Diabetes care goes beyond pills and injections. Lifestyle choices shape blood sugar control, prevent complications, and improve quality of life. Thoughtful changes in diet, physical activity, sleep, stress management, and daily self-care form the backbone of effective diabetes control. These practical diabetes management tips focus on actions that reliably reduce risk and support long-term health.
The aim here is to present clear, evidence-based guidance on a balanced diabetic diet, realistic exercise plans, and sensible daily routines. The guidance is suitable for people with type 1 diabetes, type 2 diabetes, and those at high risk. Clinical care, regular follow-up with an endocrinologist, is critical, but a healthy lifestyle puts clinical measures on a stronger footing.
Synopsis
- Diabetes and Lifestyle: What is the Connection?
- Build a Balanced Diabetic Diet
- Move More: Practical Exercise Guidance
- Weight Management
- Sleep and Stress
- Medication, Monitoring, and Safe Adjustments
- Alcohol, Smoking, and Medication Interactions
- Practical Lifestyle Tips for Diabetes
- When to Seek Specialist Care
- Conclusion
Diabetes and Lifestyle: What is the Connection?
Diabetes mellitus is a common lifestyle disorder where your daily habits hold more power than you might realise. Every choice, from weight loss and increased activity, which improve insulin sensitivity, to dietary plans, which stabilise glucose fluctuations, is a form of disease management. Stress reduction also lowers hormones that raise blood sugar. Over time, these changes reduce the need for medication escalation, lower cardiovascular risk, and preserve kidney and nerve function. In other words, small everyday choices add up to meaningful health gains.

