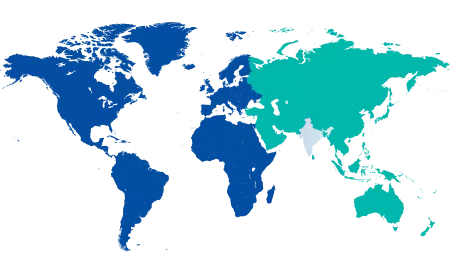
Thalassaemia is the most common hereditary disorder prevalent across the world. According to the WHO reports, 5% of the world population carries a pathological haemoglobin gene, causing 300,000 infants worldwide to be born with thalassaemia syndrome. India has a huge burden, with an estimated 100,000 patients suffering from beta thalassaemia syndrome, but only some of them are optimally managed. Individuals with thalassaemia minor, commonly described as having the thalassaemia trait, have the gene that causes the disease but do not have thalassaemia themselves. This blog post lets us understand the thalassaemia symptoms and causes in an individual.
Synopsis
What is Thalassaemia Disease?
Thalassaemia is an autosomal recessive condition characterised by haemoglobin deficiency, a protein that allows red blood cells to carry oxygen throughout the body. Without oxygen, the red blood cells die quickly, and the organs and tissues do not get enough oxygen. To develop thalassaemia symptoms, the individual must inherit the defective gene from both parents.
Thalassaemia minor is an inherited condition where you receive the defective gene for thalassaemia from only one parent. This does not cause any health issues in individuals with affected genes, but the trait can be passed on to future generations.
Types of Thalassaemia Minor
Alpha-thalassaemia trait is a highly prevalent condition, especially in Southeast Asia, the Middle East, and the Mediterranean, but the prevalence of beta-thalassaemia is less common.
- Alpha-thalassaemia trait
There are two types of this trait, as two genes, HBA1 and HBA2, are responsible for making haemoglobin alpha. Normally, healthy individuals inherit four copies of the gene, two from each parent. Depending on the number of genes affected, your symptoms can vary.
Individuals with one mutated gene are carriers for alpha-thalassaemia
If two genes are affected, the individuals develop alpha-thalassaemia minor. Such individuals have red blood cells smaller than normal, resulting in mild anaemia
If three or four genes are affected, then the individual develops a severe case of alpha-thalassaemia
- Beta-thalassaemia trait
Only the HBB gene is responsible for making haemoglobin beta. Individuals with beta-thalassaemia inherit two copies of the mutated gene, one from each parent. If the individual inherits one mutated gene, they develop beta-thalassaemia minor, a condition where red blood cells are smaller than normal, resulting in mild anaemia. If both genes are affected, the individual develops beta-thalassaemia major.
It is also possible for individuals to have traits of both alpha and beta-thalassaemia simultaneously.
Thalassaemia Minor Symptoms
Individuals with the thalassaemia trait will likely not have symptoms or may develop mild anaemia. Since red blood cells are smaller than normal, they will have low haemoglobin levels, resulting in mild anaemia. Thalassaemia symptoms associated with mild anaemia are pale skin, fatigue, and weakness. Pregnant women with a thalassaemia trait are at an increased risk of high blood pressure or anaemia during pregnancy. Unlike thalassaemia major, thalassaemia minor does not reduce the life expectancy of affected individuals.
How is the thalassaemia trait diagnosed?
Individuals with a family history of thalassaemia or with suspicion of the disease can undergo a complete blood test to determine whether they have a thalassaemia trait or not. The healthcare provider looks at the mean corpuscular volume (MCV) in the patient's CBC results to determine the size of their red blood cells. If the MCV is 80 or less, further blood testing (haemoglobin electrophoresis and quantification of haemoglobin A2 and haemoglobin F) may be prescribed to verify the trait status, or genetic testing may be performed to confirm the presence of a faulty gene.
Are treatments necessary for the thalassaemia trait?
If an individual is a silent carrier of thalassaemia minor, they do not require any treatments like Blood Transfusions or Iron Therapy. However, individuals with thalassaemia symptoms can be misdiagnosed with iron deficiency and may be prescribed iron supplements. Taking excess iron can negatively affect the health of individuals with the thalassaemia trait. Therefore, understanding thalassaemia causes and obtaining an accurate diagnosis with blood tests is necessary to avoid unnecessary thalassaemia treatment.
Why is discovering the thalassaemia trait early necessary?
