A hysterectomy is a surgical procedure to remove the uterus. It is performed as a treatment option for conditions like fibroids, endometriosis, or certain gynaecological cancers. In a robot-assisted hysterectomy, the surgeon uses a robotic system to perform the operation through small keyhole incisions. The robot is completely operated by the surgeon, and it mirrors the surgeon’s hand movements in real-time. It can perform very minute movements with great dexterity to perform procedures with the least amount of disturbance to the surrounding tissue. This method allows for highly accurate dissection and suturing, especially when the uterus is enlarged or scar tissue is present. It’s a safe, effective option that often results in faster recovery and less discomfort.
Synopsis
What Is Robot-Assisted Hysterectomy?
As mentioned earlier, the robot-assisted hysterectomy is a type of minimally invasive surgery. In the procedure, the uterus is removed using robotic instruments controlled by the operating surgeon. It may sound futuristic, but the technology has been used safely for many years and offers a high degree of control and success rates during the operation.
Here’s what typically happens during the procedure:
-
Anaesthesia and Setup: The patient is given general anaesthesia. Once asleep, the surgical team positions the body and prepares the abdomen for access.
-
Incision and Port Placement: Several small keyhole incisions (usually 5–10 mm wide) are made in the abdomen. Through these, small ports are placed that allow instruments and a high-resolution 3D camera to be inserted.
-
Robotic System Docking: The robotic system is then "docked" to these ports. From a nearby console, the surgeon uses hand and foot controls to manipulate robotic arms.
-
Camera-Guided View: The 3D camera provides a magnified, high-definition view of the internal structures. This allows the surgeon to identify delicate tissue and blood vessels with much greater clarity.
-
Precision Dissection: Using robotic tools, the uterus is carefully separated from the cervix, ovaries, fallopian tubes, and surrounding ligaments. Blood vessels are sealed and cut with minimal bleeding.
-
Uterus Removal: The uterus may be removed in one piece through the vagina or morcellated (cut into smaller sections) and extracted through one of the abdominal ports, depending on size.
-
Closure: After removal, all instruments are withdrawn, and the incisions are closed with sutures or surgical glue.
-
Monitoring: The patient is moved to recovery, where vitals are monitored. Most can walk within a few hours after the surgery.
Recovery After the Procedure
The hysterectomy recovery time after a robot-assisted procedure is generally smooth, with less pain and a quicker return to daily activities compared to traditional open surgery.
-
Most patients are required to stay only 24–48 hours. Some may even go home the same day, depending on their health and the complexity of the surgery.
-
Discomfort is usually mild and managed with oral painkillers. There's significantly less pain than with open abdominal surgery.
-
Light activities like walking are encouraged within a day. Most women can return to work and regular routines in 2–3 weeks.
-
Small incisions need minimal care and usually heal without stitches needing removal. You only have to watch for signs of infection, like redness or discharge.
-
A post-operative check-up is usually scheduled within 1–2 weeks to monitor healing.
-
Heavy lifting and sexual intercourse should be generally avoided for 6 weeks or as advised by the doctor.
-
Fatigue may persist for a few weeks. Full internal healing can take up to 6–8 weeks.
Benefits of Robot-Assisted Hysterectomy
This approach offers several medical and lifestyle advantages over traditional open or even laparoscopic surgery.
-
Since the incisions are small, there is less scarring on the abdomen and quicker healing.
-
Reduced blood loss during surgery, so you will need fewer blood transfusions.
-
The hospital stay is short and often just 1–2 days.
-
Lower risk of infection due to minimal exposure.
-
Less postoperative pain reduces dependence on strong painkillers.
-
Faster return to routine activities, often within 2–3 weeks.
-
Improved surgical access to the pelvic region, especially in complex cases.
