Arthritis, often misunderstood as something affecting only adults, can also present as a concern in childhood. Juvenile Arthritis is a serious condition that requires early diagnosis and proper care. It comprises almost 80% of the paediatric rheumatic disorders as reported by the hospitals. Recognising the early symptoms and understanding the causes and treatment options can make a big difference in a child’s quality of life.
Synopsis
What is Juvenile Arthritis?
Juvenile Idiopathic Arthritis (JIA), earlier known as Juvenile Rheumatoid Arthritis, is a type of chronic arthritis that affects children under the age of 16. It causes inflammation in one or more joints associated with pain, stiffness, and swelling. Many children may go through periods of remission and outgrow it in due course, but some may continue suffering with it into adulthood.
Types of Juvenile Idiopathic Arthritis (JIA)
The term JIA does not indicate a single disease but is a group of related conditions (autoimmune diseases) with specific attributes and complications. In JIA, the immune cells of the body attack its tissues, especially in the joints, causing inflammation and damage.
Juvenile Idiopathic Arthritis is the umbrella term that includes:
-
Oligoarticular JIA (Oligoarthritis)- mostly affects four or fewer large joints like the knees, elbows and ankles (in an asymmetrical pattern). It is the most common and mildest form of JIA
-
Polyarticular JIA (Polyarthritis)- affects multiple (five or more) joints simultaneously. It can be associated with many conditions or infections
-
Systemic JIA (Still’s Disease)- a multifactorial auto-inflammatory disease with a higher mortality rate compared to other types of JIA
-
Enthesitis-Related Arthritis (ERA)- an inflammation of the ‘entheses’ (where tendons and ligaments attach to bones), mainly affecting the lower limbs and spine
-
Psoriatic Arthritis- associated with psoriasis (a skin and nail disease), affecting about 30% of people with the disease
-
Undifferentiated JIA- symptoms do not fit completely into any of the other types of JIA or may fit into multiple types at the same time
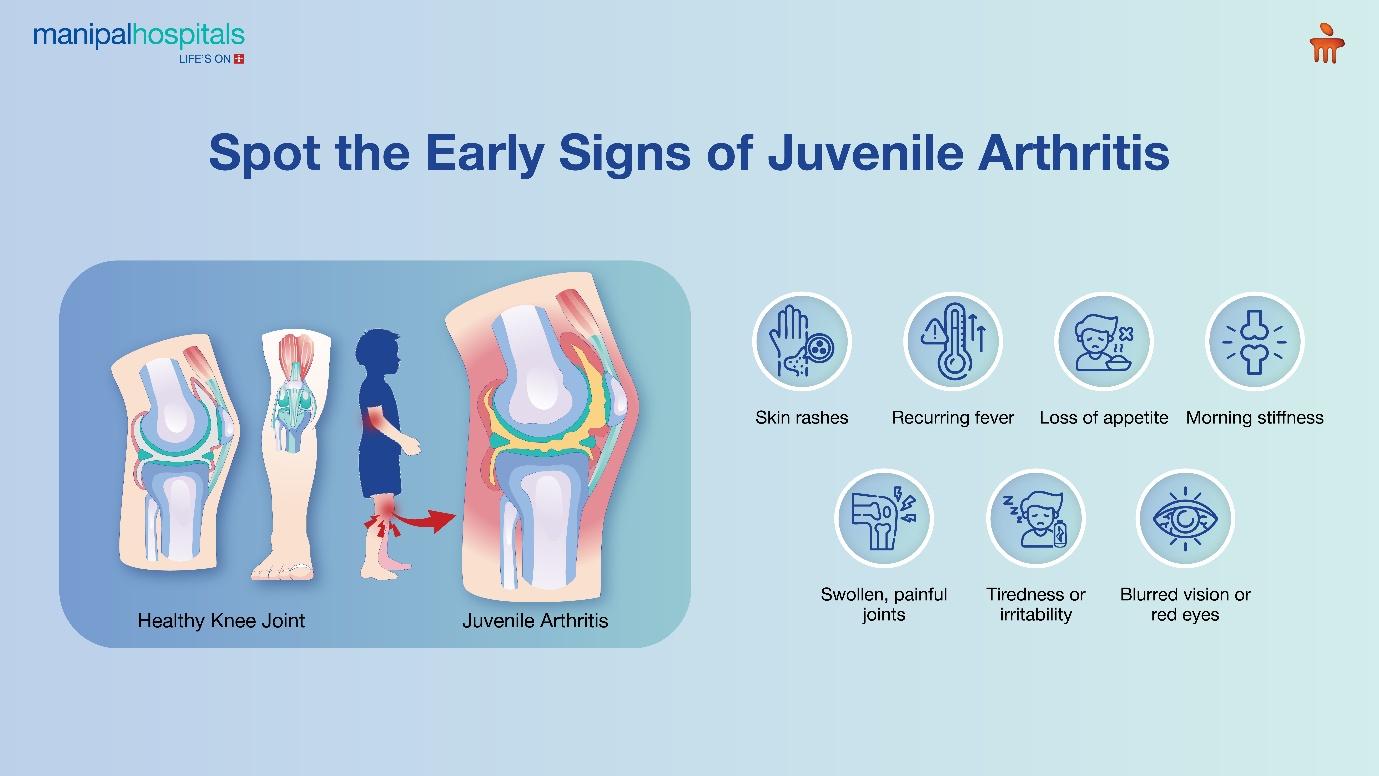
What are the common symptoms of Juvenile Idiopathic Arthritis?
