Fistula is a prevalent medical problem that afflicts a large number of people around the world. It is characterised as an abnormal opening or connection between two areas, two organs or an organ and the skin that ordinarily do not have any communication. Fistulas can occur in many parts of the body, but are often found in the digestive and urinary system. An anal fistula, for example, is a common occurrence that often occurs after draining an abscess around the anus. Symptoms associated with an anal fistula may include bleeding, discharge or drainage, pain, and changes in bowel habits.
Synopsis
What Is an Anal Fistula?
An anal fistula is an abnormal passage that connects the lining of the anal canal or rectum to the skin adjacent to the anus, resembling a tunnel. An anal fistula is a chronic medical condition and requires some kind of medical intervention. Generally, an anal fistula develops following an infection that never properly resolves. This lack of resolution leads to chronic areas of tissue abnormality manifested as a fistula and ongoing symptoms.

Key Characteristics of an Anal Fistula
-
Definition - a narrow, non-natural channel between the anal canal and skin surrounding the anus, resulting (sometimes) from a poorly constructed fistulotomy.
-
Chronic - Fistulas as a whole rarely spontaneously heal: if left untreated, anal fistulas may last for months or years.
-
Symptoms - Yorkshire practical elements include pus or foul-smelling material, pain on a bowel movement, and swelling or irritation near the anus.
Causes of Anal Fistulas
-
Infection and Abscess: Infection of an anal gland leads to an abscess (a pus-filled pocket). An abscess that is not completely drained can create a fistula tract.
-
Chronic Conditions: Chronic conditions, like Crohn’s disease, which causes inflammation in the digestive tract, greatly increase the risk of developing a fistula.
-
Other: Also, while rare, fistulas can occur due to infections (such as tuberculosis), trauma to the anal area, and complications from previous surgery.
How Fistulas Differ from Haemorrhoids and Fissures
Anal fistulas are often confused with other conditions, but they have distinct features. Some of them are as mentioned below:
|
Condition |
Description |
Key Differences from Fistula |
|
Anal Fistula |
Tunnel between the anal canal and the skin. |
Involves an infected tract, chronic discharge, and pain. |
|
Hemorrhoids |
Swollen veins in or around the anus. |
Causes itching or bleeding, no tunnel or infection. |
|
Anal Fissure |
Small tear in the anal lining. |
Results from trauma, causes sharp pain, no fistula tract. |
Understanding these distinctions is crucial, as misdiagnosing a fistula as a haemorrhoid or fissure can delay proper treatment, worsening symptoms and complications. Early consultation with a healthcare professional is essential for accurate diagnosis and effective management.
What Causes a Fistula in the Anus?
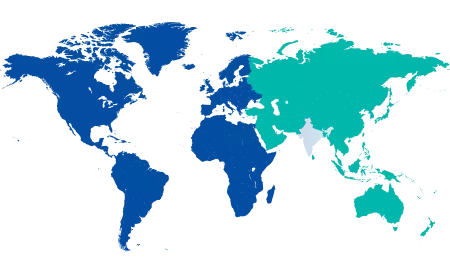
Anal fistulas form when an unusual tunnel is established between the inner lining of the anal canal and the skin surrounding the anus, often from an underlying infection or inflammatory, related condition. It is common globally, affecting many tens of thousands of people in the world, and, post-operatively, it has been estimated that it will appear in about 1 out of every 10,000 people each year (higher for people with risk factors or other health issues).
To understand causes is important not only for prevention but is also important for the treatment of anal fistulas, as acting early can help to prevent additional complications, e.g., recurrent abscesses. This piece of writing will discuss some of the more common causes and risk factors in detail below.
|
Cause Category |
Primary Trigger |
Prevalence/Impact |
Prevention Tips |
|
Infection-Related |
Clogged anal glands leading to an abscess. |
Most common (up to 90%). |
Maintain good hygiene; treat abscesses promptly. |
|
Inflammatory |
Crohn's disease or IBD. |
20-30% in affected patients. |
Manage IBD with medication; regular check-ups |
|
Infectious/Traumatic |
Tuberculosis or physical trauma. |
Rare (5-10%) |
Avoid trauma; screen for TB in high-risk areas. |
|
Systemic |
Diabetes or immunosuppression. |
Variable, higher in diabetics. |
Control blood sugar; boost immune health. |
Recognising Symptoms of an Anal Fistula
Anal fistulas present distinct symptoms that can significantly affect quality of life. Early recognition is crucial for timely diagnosis and treatment to prevent complications.
Common Signs
-
Pus or Discharge: Persistent pus or foul-smelling drainage from an external opening near the anus is a hallmark symptom. This discharge may be intermittent or constant and can stain clothing.
-
Pain or Swelling: Discomfort, often worsening during bowel movements or sitting, accompanied by swelling or a palpable lump in the anal region.
-
Skin Irritation and Redness: The constant drainage can cause itching, redness, or irritation of the skin surrounding the anus, leading to discomfort.
-
Frequent Abscesses: Recurring abscesses or boils near the anus, which may temporarily resolve but reappear, indicate an underlying fistula.
-
Fever or Malaise: In cases of infection, low-grade fever or a general feeling of unwellness may accompany other symptoms.
-
Changes in Bowel Habits: Some patients experience altered bowel movements, such as difficulty passing stool or a sensation of incomplete evacuation.
Types of Anal Fistula
Anal fistulas are classified based on their anatomical path relative to the anal sphincter muscles, which impacts treatment complexity. Understanding these types helps in planning effective interventions.

