Back pain is something almost everyone knows. Sometimes it’s a dull ache that fades away after rest. Other times, it feels sharper, spreading down the leg or arm. When pain starts shooting or tingling, it might be more than just strain. It could be a herniated disc.
This condition sounds more serious than it often is. Still, it helps to understand what’s happening inside your spine, what the signs look like, and how you can find proper relief.
Synopsis
What is a Herniated Disc
Your spine is built like a stack of small bones called vertebrae. Between them sit soft, cushion-like discs that act as natural shock absorbers. They let your back bend, twist, and move smoothly.
A herniated disc happens when one of these cushions gets a tear in its outer layer. The soft centre slips out slightly, pressing against a nearby nerve. That pressure is what causes pain, numbness, or weakness in the body.
You may have heard it called a slipped or ruptured disc. In truth, it doesn’t really “slip out”. It just bulges or leaks from its space.
Common Causes of a Herniated Disc
There’s rarely one single reason behind a herniated disc. For many people, it’s part of the natural ageing process. The discs dry out a bit, losing flexibility. Small cracks appear, and even simple bending or twisting can push the inner part outward.
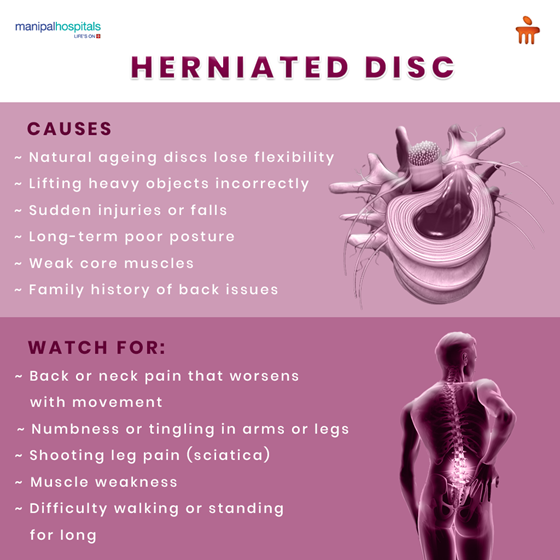
Some everyday habits can add to this:
-
Ageing: Normal wear and tear that weakens the disc over time.
-
Lifting the wrong way: Putting pressure on your lower back instead of your legs.
-
Sudden injuries: Accidents or awkward falls.
-
Poor posture: Slouching for long periods stresses the spine.
-
Weak muscles: Less core strength means less support for your back.
And sometimes, it runs in families. If your parents had back issues, your discs might be naturally a bit weaker, too.
Recognising the Symptoms
The signs of a herniated disc can vary depending on where it occurs in your spine. Most happen in the lower back or neck. The pain can be mild or intense, and it might travel along your nerves into your arms or legs.
Here are some of the usual herniated disc symptoms:
-
Pain in your lower back or neck that worsens when you move.
-
Numbness or tingling in your arms, hands, or legs.
-
Weakness in certain muscles.
-
Pain that shoots down one leg is often called sciatica.
-
Trouble standing or walking for long periods.
Some people describe it as a sudden, stabbing pain. Others feel a steady ache that lingers. If you notice the pain spreading, or it’s not going away, that’s your cue to check in with a doctor. Spotting herniated disc symptoms early makes recovery smoother and faster.
How a Herniated Disc is Diagnosed
Doctors usually start with a simple chat about your pain. When did it begin? What makes it worse? Does it travel to your arms or legs? They’ll then check your reflexes, strength, and range of movement.
If they suspect a herniated disc, they might suggest a few tests:
-
MRI scan: Gives a clear image of soft tissues and nerves.
-
CT scan: Offers a closer look at your discs.
-
X-ray: Rules out other bone issues.
The aim is to understand not just if there’s a herniated disc, but how much it’s affecting your nerves and daily activities.
Herniated Disc Treatment Options
The comforting part? Most cases get better without surgery. Many people recover through rest, exercise, and medical care that reduces inflammation and eases pressure on the nerves.
1. Non-surgical Treatments
The first step usually focuses on pain relief and gentle healing. Common herniated disc treatment options include:
-
Rest in moderation: short rest breaks, then gentle movement.
-
Pain medicines: Anti-inflammatory tablets or topical gels that reduce swelling.
-
Physiotherapy: Guided sessions with herniated disc exercises to rebuild strength and flexibility.
-
Hot and cold packs: Alternating between warm and cold compresses to relax muscles.
These steps often bring relief within a few weeks, especially when combined with posture correction and light stretching.
2. Injections
If pain lingers, your doctor might suggest a steroid injection near the affected nerve. It doesn’t cure the disc itself but calms inflammation and makes physiotherapy easier to continue.
