Have you noticed persistent fatigue, occasional abdominal discomfort, or abnormal liver tests and wondered whether these signs could point to something serious in the liver? Fatty liver is a common condition that often begins quietly, and recognising the early fatty liver symptoms and understanding the usual fatty liver causes helps you and your clinician move from uncertainty to a clear plan for diagnosis and care. This blog explains what fatty liver disease is, how it develops, which symptoms and tests matter, and what practical steps you can take toward accurate diagnosis and effective management for fatty liver disease, including options for fatty liver treatment in Bhubaneshwar.
Synopsis
What is Fatty Liver Disease?
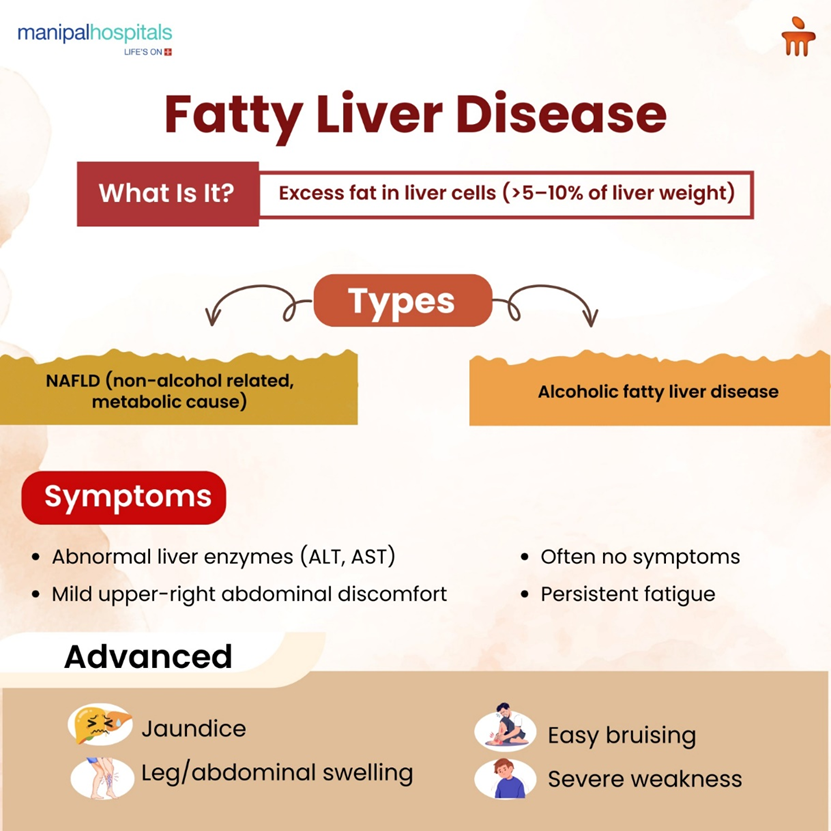
Fatty liver disease refers to excess fat stored in liver cells. When fat accounts for more than about 5–10 percent of liver weight, clinicians consider it fatty liver. There are two major types: nonalcoholic fatty liver disease (NAFLD), which is linked to metabolic factors such as excess weight and insulin resistance, and alcoholic fatty liver disease, caused by significant alcohol intake. NAFLD is now the most common form worldwide and often overlaps with fatty liver causes such as obesity, type 2 diabetes, high cholesterol, and a sedentary lifestyle.
Many people with early-stage fatty liver have no obvious problems. That is why routine blood tests or incidental findings on ultrasound often trigger further evaluation. Left unchecked, fatty liver can progress in some people to inflammation (steatohepatitis), fibrosis, and even cirrhosis, so early detection and management are important.
What Causes Fatty Liver?
Usually, metabolic factors dominate the list of fatty liver causes, but it's important to consider several contributors. Key causes include:
-
Metabolic syndrome features such as central obesity, insulin resistance, and high triglycerides
-
Type 2 diabetes, which increases the risk of fatty changes in the liver
-
Persistent excessive alcohol use
-
Certain medications, such as corticosteroids or some antiretrovirals
-
Rapid weight loss or malnutrition in specific situations
-
Certain genetic predispositions influence how the liver stores fat
-
Uncommon causes such as viral hepatitis or certain metabolic and endocrine disorders
When clinicians evaluate a patient, they assess lifestyle, medications, metabolic health, and alcohol use to identify the most likely fatty liver causes and rule out other liver disorders.
How Fatty Liver Problems Typically Present
Symptoms are often mild or absent in the early stages, which is why fatty liver symptoms are frequently overlooked. Nevertheless, there are consistent patterns clinicians watch for:
-
Persistent tiredness or low energy that does not match sleep or activity patterns
-
Discomfort or a dull ache in the upper right abdomen under the rib cage
-
Mild elevation of liver enzymes on routine blood tests, such as alanine aminotransferase (alt) or aspartate aminotransferase (ast)
-
Evidence of insulin resistance or metabolic syndrome, such as elevated fasting glucose, high triglycerides, or low hdl cholesterol
As the disease advances, signs related to liver dysfunction may appear, including easy bruising, swelling in the legs or abdomen, and jaundice. Such advanced signs indicate significant fibrosis or cirrhosis and require urgent specialist management. Most patients are identified early through clinic checks or investigations ordered for unrelated reasons.
