Blood tests give doctors signals about what is happening inside your body. One of the oldest and most widely used of these signals is the erythrocyte sedimentation rate, commonly called the ESR test. The main point of this blog is to help you understand what this simple laboratory measure actually reflects, why it is useful, and where it falls short. You will learn how the test works, what a high value may indicate, the common causes behind a raised reading, and how doctors interpret the result alongside other tests.
Synopsis
- What the ESR Test Measures
- How the Test Works in Practical Terms
- When Doctors Order an ESR Test
- High ESR May Indicate
- Low or Normal ESR and What It Means
- Factors That Affect ESR Beyond Inflammation
- How Doctors Interpret ESR Results
- Limitations of the ESR as an Inflammation Marker
- Conditions Where ESR Is Especially Helpful
- What to Do if Your ESR Is High
- Tests Commonly Paired With ESR
- Practical Tips for Patients
- When to Seek Specialist Care
- Conclusion
What the ESR Test Measures
The ESR test measures how quickly red blood cells settle to the bottom of a narrow tube over one hour. This rate of settling increases when there is more protein in the blood, which causes cells to stick together and fall faster. Because inflammation changes blood proteins, the ESR becomes a broad indicator of inflammatory activity in the body. It does not identify a cause, but it often prompts further investigation when it is higher than expected.
How the Test Works in Practical Terms
The method for measuring ESR is straightforward and inexpensive, which explains its continued use in many clinical settings. A sample of blood is placed in a vertical tube and left undisturbed for 60 minutes. The distance the red cells fall is read in millimetres and reported as the ESR value. A higher millimetre value corresponds to faster settling and generally more inflammation. The test is commonly reported as millimetres per hour.
When Doctors Order an ESR Test
Clinicians ask for the ESR test when they want a broad sense of inflammatory activity or when symptoms are vague. It is frequently used in the initial assessment of unexplained fever, prolonged fatigue, or joint pain. The test is also used to track response to treatment in established inflammatory disorders. Because the ESR is inexpensive and easy to repeat, it remains a routine tool for monitoring conditions over time.
High ESR May Indicate
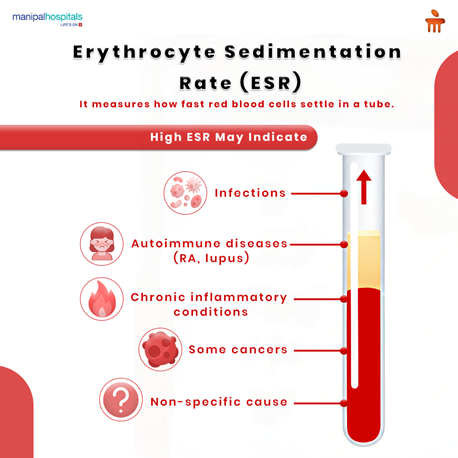
A raised ESR is a non-specific finding. It signals that inflammation is present, but it does not point to one single diagnosis. When you have a higher ESR, your doctor will interpret this result together with your symptoms, examination, and other tests.
Common conditions associated with a high ESR include:
-
Infections such as bacterial pneumonia or tuberculosis.
-
Autoimmune diseases, including rheumatoid arthritis and lupus.
-
Chronic inflammatory conditions like inflammatory bowel disease.
-
Some cancers provoke systemic inflammation.
-
Cases where no single cause is found, producing a non-specific elevation.
If your ESR is high, your clinician will use the result to guide further testing and to monitor how you respond to treatment.
Low or Normal ESR and What It Means
A normal or low ESR does not rule out disease. Many acute infections and some serious inflammatory conditions can present with a normal ESR, particularly early in the illness. Younger people may have lower ESR values overall. For these reasons, your doctor will not use ESR in isolation. It is one piece of clinical data among many that inform diagnosis and management.
Factors That Affect ESR Beyond Inflammation
Several non-disease factors influence the ESR. Age and sex alter the expected normal range. Pregnancy raises ESR. Anaemia increases ESR because fewer red cells make it easier for cells to aggregate and settle. On the other hand, very high cholesterol, sickle cell disease, or certain medications can lower ESR. Laboratory technique and the precise method used also affect results. For these reasons, doctors interpret ESR within the full clinical context rather than as an absolute measure.
How Doctors Interpret ESR Results
Interpreting ESR involves both the absolute value and its trend over time. A single mildly raised ESR may be less concerning than a markedly high reading or a value that keeps rising. Doctors compare the ESR with more specific tests to find a cause. Common complementary tests include C-reactive protein, complete blood count, kidney and liver tests, and relevant imaging or microbiology tests. In many inflammatory conditions, clinicians rely on both ESR and C-reactive protein because each test provides slightly different information about the inflammatory process.
Limitations of the ESR as an Inflammation Marker
The ESR test is useful but limited. It is non-specific and can be altered by many non-inflammatory factors. It responds slowly to change so that it may lag behind the clinical course. Drugs, pregnancy, and chronic conditions can produce persistent elevation that is not directly related to current disease activity. For these reasons, an isolated ESR result rarely provides a definitive diagnosis. Your doctor orders ESR to add a broader perspective, not as a standalone answer.
