pharmacy
- Physiotherapy
- Plastic, Reconstructive And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Reproductive Medicine
- Rheumatology
- Sports Medicine
- Surgical Oncology
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Hebbal
-

Bengaluru

-
-

Bhubaneswar

-

Bhubaneswar
-
-

Delhi - NCR

-

Goa

-

Goa
-
-

Jaipur
-

Kolkata

-

Mangaluru
-

Mysuru
-

Patiala
-

Pune

-

Ranchi
-

Salem
-

Siliguri City

-

Vijayawada
- International Patients



Clinics







- Self Registration
- In-Patient Deposit
- Mars - Ambulance
- Home Care
- Organ Donation
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Manipal Insider
- Extended Clinical Arm
- Careers
- Contact Us

Care of premature babies
Premature babies treatment in Hebbal, Bangalore
The term "premature baby" refers to an infant born about three weeks before its due date. A baby born before the 37th week of pregnancy would be another way of putting it. As the baby cannot fully develop in the mother's womb, premature birth is dangerous for the infant. Anaemia, jaundice, and apnea are common medical complications that affect premature babies, especially those born very early. The following are some care tips for premature babies,
1. Bringing Your Newborn Home From the Hospital
It might feel daunting to start taking your premature baby care tips home when the time finally comes. It is beneficial not just for your baby but also for you as a parent, as it reduces the chances of your child contracting an infection during hospitalisation. You can also establish a stronger bond with your new family member in your home, where you can provide your infant with a positive and comfortable environment where it can feed on its own. If you are not both ready to go home with your baby, the hospital will not suggest you take her home or provide premature babies treatment in Hebbal, Bangalore. Going home from the hospital is good because your child's health has stabilised.
2. Breastfeeding Your Premature Baby
It is essential for every mother to breastfeed, regardless of the circumstances. Your premature baby will grow and develop faster and healthier if you breastfeed, as breast milk contains specific vitamins and nutrients. Since your body specially designs breast milk for your baby, it is easier to digest than formula milk. You should express your milk eight to ten times a day and once at night if your infant is too premature for breastfeeding. If you've never squeezed milk before, a nurse or midwife can demonstrate how to do it. Additionally, your hospital or another source may be able to provide the donor's breast milk.
3. Keep your premature baby in skin-to-skin contact.
As well as the mother and baby, the father has found this to be a great exercise. You can practice skin-to-skin contact with your infant by dressing them in a nappy and letting them rest on your chest underneath your shirt or blanket so they are tightly attached. Communication with your child's skin has many benefits, including reducing pain and stress. Furthermore, it promotes healthy weight gain, assists in breastfeeding, makes your baby more adaptable to its new surroundings, and regulates its heart rate and breathing.
4. Don't forget to pay attention to your baby's sleeping needs
Sleeping throughout the day is normal for preterm babies since it aids their growth and development. Here are a few tips to ensure your baby is sleeping well: keep them on a hard, flat surface without any pillows, and always let them sleep on their back.
5. Limit outdoor visits
You should ensure that your baby stays at home for the first few weeks after birth. The exception is doctor's appointments, which you should attend regularly. We ask you to keep your baby at home most of the time because his immunity is deficient, making them susceptible to infections and viruses. In the first few months of your baby's life, they should be kept in a safe environment.
7. Care of sick newborns
Here are some steps you can follow to care for your ill newborns.
General Management Care
Transferring a neonate to a neonatal unit requires stabilising the neonate first:
-
To open the airway, position the head in a forward position.
-
Using a nasal cannula, administer oxygen at a maximum flow rate of 2 litres/minute (aiming for 90-95% SpO2).
-
Ventilate the patient using a mask and a bag in cases of apnoea or RR over 20/minutes
-
Checking blood glucose levels can treat hypoglycemia.
-
During the waiting period for transfer:
-
Keeping the neonate warm in a room between 23 and 25°C with a blanket or under a hospitable infant is essential.
-
Monitor temperature, respiratory rate, and oxygen saturation closely.
-
Start neonatal infection treatment.
-
Ensure to provide routine neonatal care. Start or continue feeding the newborn. Ensure that nasogastric tubes and IV fluids are supplemented with feeds only if necessary.
Do not feed the neonate by mouth if they have severe respiratory distress, abdominal distension, or are in a coma. If possible, start fluids.
Neonatal Infection
Severe neonatal infections are suspected in neonates. There is a possibility that underlying signs of danger may indicate a painful condition requiring antibiotic therapy and transfer to a neonatal unit.
In preparation for transfer to a neonatal unit, start antibiotic therapy as follows,
-
In the first instance, ampicillin IV combined with gentamicin IM is an excellent treatment of choice.
-
In circumstances where ampicillin IV administration is not feasible, administer ampicillin intramuscularly.
-
To avoid multiple IM injections, procaine benzylpenicillin and gentamicin injection may be a better option.
-
Avoid using procaine benzylpenicillin if you suspect meningitis.
-
Replace ampicillin with cloxacillin IV if the infection is cutaneous.
-
The total treatment duration is 7 to 10 days depending on the clinical response. After five days of treatment, You can stop gentamicin.
Hypoglycemia
Various neonates' hypoglycemia is asymptomatic. Recurrent or persistent hypoglycemia can have neurological consequences.
Diagnosis
The blood glucose level should be 2.5 mmol/l or 45 mg/dl.
With a lancet or 24G needle, capillary blood is sampled from the side of the heel to determine blood glucose levels.
Perform a clinical examination and assessment of risk factors in neonates at risk of hypoglycemia
The following signs may be present in neonates,
-
Hypothermia
-
Seizures
-
Dyspnea, apnea, or cyanosis
-
Insomnia, hypotonia, or impaired consciousness
-
Irritability or tremors
Management
For asymptomatic hypoglycemia of 35 to 44 mg/dl (2 to 2.4 mmol/litre)
-
Feed the neonate immediately (preferably with breast milk).
-
If milk is unavailable, give 5 to 10 ml of 10% glucose PO over a few minutes if no milk is available.
-
After 30 minutes, check blood glucose:
-
When expected (2.5 mmol/litre or 45 mg/dl), ensure the neonate eats regularly and checks his blood sugar before every meal.
-
Treat recurrent hypoglycemia if it remains over 2.5 mmol/litre or 45 mg/dl.
For severe hypoglycaemia (2-4 mmol/L or 35 mg/L) or recurring symptoms
-
If an IV line is already in place, provide 2 ml/kg of 10% glucose slow IV over 5 to 10 minutes or 5 ml/kg of 10% glucose PO over 5 to 10 minutes. After 30 minutes, check blood glucose levels:
-
Feed the neonate regularly, and check the blood glucose after 30 minutes and before each feed until the result is three consecutively every day.
-
The neonate should be transferred to a neonatal unit if the blood glucose is more than 2.5 mmol/litre or 45 mg/dl or if symptoms persist. Maintain a constant infusion of 10% glucose (80 ml/kg/24 hours) while awaiting transfer and monitor blood glucose levels.
Book an appointment at Manipal Hospitals now.
Home Hebbal Specialities Neonatology-nicu Care-of-premature-babies

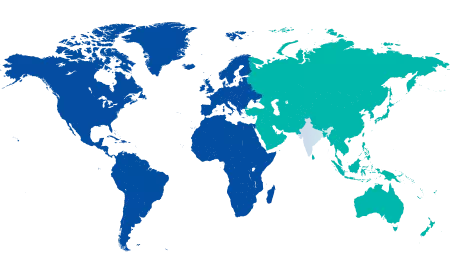
You’re on Our Indian Website
Visit the Global site for International patient services





