Vaginal health plays a significant role in a woman’s overall well-being. Sexually transmitted infection (STI) affects both vaginal health and overall well-being. Different health conditions share overlapping symptoms, but each has its origins and distinct health risks, leading to other long-term outcomes. A top gynaecologist in Hebbal, Bangalore, discusses the difference between vaginal infections and STIs, while highlighting the importance of awareness about HPV infections, vaccination, and regular screenings.
Synopsis
Vaginal Infections vs STIs: What’s the Difference?
Most vaginal infections cause itching or burning and unusual discharge; many of these infections are STIs. But, probably the most sinister ones do not cause any of these symptoms
.png)
Let’s explore the differences between the two in more detail:
-
Vaginal Infections Are Almost Always Sexually Transmitted: However, the microbial disorders causing yeast may be caused by underlying diabetes.
-
STIs Are Transmitted Through Sexual Contact: Sexual Intercourse transmits STIs, such as Chlamydia, Gonorrhoea, Syphilis, and HPV, which require various treatment methods.
-
Overlapping Symptoms Can Confuse Patients: Itching, burning, and unusual discharge are common to both, but STIs may also bring systemic symptoms or longer-term complications.
-
Vaginal Infections Often Respond to Simple Treatment: Most vaginal infections clear up with antifungal or antibiotic medication, often without lasting damage.
-
STIs May Cause Lasting Harm if Left Untreated: Some STIs can result in infertility, chronic pelvic pain, or increased cancer risk if undetected.
How Does HPV Spread?
HPV is one of the most widespread STIs in the world. What makes it uniquely dangerous is that most infections do not present with symptoms, yet it can lead to severe complications like cervical cancer.
Understanding its transmission is crucial for prevention:
-
Skin-to-Skin or Mucosal Contact Is Enough: Unlike many STIs, HPV doesn’t always require penetration. It can spread through genital, oral, or anal linings.
-
Condoms Offer Partial Protection: While condoms reduce the risk, they do not eliminate the chance of HPV transmission. However, they may help the body clear the infection faster.
-
The Virus Can Persist for Years: Many infected individuals are unaware and may carry the virus unknowingly, increasing community-level risk.
How to Diagnose HPV?
HPV often shows no symptoms, making regular screenings essential, especially for sexually active women. An expert OBG specialist in Bangalore may recommend the following diagnostic tests:
-
PAP Smear (Papanicolaou Test): This screening checks for abnormal cervical cells that could indicate precancerous changes caused by high-risk HPV strains.
-
HPV DNA Test: Often done with or following a PAP smear, this test detects the presence of high-risk HPV serotypes in cervical cells.
-
Colposcopy: If a PAP smear result is abnormal, doctors may perform a colposcopy - a magnified visual exam of the cervix—to look for abnormal tissue.
-
Biopsy: In cases where abnormal areas are detected, a biopsy may be done to determine whether pre-cancer or cancer is present.
The Role of the HPV Vaccine
HPV infection is so common that over 80% of sexually active adults are expected to contract it at least once in their lifetime. However, vaccination offers a powerful shield against the high-risk strains that can cause cervical and other cancers. Here’s why the HPV vaccine is a game-changer:
-
It Prevents the Most Dangerous HPV Strains: Vaccines like Gardasil and Cervarix protect against high-risk HPV types 16 and 18, which are responsible for the majority of cervical cancer cases.
-
Vaccination Works Best When Given Early: Girls can be vaccinated as early as 9. It is most effective when given before any sexual activity begins.
-
Catch-Up Vaccination Is Still Valuable: The vaccine is beneficial for women up to age 40. Even those previously exposed to HPV may gain protection from other strains.
-
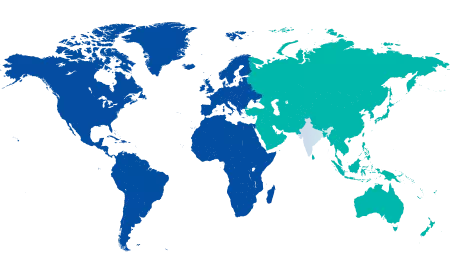
Promising Global Impact on HPV-Related Disease: Countries with widespread HPV vaccination programs have already seen significant declines in HPV-related diseases, including cervical cancer.
Conclusion
Understanding the difference between common vaginal infections and serious STIs like HPV is crucial for every woman. While both types of infections can share symptoms, HPV remains especially concerning because of its silent nature and strong link to cancer. But there is hope - early screening, safe practices, and the HPV vaccine can drastically reduce the burden of the disease. Raising awareness, encouraging open conversations, and supporting preventive healthcare can make a life-saving difference. Visit the Gynaecology Department at Manipal Hospital, Hebbal, Bangalore, for expert treatment.
FAQ's
Yes, HPV can be transmitted through skin-to-skin contact, which condoms may not entirely prevent.
Most high-risk HPV infections have no symptoms. Low-risk types may cause genital warts.
Women aged 21 to 65 should get screened every 3 to 5 years, depending on test type and risk factors.
There is no cure for the virus itself, but the immune system usually clears it naturally. Regular screening helps manage complications.
Yes. The HPV vaccine is proven safe and effective, and millions of doses have been administered globally under medical guidelines.





















 4 Min Read
4 Min Read