|
Type |
Description |
Prevalence |
Treatment Complexity |
|
Intersphincteric |
Runs between the internal and external sphincter muscles, within the anal canal. |
Most common (70%). |
Simple, often fistulotomy. |
|
Transsphincteric |
Crosses both internal and external sphincter muscles, involving deeper tissue. |
Common (25%). |
Moderate, may require seton. |
|
Suprasphincteric |
Extends above the sphincter muscles, looping over the external sphincter. |
Rare (5%). |
Complex, specialized surgery. |
|
Extrasphincteric |
Bypasses sphincters entirely, connecting the rectum directly to the skin. |
Very rare (<1%). |
Highly complex, advanced procedures. |
How Is a Fistula Diagnosed?
Fistula can be diagnosed using both clinical evaluation and by conducting some imaging tests. If you want to choose the former, you can choose from the two options: digital rectal exam, where the doctor checks the anal section to check for some abnormalities or tenderness, or your medical history can also help in diagnosing a fistula.
If you want to choose the latter, you can be advised to go for an ultrasound or MRI, where detailed images of the fistula can be used to make the diagnosis, or you have the option to do fistulography, where experts perform an X-ray with contrast dye to trace the fistula tract. One of the more advanced ways of treatment is via endoanal ultrasound, which offers more precise mapping of the tunnel for complex fistulas.
Treatment Options for Anal Fistula
The treatment for an anal fistula depends on the location and severity of the condition. In some cases, the anal fistula may heal on its own, but in most cases, medical intervention is required. Treatment options include medication, surgery, or a combination of both. Antibiotics may be prescribed to treat any infection that is present, while medications may be given to reduce inflammation and pain. Surgery is often necessary as an anal fistula generally does not heal on its own. Surgery is also recommended when an anal fistula causes significant discomfort or other health problems. Treatment procedures at a gastroenterology hospital in Sarjapur Road include the removal of infected tissue and anal fistula closure and repair. The type of surgery usually depends on the location of the anal fistula.
Most anal fistulas are easily treated by laying them open; the procedure is called fistulotomy. The muscle around the anus is protected during a fistulotomy to avoid incontinence. Other than that, more advanced procedures such as ligation of the intersphincteric anal fistula tract (LIFT), and advancement flaps are well-known surgical procedures that are often used to treat cases of anal fistula. Seton, which is a rubber band or thread, is placed in an anal fistula tract to help prevent progression to abscesses or recurrent infection. The seton is often left in the anal fistula for several weeks to keep it open, which allows it to drain and helps it heal.
A laser is a colloquial term for a specific energy source. Lasers, though not proven, have been popularised by commercial enterprises. However, it is not recommended for treating anal fistulas by major colorectal societies, such as the American Society of Colon and Rectal Surgeons.
It is recommended that you consult the best gastroenterologist at Manipal Hospitals, Sarjapur Road, if you have anal fistula or similar symptoms. Early detection will aid in determining the underlying cause of the condition and recommending the best course of treatment. Recovery time and post-surgical care will also vary depending on the type of surgery performed. Hence, additional procedures or treatments may be necessary to fully treat the condition. Though it is important to note that the best treatment for an anal fistula will depend on the individual case, and the treatment plan may be different for each patient.
Comparison: Fistulotomy vs. Seton Placement
|
Feature. |
Fistulotomy. |
Seton Placement. |
|
Procedure Type. |
Surgical cut of the fistula. |
The thread is placed for drainage. |
|
Recovery Time. |
1–2 weeks. |
May require multiple visits. |
|
Best For. |
Simple fistulas. |
Complex fistulas. |
|
Risk of Incontinence. |
Low for superficial fistulas. |
Lower for deep fistulas. |
Conclusion
Book an appointment in Manipal Hospitals Sarjapur Road or visit our Gastrointestinal Science department today!
FAQ's
Most anal fistulas require minor surgical intervention for complete healing, as spontaneous resolution is rare.
A fistula is an infected tunnel connecting the anal canal to the skin, while haemorrhoids are swollen veins in the anal region.
Surgery is performed under anaesthesia, and post-operative discomfort is typically mild and manageable.
Recurrence is uncommon with proper treatment but can occur in complex cases or if post-surgical care is inadequate.





















 7 Min Read
7 Min Read