Fatty Liver Disease is increasingly being diagnosed across all age groups, often silently and incidentally during routine health checks. While many people live with the condition for years without major complications, a small proportion progress to severe liver damage, where a liver transplant becomes the only life‑saving option. Understanding when fatty liver disease becomes dangerous and when a transplant is required can help patients seek timely care and prevent irreversible damage.
At Manipal Hospital Baner, liver specialists focus strongly on early diagnosis, lifestyle-based treatment, and advanced hepatology care to help patients avoid end-stage liver disease wherever possible.
Synopsis
- What Is Fatty Liver Disease?
- Fatty Liver Disease Causes
- Fatty Liver Disease Symptoms
- Stages of Fatty Liver Disease
- Fatty Liver Disease Treatments
- When Is a Liver Transplant Required?
- Life After a Liver Transplant
- Can Fatty Liver Disease Be Prevented From Reaching Transplant Stage?
- Short Patient Story
What Is Fatty Liver Disease?
Fatty Liver Disease occurs when excess fat accumulates in liver cells, making up more than 5–10% of the liver’s weight. This fat build-up interferes with normal liver function and, over time, can cause inflammation, scarring, and liver failure.
There are two main types:
-
Alcoholic Fatty Liver Disease (AFLD) – caused by excessive alcohol consumption
-
Non-Alcoholic Fatty Liver Disease (NAFLD) – linked to obesity, diabetes, high cholesterol, and metabolic syndrome
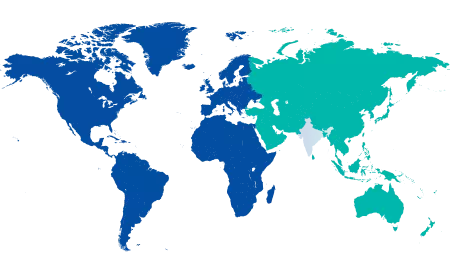
NAFLD is now one of the leading causes of chronic liver disease worldwide.
Fatty Liver Disease Causes
Several lifestyle and medical factors contribute to fatty liver disease, including:

-
Obesity and abdominal fat
-
Type 2 diabetes or insulin resistance
-
High cholesterol or triglycerides
-
Sedentary lifestyle
-
Excessive alcohol intake
-
Rapid weight loss or poor nutrition
-
Certain medications (steroids, chemotherapy drugs)
In many cases, a combination of these factors accelerates disease progression.
Fatty Liver Disease Symptoms
In its early stages, fatty liver disease symptoms are often mild or absent. As the condition worsens, symptoms may include:
-
Persistent fatigue
-
Discomfort or pain in the upper right abdomen
-
Loss of appetite
In advanced stages, symptoms of liver failure appear:
-
Yellowing of skin and eyes (jaundice)
-
Swelling of the abdomen (ascites)
-
Swollen legs and feet
-
Easy bruising or bleeding
-
Mental confusion (hepatic encephalopathy)
These signs indicate urgent medical attention is required.
Stages of Fatty Liver Disease
Understanding disease stages helps clarify when a transplant may be needed:
-
Simple Fatty Liver (Steatosis) – Fat accumulation without inflammation
-
Steatohepatitis (NASH/ASH) – Fat with inflammation and liver cell injury
-
Fibrosis – Formation of scar tissue
-
Cirrhosis – Extensive scarring leading to permanent liver damage
-
End-Stage Liver Disease – The liver can no longer perform vital functions
A liver transplant is considered only in the final stages.
Fatty Liver Disease Treatments
Most patients can manage fatty liver disease effectively without surgery. Fatty liver disease treatments focus on reversing liver fat and preventing progression:
-
Gradual weight loss (7–10% of body weight)
-
Balanced, liver-friendly diet
-
Regular physical activity
-
Strict control of blood sugar and cholesterol
-
Complete avoidance of alcohol
-
Treating associated conditions such as hypertension
At Manipal Hospital Baner, personalised treatment plans are designed by hepatologists, dietitians, and endocrinologists working together.
When Is a Liver Transplant Required?
A liver transplant is required only when fatty liver disease progresses to irreversible liver failure, and no other treatment options remain.
Common indications include:
-
Decompensated cirrhosis (fluid accumulation, bleeding, confusion)
-
Recurrent hospitalisations due to liver complications
-
Liver cancer arising from cirrhosis (Hepatocellular carcinoma)
-
Poor quality of life due to severe symptoms
-
High MELD score (Model for End-Stage Liver Disease)
Doctors assess transplant eligibility through blood tests, imaging, heart and lung evaluations, and overall health status.
Life After a Liver Transplant
A transplant can be life-changing, but long-term success depends on commitment to healthy living:
-
Lifelong immunosuppressive medications
-
Regular follow-ups and blood tests
-
Healthy diet and weight maintenance
-
Strict avoidance of alcohol
-
Management of diabetes and cholesterol
Patients who follow medical advice often return to an active and fulfilling life.
Can Fatty Liver Disease Be Prevented From Reaching Transplant Stage?
Yes, Early detection and lifestyle changes are extremely effective. Regular health check-ups, ultrasound screening, and blood tests help identify fatty liver disease before complications arise.
Seeking expert care at centres like Manipal Hospital Baner ensures access to advanced diagnostics, early intervention, and transplant evaluation if needed.
Short Patient Story
A Journey Back to Health
Mr Ramesh (name changed), a 52-year-old IT professional from Pune, was diagnosed with Fatty Liver Disease during a routine health check-up. Initially asymptomatic, his condition worsened over the years due to unmanaged diabetes and a sedentary lifestyle. When he developed abdominal swelling and extreme fatigue, further tests revealed advanced cirrhosis.
Under the care of the liver specialists at Manipal Hospital Baner, Mr Ramesh underwent a comprehensive evaluation and was placed on an intensive medical and lifestyle management plan. Although his liver damage could not be reversed completely, timely intervention stabilised his condition and improved his quality of life. Today, he continues regular follow-ups, adheres to dietary guidance, and remains active, highlighting how early diagnosis and expert care can make a significant difference.
FAQ's
No. Most people with fatty liver disease never require a transplant. Early-stage disease can often be reversed with lifestyle changes and medical management.
Doctors assess liver function, symptoms, complications, imaging results, and MELD score to determine whether transplantation is required.
Yes, if unhealthy lifestyle habits continue. Maintaining a healthy weight, avoiding alcohol, and controlling diabetes are essential after a transplant.
Early stages are usually not life-threatening. However, advanced cirrhosis and liver failure can be fatal without timely treatment or transplant.
Patients should follow their doctor’s advice, but regular blood tests and imaging every 6–12 months are commonly recommended.






















 5 Min Read
5 Min Read