Conditions Where ESR Is Especially Helpful
While the ESR is not diagnostic, it is particularly helpful in certain clinical situations where it guides diagnosis and monitoring. These include:
-
Large vessel vasculitis and temporal arteritis, where a very high ESR supports urgent investigation.
-
Monitoring inflammatory arthritis, such as rheumatoid arthritis, to assess treatment response.
-
Following chronic inflammatory disorders, where trends in ESR reflect changing disease activity.
When ESR is used in these contexts, it is part of a structured plan that combines symptoms, physical findings, and targeted tests to reach a clear conclusion.
What to Do if Your ESR Is High
If your ESR result is higher than expected, the best step is to discuss the finding with your doctor. They will review your symptoms and may repeat the test or order more specific investigations to look for infections, autoimmune disease, or other causes. Treatment depends on the underlying diagnosis. Infections are treated with appropriate antimicrobials, autoimmune conditions may require anti-inflammatory or immunosuppressive therapy, and cancers are managed according to oncologic principles. Your clinician will explain the likely next steps and a timeline for follow-up.
Tests Commonly Paired With ESR
Because ESR is non-specific, it is often requested alongside other laboratory tests that provide more targeted information. These include:
-
C-reactive protein, which rises and falls more quickly with acute inflammation.
-
Full blood count to look for anaemia or signs of infection.
-
Kidney and liver function tests to screen for organ involvement.
-
Autoantibody panels are used when autoimmune disease is suspected.
-
Microbiology tests, such as blood cultures, if infection is a concern.
Using these tests together improves the accuracy of diagnosis and helps tailor treatment more precisely.
Practical Tips for Patients
Understanding laboratory reports helps you take an informed role in your care. If you have an ESR result to discuss, consider these practical points.
-
Keep a record of symptoms and share them with your clinician.
-
Ask whether the test will be repeated to follow trends.
-
If medication or a chronic condition may affect ESR, tell your doctor.
-
Do not panic over a single elevated value; ask what the likely causes are and what investigations will follow.
-
For conditions that require long-term monitoring, discuss what change in ESR would prompt treatment adjustment.
These steps help you and your doctor make decisions based on both numbers and how you feel.
When to Seek Specialist Care
Some situations require referral to a specialist. If your doctor suspects an autoimmune disease, vasculitis, persistent unexplained inflammation, or a serious infection, they may refer you to a rheumatologist, infectious disease specialist, or a relevant physician for urgent assessment. Specialists use ESR along with more advanced tests and clinical expertise to reach a definitive diagnosis and start targeted treatment.
Conclusion
The Erythrocyte sedimentation rate is a long-established and useful inflammation marker. It gives clinicians a broad sense of inflammatory activity in the body and helps guide further testing. A high ESR may indicate infections, autoimmune diseases, chronic inflammatory conditions, some cancers, or a non-specific cause. The test has limits and is best used together with other investigations and careful clinical assessment. If your ESR is outside the expected range, work with your doctor to find the underlying reason and to plan appropriate follow-up.
For any concerns related to abnormal ESR levels, inflammation, or unresolved symptoms, consult the expert specialists at Manipal Hospitals for accurate diagnosis and personalised care. Book an appointment today for a timely evaluation and guidance.
FAQ's
Normal values vary by age and sex and by the laboratory method. A common general guide is up to 15 millimetres per hour for men and up to 20 millimetres per hour for women, but your lab report should state the reference range used. Always ask your clinician to interpret results against your personal context.
ESR changes more slowly than some markers. It can take days to weeks to fall after effective treatment, so doctors often use C-reactive protein for rapid changes and ESR to follow longer-term trends.
Yes. Pregnancy, anaemia, and certain medications can raise ESR. An isolated mild elevation without symptoms is often monitored rather than treated immediately.
Neither is categorically better. ESR and C-reactive protein measure different aspects of inflammation. CRP responds more quickly to acute changes, while ESR can reflect more chronic processes. Doctors often use both tests together for a fuller picture.
Ask what possible causes the clinician considers likely, whether further tests are planned, how the clinician will monitor progress, and what symptoms should prompt urgent review. Clear follow-up instructions reduce uncertainty and help you participate in care.





















 8 Min Read
8 Min Read









10.png)


8.png)