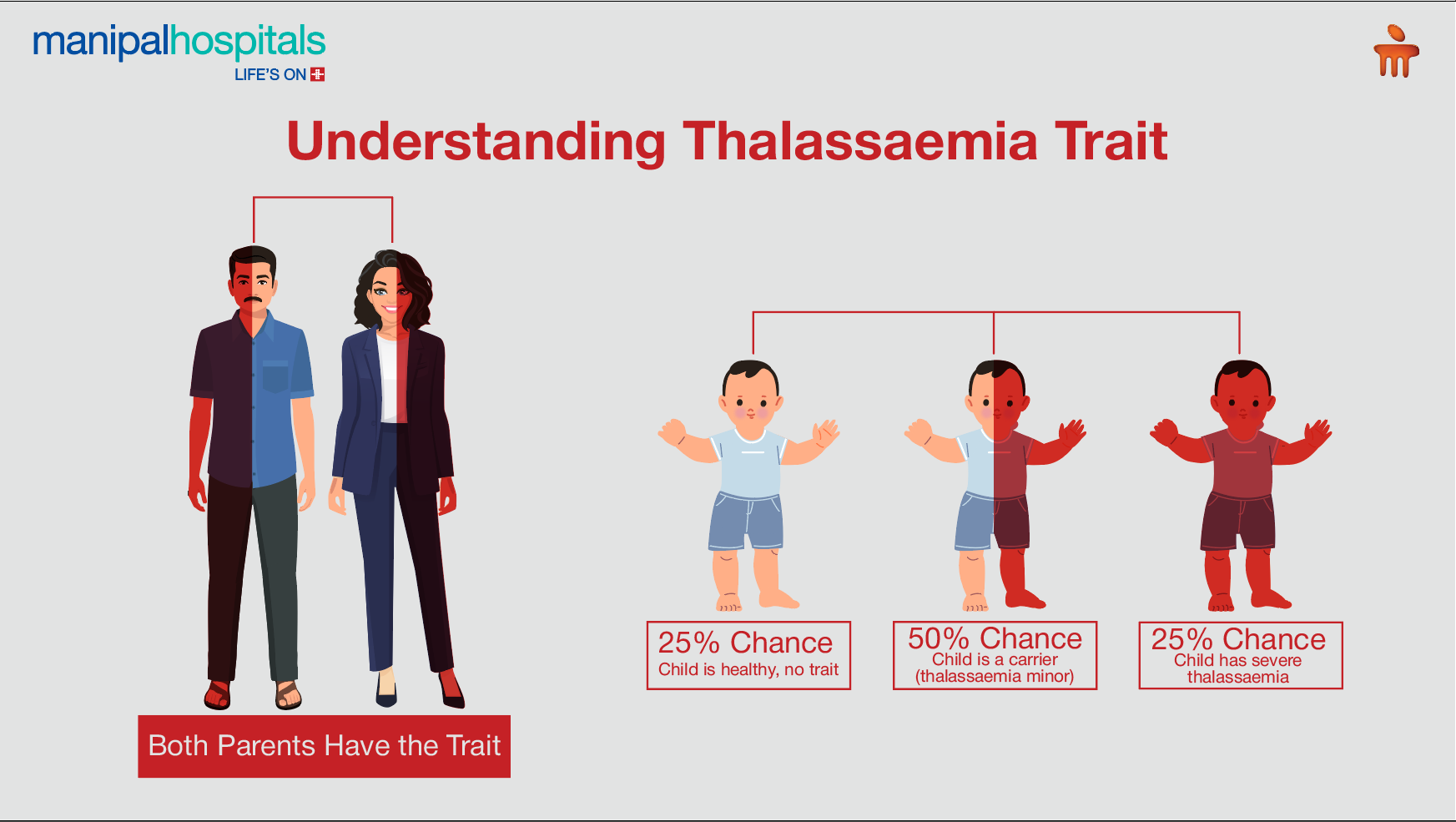
If two individuals with the same thalassaemia trait have a child, then there is a 25% increase in the risk of the child being born with severe thalassaemia. Getting genetic testing done can help the couple determine if they carry the mutated gene. This helps the couple to plan for their pregnancy.
If both you and your partner have the thalassaemia trait:
-
There is a 1 in 4 chance that your child will not have thalassaemia or carry the trait
-
There is a 1 in 2 chance that your child is a carrier but does not have the condition themselves
-
There is a 1 in 4 chance that your child will be born with severe thalassaemia
Conclusion
Understanding thalassaemia causes and symptoms is crucial for identifying carriers, reducing misdiagnosis, and preventing severe cases in future generations. If you suspect you or your partner may carry the thalassaemia gene, schedule a consultation at Manipal Hospitals, Kolkata, for accurate genetic testing and comprehensive genetic counselling. Also, pay attention to thalassaemia symptoms for better early detection and timely medical guidance to prevent complications and ensure appropriate care.
FAQ's
Since thalassaemia is an inherited condition, you must undergo screening if you are:
-
Planning to start a family
-
Have a family history
-
One partner has already been diagnosed with thalassaemia
Unless you suffer from both iron deficiency anaemia and thalassaemia, it is not advised to follow any dietary restrictions. However, if you also have iron deficiency anaemia, avoid foods that limit iron absorption, such as coffee, tea, milk, egg whites, and soy protein.
Individuals with the thalassaemia trait taking iron supplements can suffer from cardiac ailments such as arrhythmia and congestive heart failure. Iron overload can also lead to problems in the liver and endocrine system.
If a woman is pregnant, chorionic villus sampling is done about 11 weeks into pregnancy, or amniocentesis is done about 16 weeks into pregnancy, to determine thalassaemia risk in the foetus. In newborns, a screening test is performed soon after birth.
You can schedule an appointment at Manipal Hospitals, Kolkata, by contacting us or visiting our website.
Visit: https://www.manipalhospitals.com/kolkata/
Contact no: 033 6907 0001






















 6 Min Read
6 Min Read

.png)