-
Book Appointments &
Health Checkup Packages - Access Lab Reports
-
-
Book Appointments & Health Checkup Packages
-
Centre of
Excellence
Centre of Excellence
- Robotic Spine - MIRSS
- Joint Replacement and Robotic Surgery - MIJRRS
- Bariatric Surgery - MIBS
- Head and Neck - MIHNS
- Children's Airway & Swallowing Centre - CASC
- Manipal Hearing and Implant Institute - MHII
- Manipal Skull Base Institute - MSBI
- Accident and Emergency Care
- Bone Marrow Transplantation
- Cancer Care
- Cardiology
- Cardiothoracic Vascular Surgery
- Clinical Hematology and Hemato Oncology
- Gastrointestinal Science
- Liver Transplantation Surgery
- Neonatology & NICU
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Paediatric Intensive Care Unit
- Spine Care
- Urology
Other Specialities
- Anesthesiology
- Bariatric Surgery
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- ENT- Head & Neck Surgery
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- Growth and Hormone
- Hand Surgery
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- IVF and Infertility
- Laboratory Medicine
- Microbiology
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Paediatric Endocrinology
- Paediatric Infectious Disease
- Paediatric Neurology
- Pain Medicine
- Pathology
- Pharmacy
- Physical Medicine and Rehabilitation
- Plastic, Cosmetic and Reconstructive Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Reproductive Medicine
- Rheumatology
- Robotic Assisted Surgery
- Sports Medicine
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Old Airport Road
-

Bengaluru

-
-

Bhubaneswar

-

Bhubaneswar
-
-

Delhi - NCR

-

Goa

-

Goa
-
-

Jaipur
-

Kolkata

-

Mangaluru
-

Mysuru
-

Patiala
-

Pune

-

Ranchi
-

Salem
-

Siliguri City

-

Vijayawada
- International Patients



Clinics









Angioedema Clinic
Best Hospital For Angioedema in Old Airport Road, Bangalore
Angioedema is a very common disorder that causes localized swelling beneath the skin or mucous membranes. It is broadly categorized into mast cell mediator-mediated angioedema (commonly known as allergic angioedema) and bradykinin-mediated angioedema. Mast cell mediator-mediated angioedema is the most common form and is seen in up to 5% of the population, often accompanied by urticaria or hives. Managing angioedema needs a comprehensive and multidisciplinary approach involving immunologists, dermatologists, and emergency physicians. While there is no known cure for patients with hereditary angioedema, an individualized management plan can improve the quality of life of patients and prevent mortality. For allergic angioedema, various potential treatments offer excellent results, greatly improving patient well-being.

