-
Book Appointments & Health Checkup Packages
- Access Lab Reports
-
-
Book Appointments & Health Checkup Packages
-
Centre of
Excellence
Centre of Excellence
- Bariatric Surgery - MIBS
- Bariatric Surgery
- Cancer Care
- Cardiology
- Cardiothoracic Vascular Surgery
- General Surgery
- Hemato Oncology
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Orthopaedics
- Paediatric And Child Care
- Renal Sciences
- Robotic Assisted Surgery
- Urology
- Vascular and Endovascular Surgery
Other Specialities
- Accident and Emergency Care
- Anesthesiology
- Bone Marrow Transplantation
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- IVF and Infertility
- Laboratory Medicine
- Liver Transplantation Surgery
- Medical Gastroenterology
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Neurology
- Paediatric Surgery
- Pain Medicine
- Physiotherapy
- Plastic, Reconstructive And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Reproductive Medicine
- Rheumatology
- Spine Care
- Surgical Gastroenterology
- Doctors
- Yeshwanthpur
-

Bengaluru

-
-

Bhubaneswar

-

Bhubaneswar
-
-

Delhi - NCR

-

Goa

-

Goa
-
-

Jaipur
-

Kolkata

-

Mangaluru
-

Mysuru
-

Patiala
-

Pune

-

Ranchi
-

Salem
-

Siliguri City

-

Vijayawada
- International Patients



Clinics







- Self Registration
- In-Patient Deposit
- Mars - Ambulance
- Home Care
- Organ Donation
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Manipal Insider
- Extended Clinical Arm
- Careers
- Contact Us

Sickle cell anaemia
Sickle cell anaemia in Yeshwanthpur, Bangalore
Sickle cell anaemia is an autosomal recessive hereditary disorder in which the RBC (Red blood corpuscles) become sickle-shaped and cause oxygen deficiency. The main function of RBC is to carry oxygen from the lungs to the rest of our body. Red blood cells are normally round and flexible, so they easily flow through blood vessels.
However, in sickle cell anaemia, RBCs become sickle-shaped like crescents. Due to their rigid and sticky nature, they clog the blood flow and thereby cause oxygen deficiency in some parts of the body. The sickle cells often have short life spans and hence die early, which causes a shortage of RBCs.
Causes of Sickle cell anaemia
Sickle cell anaemia is a genetic condition where a child receives two sickle cell genes – one from each parent. If a child inherits only one sickle cell gene, then it is called sickle cell trait. Sickle cell anaemia in Yeshwanthpur, Bangalore is available at Manipal Hospitals, visit today.
Symptoms
Sickle cell anaemia starts showing symptoms around 6 months of age. Some of the common symptoms include,
-
Anaemia - Healthy Red blood cells usually live up to 120 days until replaced. But these sickle cells easily break and die within 10 – 20 days. This causes a shortage of RBCs which in turn leads to a lack of oxygen and causes fatigue.
-
Pain crisis - When the sickle cells block flow to tiny blood vessels connected to your chest or abdomen, it causes severe pain. The intensity of pain varies from person to person and can last from a few hours to a few days.
-
Vision problems - When the blood supply to the eyes is blocked by sickle cells, it can damage the retina and lead to vision problems.
-
Jaundice - Sickle cells tend to have shorter life spans than other RBCs. Bilirubin from these broken-down cells causes Jaundice.
-
Stroke - When the blood and oxygen supply to the brain is interrupted by sickle cells, it leads to severe brain damage or stroke.
Diagnosis
A Blood test is done to check for the presence of the sickle cell form of haemoglobin. In many countries, this test is a part of newborn screening.
Sickle cell disease can also be diagnosed in an unborn baby by testing the amniotic fluid around the baby in the mother’s womb. This can be done when both parents have sickle cell genes. Early diagnosis and treatment can reduce complications. Book an appointment to know more about the diagnosis procedures.
Treatments
Sickle cell disease is a lifelong illness. Medications are given only to reduce the symptoms and to prevent further complications. However, the only cure currently available for SCD is a Bone marrow transplant, but this is not for everyone.
-
Hydroxyurea
It is an anti-cancer drug. This medicine helps in reducing the pain crisis and increases haemoglobin. It also reduces the clotting of blood vessels. It induces the production of fetal haemoglobin (HbF). However, pregnant patients must strictly avoid this drug.
-
Penicillin
Since SCD patients are easily prone to infections, penicillin is prescribed for children up to 5 years of age. Adults with SCD need to take penicillin lifelong if they have undergone any spleen surgery.
-
L-Glutamine
This medicine is prescribed to protect sickled cells from becoming more misshapen. FDA has approved this drug for children above 5 years of age.
-
Voxelotor
This medicine prevents the conversion of abnormal haemoglobin RBCs into sickled cells. It slows down the destruction of sickled RBCs and improves blood flow to organs.
-
Blood Transfusions
Blood transfusions are normally recommended to treat or prevent stroke in SCD patients. It provides healthy RBCs by injecting the donor’s blood that has matching antigens.
-
Stem cell Transplant
This is the only “cure” available for treating SCD currently. Stem cells produced by bone marrow can be turned into different types of cells. Thus, stem cells of a healthy donor are injected into the patient, which in turn starts producing healthy RBCs. However, it also involves various risks, such as graft vs host disease, where the donor cells start attacking the host cells. This treatment is recommended only for critical patients, and the biggest challenge lies in finding a suitable donor.
Home Yeshwanthpur Specialities Hemato-oncology Sickle-cell-anaemia

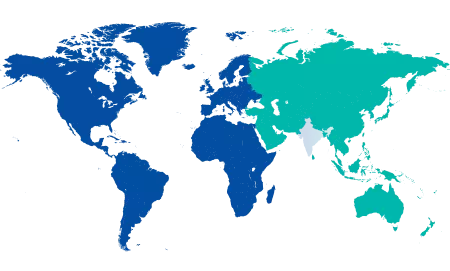
You’re on Our Indian Website
Visit the Global site for International patient services