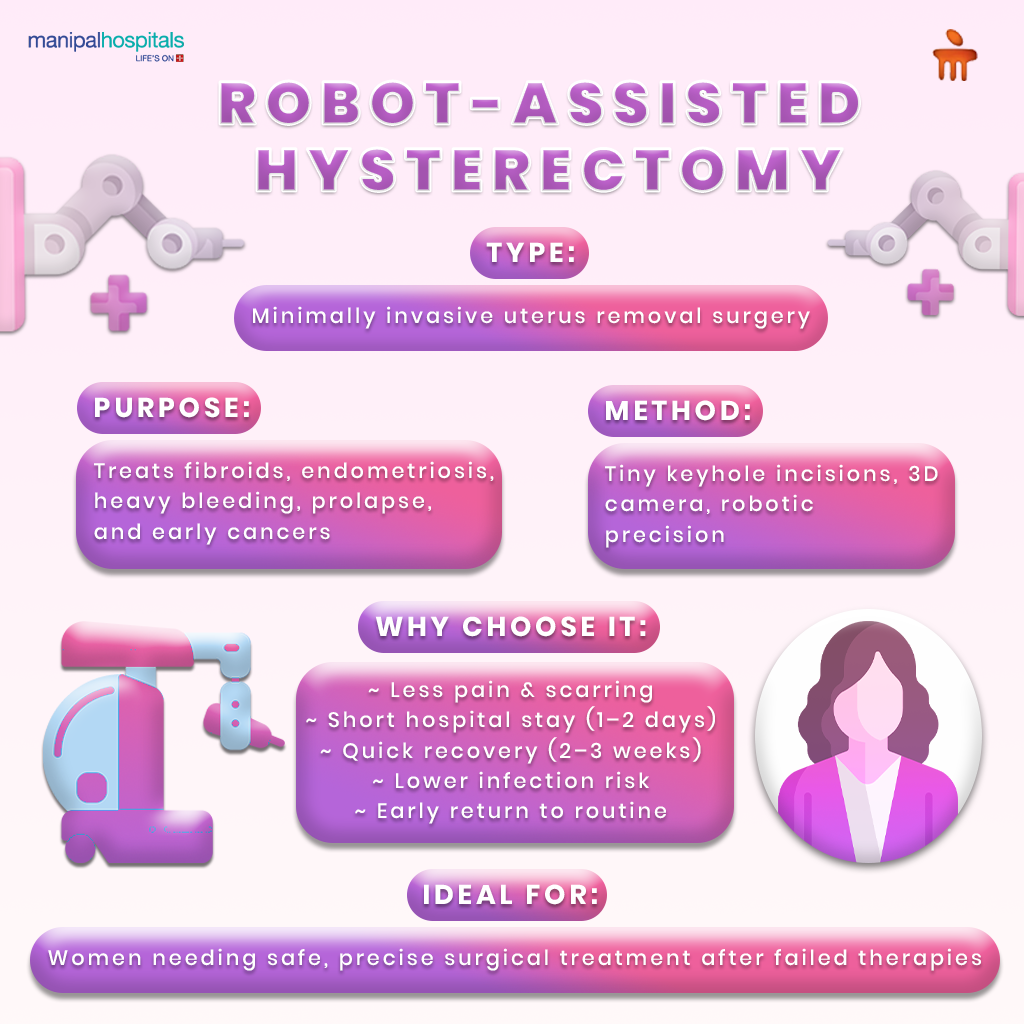
Who can Consider the Procedure?
Robot-assisted hysterectomy is typically recommended when other treatments haven’t worked or when surgery is the most effective option. Although it's not always the first step, it’s becoming a common and preferred method for many patients needing a hysterectomy.
-
Women with symptomatic fibroids who don’t respond to medication.
-
Those with endometriosis may experience severe pain or fertility issues.
-
Patients with early-stage gynaecological cancers need precise removal.
-
Women with chronic abnormal bleeding unresponsive to conservative therapies.
-
Cases of uterine prolapse, especially in postmenopausal women.
-
Patients needing revision surgery, where robotic access improves outcomes.
-
Minimally invasive surgery is preferred for faster recovery and fewer complications.
-
It may be recommended after nonsurgical treatments fail or if imaging shows that open surgery poses higher risks.
Conclusion
Robot-assisted hysterectomy is a safe procedure that offers a fast recovery time and safe surgical outcomes. If you’re exploring treatment options and want expert guidance, consult our robotic surgery specialist at Manipal Hospitals, Old Airport Road. Our specialist teams offer advanced and personalised care using cutting-edge robotic technology. Book an appointment today!
FAQ's
Yes, pelvic surgery robotics is safe and well-established. The surgeon controls the robot at all times, and the system enhances the accuracy with which different procedures are performed. The advantage is that it reduces risks like infection, bleeding, and pain compared to open surgery.
Most patients return home within 24–48 hours after a robotic hysterectomy. The recovery period is about 2–4 weeks, which is much shorter than traditional surgery. Light activity can be resumed much sooner, depending on individual health and the extent of the procedure, and they can get back to their normal routine in no time.
The procedure is often recommended for conditions like fibroids, heavy bleeding, endometriosis, or uterine cancer, provided the woman has no desire for children or she has passed menopause. Most often, it’s a last resort, and many doctors prefer it early for suitable cases due to better outcomes and quicker recovery.
Scarring is minimal since the robotic surgery uses small incisions that are usually less than an inch. These incisions heal quickly and often fade over time. With proper post-surgical care, the scars can be minimised. If needed, the leftover marks from the procedures can be easily corrected with simple cosmetic procedures.
In a minimally invasive hysterectomy, the robot doesn’t act independently or perform surgery on its own. It only mirrors the surgeon’s hand movements with complete control of the surgeon at all times. You can think of it as an extended tool. The procedure is fully controlled by a trained specialist, offering greater safety in confined or sensitive areas.





















 7 Min Read
7 Min Read