Listen to article
Loading audio...
Drinking alcohol for pleasure, to beat work stress, or just to look cool? If you're one of them, stop before it's too late. Over 2 million people worldwide die each year due to liver diseases. Liver cirrhosis is a major public health concern and the 11th most common cause of death globally. According to WHO data, India accounts for one-fifth of all cirrhosis-related deaths worldwide, primarily due to the rising trend in drinking alcohol.1,2 Understanding the extent of liver damage caused by the moderate to regular consumption of alcohol is important to be safe.
This blog will help you get an understanding of alcoholic liver disease, its various stages, symptoms, causes, and treatment.
Synopsis
What is Alcoholic Liver Disease?
The liver is an important organ performing various bodily functions. Heavy alcohol consumption damages the liver and its functioning, leading to alcoholic liver disease. It is a broad category that progresses with time and consumption of alcohol, going from common fatty liver disease and liver hepatitis to cirrhosis, an end-stage, irreversible disease.
What are the Stages of Alcoholic Liver Disease?
If the alcohol consumption continues, the alcoholic liver disease progresses through three stages with time. These stages are:
Alcoholic Fatty Liver or Steatotic: The fat buildup starts in the liver parenchyma, leading to an enlarged liver. Steatotic liver is among the most common liver diseases caused by alcohol.
Alcoholic Hepatitis: At this stage, the inflammation of the liver cells starts taking place, causing the death of the cells, followed by permanent scarring. Its early detection can help in the treatment, but once it gets severe, it results in liver failure.
Alcoholic Cirrhosis: Destruction of the liver tissue occurs, leaving behind only scar tissue. This type of liver damage is irreversible, and the liver may soon stop working, leading to further complications.
What Causes Alcoholic Liver Disease?
As the name suggests, this type of liver disease is caused by heavy use of alcohol. Although the liver can tolerate and break down a smaller amount of alcohol, as the consumption increases, it starts affecting the metabolic functioning of the liver, resulting in the initial stage, known as alcoholic fatty liver. If the alcohol consumption continues, it progresses to alcoholic hepatitis and finally the end-stage liver cirrhosis.
As per WHO, 3.3 million people died in 2012 due to excessive alcohol consumption, which can damage almost every organ of the body, the liver being the first one.3
In addition, genetic, environmental, metabolic, and immunological factors also play a role in influencing alcoholic liver disease.
What are the Symptoms of Alcoholic Liver Disease?
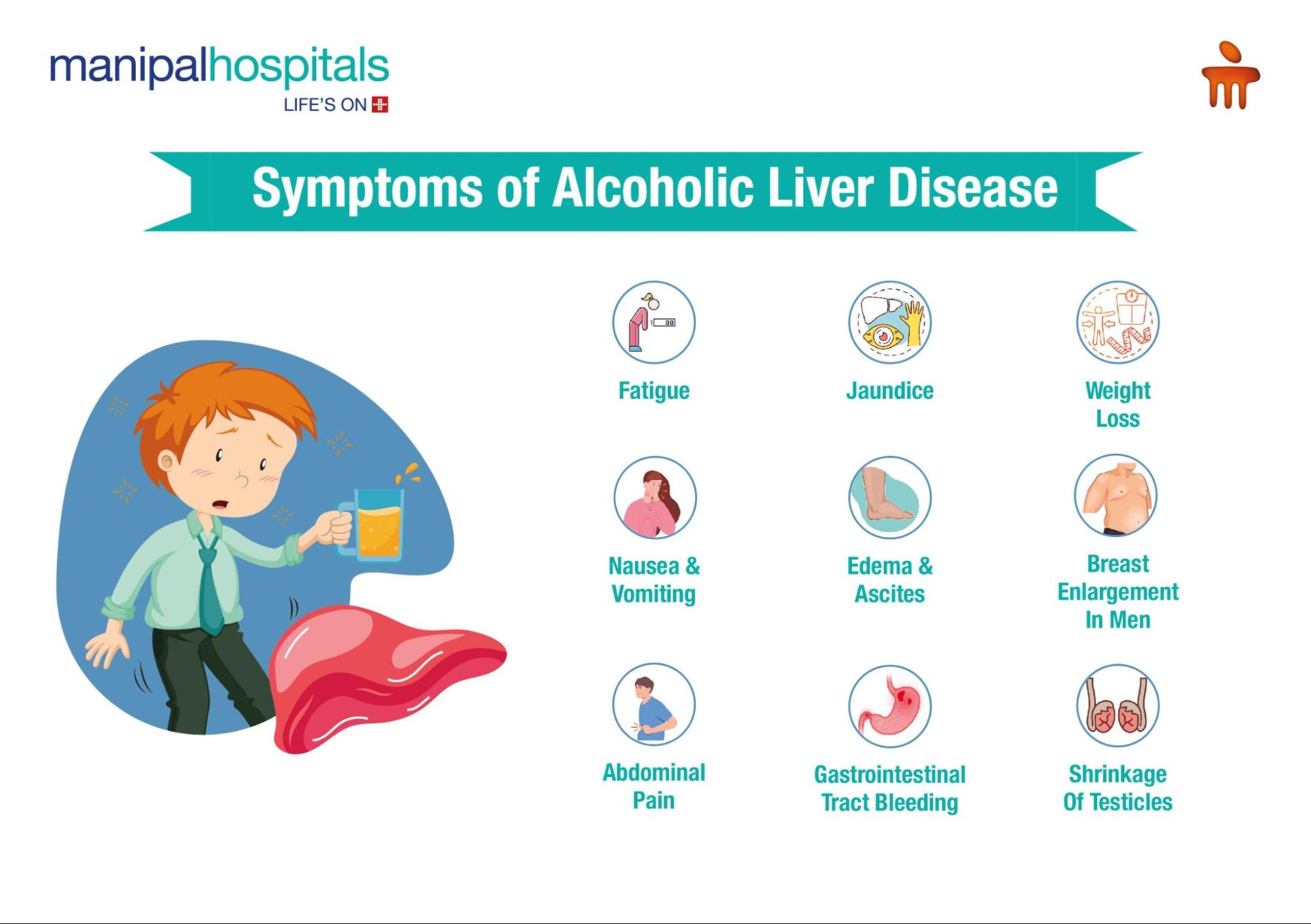
The alcoholic liver disease symptoms will vary based on many factors and the type of disease, but here are 14 signs of liver damage from alcohol that one should watch for. If you experience any of the symptoms, consult a hepatologist at the earliest.
-
Fatigue or weakness
-
Jaundice, yellowing of the skin and eyes
-
Poor appetite or weight loss
-
Abdominal pain, mostly in the upper right side
-
Nausea and vomiting
-
Fluid buildup or swelling in the legs (oedema) or abdomen (ascites)
-
Spider-like blood vessels on the skin - red and small
-
Easy bruising or abnormal bleeding
-
Breast enlargement in men
-
Confusion
-
Palms become red
-
Bleeding in the gastrointestinal tract
-
Shrinkage of the testicles in men
How is Alcoholic Liver Disease Treated?
There is no particular treatment for alcoholic liver disease, as it mostly remains unnoticed unless it reaches a severe stage of liver cirrhosis. The treatment options available are:
Alcohol Abstinence or Withdrawal: The liver has the capacity to recover, so to treat alcoholic liver disease, the best thing is to stop drinking alcohol completely before it reaches the last stage. The risk can be reduced, and the liver can recover before the disease progresses to cirrhosis.
Lifestyle Changes: In addition to leaving alcohol, make some other lifestyle changes to treat alcoholic liver disease early. These include:
-
Eat a well-balanced diet low in salt
-
Inform the doctor about all the medicines you are consuming
-
Get yourself vaccinated for influenza, hepatitis B, hepatitis A and pneumococcal pneumonia
Medications: Depending on the stage and severity of the disease, the hepatologist may prescribe certain medications to control the damage and alleviate the symptoms. These include:
-
Diuretics to get rid of the fluid buildup
-
Antibiotics (in case of infections)
-
Vitamin K to prevent bleeding
-
Benzodiazepines and antipsychotic drugs for alcohol withdrawal
-
Acamprosate and naltrexone to manage alcohol cravings
-
Drugs to improve liver health
Nutritional Therapy: Malnutrition usually occurs, especially in patients who are in the second stage of alcoholic liver disease. Nutritional Therapy can help and improve the stage of liver disease.
Liver Transplant: For severe cases and end-stage alcoholic liver disease, Liver Transplantation is the only solution. But this option is considered only if other treatment approaches or medications do not work. Also, to be eligible, you must have stopped drinking alcohol for almost 6 months.
Other Treatments: Endoscopic treatment for enlarged oesophageal veins, Paracentesis for the removal of fluid from the abdomen, and Transjugular Intrahepatic Portosystemic Shunt (TIPS) placement for portal hypertension.
Conclusion
If you are one of those who think occasional drinking will not affect your liver health, then it's time to rethink, as it can lead to liver damage. Mostly, how much alcohol you have been drinking and for how long will decide the stage of alcoholic liver disease. Stop worrying and book a consultation with an expert gastroenterologist at Manipal Hospitals, Broadway, and take the first step toward better liver health with a thorough checkup and appropriate treatment.
FAQ's
After a thorough physical examination and review of your medical history and symptoms, certain diagnostic tests may be recommended, such as blood tests, liver biopsy, ultrasound, CT scan, or MRI to help rule out the condition.
Alcohol-related liver damage can be reversed, if diagnosed in the early stages, by completely stopping alcohol consumption. However, the time and extent of damage that can be healed will depend on the stage of the disease and your overall health.
As per the National Institute of Health in 2023, heavy alcohol use is defined as :
-
Men: More than 4 drinks on any day or more than 14 drinks per week
-
Women: More than 3 drinks on any day or more than 7 drinks per week
This level of alcohol consumption increases the risk of liver damage, heart disease, mental health issues, and several types of cancer. Reducing or eliminating alcohol intake can significantly improve long-term health outcomes
If not treated on time, alcoholic liver disease can lead to the following complications:
-
Bleeding disorders
-
Complete liver damage
-
Mental confusion
-
Liver cancer
-
Kidney failure
-
Portal hypertension, increased blood pressure in the blood vessels of the liver
-
Enlarged veins in the oesophagus, stomach or intestines that can bleed
-
Gastrointestinal bleeding
-
Severe infections
You can contact us or visit our website to schedule an appointment with a haematologist at Manipal Hospitals, Broadway.



















 6 Min Read
6 Min Read










27.png)

26.png)