OUR STORY
Know About Us
Why Manipal?
The Angioedema Clinic at Manipal Hospital Old Airport Road, Bangalore, is the first-of-its-kind clinic in India to provide a ‘state-of-the-art’ facility in the diagnosis and management of different forms of angioedema.
Angioedema is a chronic disease that needs regular follow-up. Our expert team includes experts from the fields of Paediatric Immunology, Adult Immunology, Dermatology, and Emergency services with a collective aim to provide high-quality, specialised care for children suffering from angioedema and their families.
Our experts also collaborate with international experts on angioedema, who provide valuable guidance. Consult our specialists in Bangalore if you need treatment for angioedema.
.png)
What is Angioedema?
Angioedema is characterised by recurrent, localised swelling of the subcutaneous and/or submucosal tissues. This common chronic disorder is broadly classified into 2 major types: Mast Cell Mediator-Mediated Angioedema (often called allergic angioedema) and Bradykinin-Mediated Angioedema.
-
Mast cell mediator-mediated angioedema is the more prevalent form, affecting up to 5% of the population, and is frequently accompanied by urticaria (hives) in 90% of cases.
-
Bradykinin-mediated angioedema is further divided into hereditary and acquired forms.
-
Hereditary angioedema (HAE) is a rare, life-threatening genetic condition. It is most commonly caused by a defect in the SERPING1 gene. This can lead to a deficiency or dysfunction of C1-esterase inhibitor protein in the blood.
-
Acquired angioedema (AAE) involves an acquired deficiency of C1-inhibitor protein. It commonly manifests in individuals in their 40s and 50s and is often associated with lymphoproliferative disorders like lymphoma or monoclonal gammopathy or autoimmune diseases such as systemic lupus erythematosus (SLE).
How Common is Angioedema?
-
Allergic angioedema is very common and may be seen in up to 5% of the population.
-
Hereditary angioedema has a prevalence of 1:10,000 to 1:50,000 population. Considering this prevalence, it is expected that there are approximately 27,000 to 135,000 patients with hereditary angioedema in India.
-
Acquired angioedema is approximately 10 times less common than hereditary angioedema.
Signs and Symptoms of Allergic Angioedema:
-
Recurrent swelling episodes, most commonly located over face, eyes, lips, hands and feet
-
Urticaria or hives or wheals, associated with itching
-
Other allergic manifestations
Signs and Symptoms of Hereditary Angioedema:
-
History of recurrent swelling of the skin (extremities, face, and genitals)
-
Positive family history (in approximately 80%)
-
Onset of symptoms in childhood/adolescence
-
Recurrent and painful abdominal symptoms (at times, this is the only symptom)
-
Occurrence of upper airway edema (may lead to asphyxiation and death)
-
Failure to respond to anti-histamines, glucocorticoids, epinephrine, or omalizumab
-
Presence of a prodrome (that appears a few hours before the onset of swelling)
-
Absence of urticaria/wheals/hives
Signs and Symptoms of Acquired Angioedema:
-
History of recurrent swelling of the skin (extremities, face, and genitals)
-
No family history
-
Onset of symptoms in the 40s and 50s
-
Recurrent and painful abdominal symptoms
-
Occurrence of upper airway edema (may lead to asphyxiation and death)
-
Failure to respond to anti-histamines, glucocorticoids, epinephrine, or omalizumab
-
Absence of urticaria/wheals/hives
-
Signs and symptoms of underlying disease, such as autoimmune disease or malignancy
Angioedema Management:
Management of Allergic Angioedema
Allergic angioedema is usually managed using antihistamines (such as levocetirizine, fexofenadine, bilastine, and hydroxyzine) and/or omalizumab.
Management of Hereditary Angioedema:
It involves three key principles:
1. Treatment of Acute Attacks (i.e., On-Demand Therapy):
On-demand therapy focuses on addressing acute attacks to alleviate symptoms and minimise their impact. The drugs that are used for on-demand therapy are plasma-derived C1 inhibitor (C1 INH) concentrate, Icatibant, Ecallantide, and fresh frozen plasma (FFP).
2. Short-Term Prophylaxis:
Short-term prophylaxis is implemented in situations where there is a predictable risk of developing life-threatening laryngeal oedema, commonly occurring during major surgeries or dental procedures. Plasma-derived C1-INH concentrate is the best possible option for STP.
3. Long-Term Prophylaxis:
Long-term prophylaxis includes the administration of drugs continuously to prevent the development of attacks or to reduce their severity. This approach is particularly suitable for individuals with frequent and debilitating episodes. Drugs used for LTP include Tranexamic Acid, attenuated Androgens such as stanozolol and danazol, plasma-derived C1 inhibitor concentrate and lanadelumab.
Other General Measures:
Identification of potential triggers and counselling to avoid them is essential for patients with HAE. ACE inhibitors and oestrogen-containing pills must be avoided in all patients with HAE.
Management of Acquired Angioedema:
The principles of management of acquired angioedema are similar to hereditary angioedema. However, at times, drugs are used to treat the underlying diseases, such as autoimmune diseases and malignancies. These drugs include immunosuppressive medications, such as corticosteroids, mycophenolate mofetil, rituximab, and chemotherapy.
FAQ's
To book an appointment with a Angioedema Clinic expert at Manipal Hospitals Old Airport Road - Bengaluru, please call 1800 102 5555. Our dedicated team will assist you in scheduling a convenient consultation.
The Angioedema Clinic department is led by highly qualified specialists, including:
For your initial consultation at Manipal Hospitals Old Airport Road - Bengaluru, please bring:
- Medical Records – Previous reports, imaging scans, and lab results.
- Medication List – Details of current and past prescriptions.
- Insurance Details – Health insurance card and referral documents (if applicable).
- Personal ID Proof – For registration purposes.
Providing these documents will help our specialists ensure a comprehensive diagnosis and personalized treatment plan.
Manipal Hospitals Old Airport Road - Bengaluru is a preferred choice for Angioedema Clinic due to:
- Highly experienced specialists.
- State-of-the-art medical infrastructure.
- Comprehensive treatment plans with a multidisciplinary approach.
- Advanced diagnostic & surgical facilities.
- Patient-centric care with personalized treatment options.
We are committed to providing world-class healthcare with compassionate service.
The Angioedema Clinic at Manipal Hospital Old Airport Road, Bangalore, is the first-of-its-kind clinic in India to provide a ‘state-of-the-art’ facility in the diagnosis and management of different forms of angioedema.
Angioedema is a chronic disease that needs regular follow-up. Our expert team includes experts from the fields of Paediatric Immunology, Adult Immunology, Dermatology, and Emergency services with a collective aim to provide high-quality, specialised care for children suffering from angioedema and their families.
Our experts also collaborate with international experts on angioedema, who provide valuable guidance. Consult our specialists in Bangalore if you need treatment for angioedema.
Explore Stories
.jpg)
Could Your Child’s Leg…
Just Growing Pains or Something More Sinister. Frequent leg pain in children is often just growing pains, nothing to worry about unless it affects their growth, sleep or daily routine. But when other…
_(2).jpg)
Childhood Autoimmune Diseases…
Autoimmune rheumatic diseases like juvenile arthritis and systemic lupus erythematosus (SLE) can affect children’s joints, skin, kidneys, and more. In this informative video, Dr. Ankur Kumar Jindal, Consultant…
_(1).jpg)
Understanding Angioedema…
Angioedema is a condition marked by sudden, severe swelling beneath the skin and mucous membranes. In this video, Dr. Ankur Kumar Jindal, Consultant - Pediatric Clinical Immunology & Rheumatology, Manipal…
Home Oldairportroad Specialities Angioedema-clinic

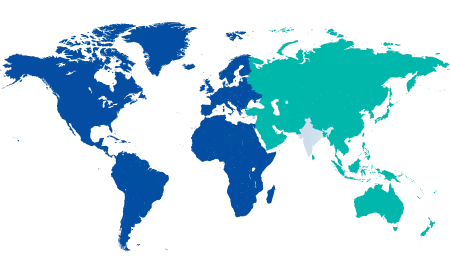
You’re on Our Indian Website
Visit the Global site for International patient services