Symptoms of Juvenile Rheumatoid Arthritis are common across all its variants. These may include:
-
Swelling, pain and inflammation in the joint/joints- these are the primary complaints in a JIA patient
-
Stiffness- especially in the morning or after a span of inactivity
-
Inflammation in the eyes (known as Uveitis)- in some cases, the eye is affected with redness, pain and blurry vision
-
Skin rashes, fever and swollen lymph nodes- this is seen particularly in Systemic JIA
-
Loss of appetite and weight loss are present at times
-
Fatigue and irritability- might be present
What causes Juvenile Arthritis?
In most cases, Juvenile Arthritis has no clear cause, hence the term ‘Idiopathic’. Yet, a few factors can stimulate the development of JIA:
-
Improper autoimmune response
-
Presence of certain genes like HLA (Human Leukocyte Antigen)
-
Specific type of viral/bacterial infections in susceptible children
-
Being a female- Most subtypes of Juvenile Arthritis are slightly more common in females, except Enthesitis-related arthritis, which shows a male preponderance.
-
Age under 16 yearWhat are the common complications of JIA?
-
JIA can lead to several short-term and long-term complications, such as:
-
Erosion of bone and cartilage leading to deformity, disability and reduced range of motion
-
Delayed, stunted or faster growth
-
Loss of vision, cataract or glaucoma
-
Weak bones/Osteoporosis with increased risk of fracture
-
Low quality of life with poor sleep and difficulty concentrating
-
Hormonal imbalance causing delayed puberty
-
Complications with heart and/or lungs (especially in Systemic JIA)
-
Depression, anxiety and loneliness
How is Juvenile Rheumatoid Arthritis treated?
Juvenile Arthritis does not have a cure. Treatment essentially aims to control inflammation, prevent joint damage, and relieve symptoms. The mode of treatment depends on the type and severity of the condition. These involve:
-
Medication- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) are the first line of treatment in mild cases, Disease-Modifying Anti-Rheumatic Drugs (DMARDs) to slow disease progression, Biologic agents to target specific parts of the immune system in moderate to severe JIA, and Corticosteroids for controlling inflammation quickly
-
Therapy- Physical and Occupational therapies are done using splints, braces or exercises for joint flexibility, muscle strength and prevention of deformity to help with daily activities
-
Surgery-This is considered only when the joints are severely damaged and other treatments have failed. This includes correctional surgeries (for deformity) and joint replacement
Apart from treatment, regular monitoring (eye screening, blood tests and imaging), time to time-to-time follow-up with a paediatric rheumatologist, exercising (swimming, stretching, balanced diet to aid in growth and bone health, and psychological support/counselling can go a long way in helping a JIA-affected child lead an easier life.
Conclusion
Cases of Juvenile Idiopathic Arthritis, though much prevalent in India, are mostly under-reported owing to a lack of awareness. Most of the reported cases are diagnosed at a later stage with a considerable extent of joint damage, growth impairment and functional disability. JIA is a treatable condition, provided detection is early and proper care is provided.
If you notice symptoms or suspect your child to be at risk of Juvenile Arthritis, do not delay in checking with a specialist. Manipal Hospitals Salt Lake provides precise diagnosis and state-of-the-art treatment facilities for Juvenile Idiopathic Arthritis.
FAQ's
Certain types of Juvenile Arthritis may resolve in childhood, while others persist into adulthood. The child may go into remission and no longer have joint symptoms, but then have a disease flare years later.
No, JIA is not contagious; it does not spread from person to person.
JIA can affect bone growth and development adversely, especially if left untreated.
Although there remains a genetic component, most siblings do not develop JIA unless there is a family history of autoimmune diseases.
‘Remission’ implies a period when the child has no active symptoms, with or without any medication.





















 6 Min Read
6 Min Read