Symptoms and Suggested Diagnostic Steps
|
Symptom or Findings |
What It Indicates | Suggested Diagnostic Step |
|
Fatigue with normal routine |
Possible early metabolic impact on the liver |
Check liver enzymes, fasting glucose, lipid profile |
|
Mild right upper quadrant discomfort |
Stretching of the liver capsule or mild inflammation |
Abdominal ultrasound and clinical exam |
|
Raised ALT/AST on routine blood tests |
Hepatocellular injury is common in NAFLD |
Repeat tests, screen for viral hepatitis, and ultrasound |
|
Metabolic syndrome (obesity, diabetes) |
High risk for NAFLD |
Evaluate for fatty liver with imaging and metabolic assessment |
|
Signs of advanced liver disease (jaundice, ascites) |
Possible fibrosis or cirrhosis |
Referral to hepatology for fibrosis assessment and management |
How Doctors Diagnose Fatty Liver Disease
Diagnosis combines history, examination, blood tests, and imaging, with liver biopsy reserved for specific questions. Doctors monitor for risk factors associated with progression, including older age, diabetes, severe obesity, elevated liver enzymes, and high fibrosis scores on noninvasive testing. Patients with significant fibrosis require closer follow-up and may be eligible for specialised therapies or clinical trials.
The usual diagnostic pathway includes:
-
History and physical: clinicians ask about alcohol intake, medications, metabolic conditions, and family history; an abdominal exam may detect liver enlargement.
-
Blood tests: liver enzymes (ALT, AST), full metabolic profile, fasting glucose or HbA1c, and lipid panel. Tests for viral hepatitis or autoimmune liver disease are ordered when indicated.
-
Imaging: Abdominal ultrasound is the common first-line imaging test because it detects moderate to severe steatosis and is widely available. Ultrasound cannot reliably stage fibrosis, however.
-
Fibrosis assessment: noninvasive scores (Fib-4, NAFLE fibrosis score) and elastography (transient elastography or shear wave elastography) check how stiff elastography is valuable to stratify who needs more intensive follow-up.
-
Liver biopsy: reserved when the diagnosis is uncertain or when staging inflammation and fibrosis will change management. Biopsy gives definitive histology but carries procedural risk and is not required in most patients.
This stepped approach helps target fatty liver treatment to the individual patient and avoids unnecessary invasive procedures.
Evidence-Based Fatty Liver Treatment Strategies
Management centers on treating the underlying fatty liver causes and reducing liver fat by addressing metabolic health. Core elements of fatty liver treatment include:
|
Weight loss |
Gradual, sustained weight reduction of 5 to 10 percent of body weight improves liver fat and inflammation; clinicians recommend combined dietary change and increased physical activity. |
| Improved glycemic control |
For patients with diabetes, optimising blood glucose with medication adjustments can reduce liver injury; certain diabetes medications also show liver benefits, and clinicians may select these agents when appropriate. |
| Lipid management |
Treating high triglycerides and low HDL according to cardiovascular risk, statins are safe in fatty liver and reduce cardiovascular risk. |
| Alcohol moderation or abstinence |
For patients with alcoholic fatty liver disease or mixed causes, reducing or stopping alcohol is essential. |
| Targeted therapies |
There is active research into drugs for NASH and fibrosis. Some agents are available in clinical trials or specialist centres and may be considered for patients with significant fibrosis. |
| Addressing comorbidities |
Effective treatment of hypertension, sleep apnea, and thyroid disorders supports liver health. |
Lifestyle measures remain the foundation of fatty liver treatment, and medications are tailored to individual risk profiles and disease stage.
Practical Steps You Can Take Now
If you suspect fatty liver disease or have risk factors, start with achievable steps: discuss testing with your clinician, aim for gradual weight loss if overweight, increase moderate-intensity physical activity to at least 150 minutes per week, reduce intake of refined sugars and saturated fats, and avoid unnecessary alcohol. Smoking cessation and control of diabetes and lipids are also priorities because cardiovascular disease is the leading cause of death in patients with fatty liver.
Conclusion
Recognising fatty liver symptoms and understanding the common fatty liver causes moves you from uncertainty to action. Early-stage fatty liver disease is reversible in many people with targeted lifestyle changes and medical care. Routine tests and ultrasound often uncover disease early; noninvasive fibrosis assessment guides the intensity of follow-up; and tailored fatty liver treatment focuses on weight management, metabolic control, and addressing alcohol use.
If you live in or near Bhubaneswar and need assessment or ongoing fatty liver treatment in Bhubaneswar, Manipal Hospital Bhubaneshwar offers specialist consultations, integrating with multidisciplinary teams so that your liver care is aligned with overall health goals.
FAQ's
Early fatty liver symptoms are often non-specific and can include persistent fatigue, mild discomfort in the upper right abdomen, and small unexplained elevations in liver enzymes on routine blood tests; many people have no symptoms, which is why screening is important when risk factors are present.
Fatty liver disease describes fat accumulation in the liver; when it is primarily caused by metabolic factors such as obesity and diabetes, it is termed nonalcoholic fatty liver disease (NAFLD), whereas alcoholic fatty liver results from significant alcohol intake; both lead to similar liver pathology, but the underlying causes and treatment priorities differ.
In many cases, early-stage fatty liver improves with sustained lifestyle changes, including gradual weight loss, improved pregnancy nutrition, and increased physical activity; for patients with advanced fibrosis, lifestyle changes are still important, but additional medical therapies and specialist input may be required.
Typical tests include measuring liver enzymes (ALT, AST), checking blood for metabolic issues (fasting glucose, lipids), doing an abdominal ultrasound, and using noninvasive methods to assess fibrosis like transient elastography; a liver biopsy is only done if the diagnosis or staging is still unclear
If you have risk factors such as obesity, diabetes, high triglycerides, or regular alcohol use, you should discuss screening and possible fatty liver treatment in Bhubaneswar with your clinician promptly, because early identification allows effective interventions that reduce the chance of progression to fibrosis or cirrhosis.






















 6 Min Read
6 Min Read