Build a Balanced Diabetic Diet
Nutrition is central to diabetes control. A well-structured diabetic diet aims to stabilise blood glucose, provide adequate nutrients, and support a healthy weight. Key principles:
|
Focus on whole foods |
Prioritise vegetables, whole grains, legumes, lean proteins, nuts and seeds, and fresh fruit in moderation. |
|
Control carbohydrate quality and quantity |
Choose complex carbohydrates (brown rice, millets, oats) and combine them with protein or healthy fats to slow absorption. |
|
Prefer low glycaemic index foods |
Foods that raise glucose slowly reduce post-meal spikes. |
|
Keep portion sizes consistent |
Regular portions at predictable intervals help avoid wide glucose swings. |
|
Limit refined sugars and processed foods |
Sugary drinks, sweets, and packaged snacks quickly raise blood glucose and add empty calories. |
|
Include healthy fats |
Use sources such as olive oil, nuts, fatty fish, and avocado, while minimising trans fats. |
|
Hydrate sensibly |
Water is best; avoid sugary beverages and limit alcohol. |
Work with a registered dietitian to personalise the diabetic diet for cultural preferences, comorbidities, and medication schedules. Meal plans should be realistic and sustainable.
Move More: Practical Exercise Guidance
Physical activity is a powerful tool for both preventing and managing diabetes. Exercise improves insulin sensitivity, assists weight control, and supports cardiovascular health.
-
Aim for at least 150 minutes per week of moderate-intensity aerobic activity (for example, brisk walking, cycling, or swimming).
-
Add strength training on two or more days per week to build muscle and maintain metabolic rate. Resistance exercises are especially advantageous for people on insulin or those with metabolic syndrome.
-
Break long periods of sitting into short activity bursts. Standing or walking for a few minutes every hour helps with glucose regulation.
-
Start gradually if sedentary, and increase intensity under professional guidance. People with complications such as neuropathy, retinopathy, or cardiovascular disease should receive tailored exercise advice from their care team.
-
When following diabetes management tips, consistency matters more than intensity. Daily movement that fits into life is better than sporadic heavy workouts.
Weight Management
For many people with type 2 diabetes, modest weight loss (5–10% of body weight) produces large metabolic benefits. Strategies that work include portion control, regular physical activity, and mindful eating. Avoid extreme diets that are unsustainable or interfere with medication. If weight remains difficult despite lifestyle changes, discuss pharmacologic or procedural options with an endocrinologist.
Sleep and Stress
Poor sleep and chronic stress raise blood glucose and worsen insulin resistance. Address both with practical steps:
-
Prioritise 7–8 hours of sleep nightly and keep a consistent sleep–wake schedule.
-
Reduce evening screen time, and make the bedroom restful and dark.
-
Practice brief daily stress-reduction techniques, deep breathing, progressive muscle relaxation, or short mindfulness sessions.
-
Seek help for anxiety, depression, or persistent sleep problems; these conditions affect self-management and deserve clinical attention.
Medication, Monitoring, and Safe Adjustments
A healthy lifestyle comprising diabetes management tips complements, but does not replace, prescribed medication where needed. Regular self-monitoring of blood glucose and periodic HbA1c testing guide adjustments. Follow these principles:
-
Take medications exactly as prescribed and discuss any side effects promptly.
-
Understand how food, exercise, and illness affect glucose and medication needs. Plan for activity and sick days.
-
Carry identification that indicates diabetes, and if on insulin or sulfonylureas, be prepared to manage hypoglycaemia.
-
Use technology where helpful: glucose monitors, structured logs, or apps to track trends. Share these records with the care team.
-
Close collaboration between the individual and the endocrinologist keeps treatment safe and effective.
Alcohol, Smoking, and Medication Interactions
Alcohol can cause unpredictable glucose swings and increase hypoglycaemia risk, particularly for those on insulin or sulfonylureas. If consumed, do so in moderation and with food. Smoking increases cardiovascular risk substantially; cessation is one of the most effective steps to reduce complications. Discuss nicotine replacement and other support with the care team.
Practical Lifestyle Tips for Diabetes
Some of the key diabetes management tips are listed below:
-
Plan meals and snacks to align carbohydrate intake with medication timing.
-
Prepare simple meals at home; cooking controls ingredients and portions.
-
Keep healthy snacks accessible to prevent overeating.
-
Schedule routine physical activity and make it enjoyable; walking with friends or gardening counts.
-
Set small, measurable goals and celebrate progress. Breaking large goals into weekly targets improves adherence.
-
Join a support group or diabetes education programme. Peer learning improves long-term outcomes.
These diabetes management tips create a stable foundation for metabolic control.
When to Seek Specialist Care
Seek prompt medical attention for frequent hypoglycaemia, unexplained hyperglycaemia, symptoms of infection, new visual changes, persistent numbness or pain in the feet, or sudden weight loss. Regular follow-up with an endocrinologist ensures timely modification of therapy and management of complications.
Conclusion
Effective diabetes care rests on a partnership between medical treatment and a healthy lifestyle. These diabetes management tips—a balanced diabetic diet, regular physical activity, good sleep, stress control, preventive screening, and careful medication use, work together to reduce complications and support daily well-being. Making sustainable, evidence-based changes delivers real results.
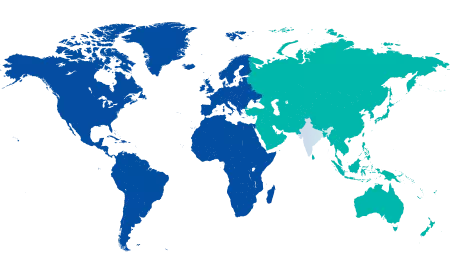
For personalised evaluation, monitoring, and a structured care plan, consult an endocrinology specialist at Manipal Hospital Jayanagar.
FAQ's
Frequency depends on treatment: people on insulin may check multiple times daily, while those on diet or oral drugs may test less often. Follow the endocrinologist’s plan and use tests to guide lifestyle and medication adjustments.
Some people with early type 2 diabetes achieve control with lifestyle changes alone. Others require medication. Decisions should be individualised, based on glucose levels, duration of diabetes, and overall health.
Aerobic activity combined with resistance training offers the greatest benefits. Aim for at least 150 minutes of moderate aerobic exercise weekly plus two strength sessions.
Stress hormones raise blood glucose and can make control harder. Regular stress-reduction techniques and professional support when needed improve metabolic control.
See a specialist at diagnosis, when control is suboptimal, when starting insulin, or when complications arise. Routine specialist follow-up ensures appropriate long-term management.





















 7 Min Read
7 Min Read


--Symptoms-and-Septoplasty-Recovery.png)