3. Surgical Treatment
Surgery becomes an option only when pain stays strong despite other methods or when nerve compression is severe. The goal is simple: remove the part of the disc pressing on the nerve. Modern techniques are far less invasive now, which means shorter hospital stays and faster recovery.
Herniated Disc Exercises and Recovery Time
Once your pain settles, movement becomes your best friend. The right herniated disc exercises can strengthen your back muscles, improve flexibility, and help prevent another injury.
Here are some easy, commonly recommended moves:
-
Pelvic tilt: Tightens your lower back and core gently.
-
Knee-to-chest stretch: Relieves pressure on the lower spine.
-
Partial crunches: Strengthens your abs to support your back.
-
Cat-cow stretch: Keeps your spine flexible.
Always check with your physiotherapist before starting any exercise. They’ll make sure your form is safe and suited to your condition.
When it comes to herniated disc recovery time, it really depends on how your body heals. Some people feel better in 6 weeks; others take a few months. Mild cases tend to recover faster, especially if you follow your herniated disc exercises regularly.
Patience helps. Healing takes time, and rest is just as important as movement. Generally, herniated disc recovery time can range between six weeks and three months for mild conditions, sometimes longer for more complex cases.
Living with a Herniated Disc
It can be frustrating when your back keeps reminding you to slow down. But living with a herniated disc doesn’t have to mean giving up your normal life. With the right care and steady habits, you can move comfortably again.
Here are a few daily tips that make things easier:
-
Avoid lifting heavy items. If you must, bend your knees, not your waist.
-
Take regular breaks if you sit for long hours.
-
Keep your posture upright, whether you’re at a desk or walking.
-
Sleep on a supportive mattress that keeps your spine aligned.
-
Stay active, but don’t push through sharp pain.
Little things like these can shorten your herniated disc recovery time and reduce the chances of another flare-up.
Prevention and Daily Spine Care Tips
Even though ageing or genetics can’t be avoided, you can still take care of your back each day. The spine responds well to small, consistent habits.
Simple Tips for a Healthier Spine
|
Tip |
Description |
|
Stay active |
Choose low-impact workouts like swimming, yoga, or brisk walking |
|
Build core strength |
Strong abdominal muscles support your lower back |
|
Lift properly |
Use your legs, not your back, to lift objects |
|
Watch your sitting posture |
Keep your feet flat and shoulders relaxed |
|
Keep your weight balanced |
Extra kilos can strain your spine. |
|
Strech Often |
Epecially if your job keeps you seated for hours |
These gentle practices not only protect your spine but also reduce your chances of getting a herniated disc later in life.
When to See a Doctor
If your back pain isn’t improving, or if you notice tingling, weakness, or numbness spreading, it’s time to get checked. You should also seek help if you lose bladder or bowel control or feel pain shooting down your leg.
A specialist can design a herniated disc treatment plan that suits your body’s needs. The right help can stop the problem before it grows worse.
Conclusion
Back problems can test your patience, but a herniated disc doesn’t mean the end of comfort or movement. With the right care, awareness, and steady herniated disc exercises, recovery is absolutely possible.
If you or someone you know is facing long-term back pain, expert guidance makes all the difference. At Manipal Hospitals Bhubaneswar, specialists offer individualised herniated disc treatment focused on comfort, safety, and long-term healing.
Listen to your body, move carefully, and give it time. Healing is a journey, not a race.
FAQ's
The most common herniated disc symptoms are back or neck pain, tingling in your arms or legs, and sometimes muscle weakness. Some people feel a sharp pain that moves down one leg or arm. The level of pain can differ quite a bit, depending on where the disc is pressing on a nerve.
Gentle stretching, light yoga, and moves taught by a physiotherapist are some of the best herniated disc exercises. They strengthen your core, keep your back flexible, and improve posture. Always learn the exercises properly before doing them on your own.
Yes, with time and care, a herniated disc can often heal itself. The body slowly absorbs the bulging part, which takes pressure off the nerves. Gentle activity, good rest, and the right herniated disc treatment plan can help you recover naturally.
Surgery is usually the last option if pain, numbness, or weakness doesn’t get better after other herniated disc treatment methods. It may also be needed when nerve pressure affects walking or bladder control. Your doctor will advise you on what’s safest and most effective for you.
You can lower your risk by keeping your back strong and flexible through daily movement. Regular herniated disc exercises, correct posture, and careful lifting habits all make a big difference. Even small changes, like standing up more often and stretching, help protect your spine over time.






















 8 Min Read
8 Min Read

_need_Surgery__Expert_Guide_.png)











