Epilepsy is a common neurological condition. It causes recurrent seizures, and that fact alone often causes concern. But seizures are manageable. With modern epilepsy treatment, most people gain good seizure control and continue full, active lives. National Epilepsy Day in India (November 17) is a reminder: accurate diagnosis, the right treatment plan, and community support change outcomes. This blog explains what epilepsy is, how doctors diagnose it, the treatment choices available, and practical steps to live well.
Synopsis
- What Is Epilepsy?
- Common Types of Seizures
- How Doctors Make An Epilepsy Diagnosis?
- Treatment Options: Medicines, Devices, and Surgery
- Living with Epilepsy: Practical Steps and Everyday Life
- Seizure First Aid: What to Do When Someone Has A Seizure?
- Mental Health, Stigma, and Social Support
- When to See a Neurology Specialist?
- Why Early and Sustained Care Changes Outcomes
- Conclusion
What Is Epilepsy?
Epilepsy is defined by the tendency to have unprovoked seizures. Seizures happen when brain cells fire in an abnormal, excessive pattern. That electrical misfiring can cause loss of awareness, involuntary movements, changes in sensation, or brief staring spells. Causes vary. Some people have a clear trigger, such as a structural brain injury or genetic condition. For others, no specific cause is found. The label epilepsy doesn’t describe ability or life expectancy. It only describes a condition that needs attention and tailored care.
Common Types of Seizures
Seizures are not all the same. They fall into broad groups: focal seizures and generalized seizures.
-
Focal seizures start in one part of the brain. You may notice odd feelings, lip smacking, or movement limited to one limb. Consciousness may be preserved or impaired.
-
Generalized seizures involve both sides of the brain from the start. Tonic-clonic seizures, the kind with stiffening and jerking, are the most visible. Absence seizures look like brief staring spells and often occur in children.
Epilepsy symptoms can be subtle. A short period of confusion, sudden dizziness, or unusual taste can be seizure signs. If you recognise repeated unusual events, note details, timing, triggers, duration, and discuss them with a neurologist.
How Doctors Make An Epilepsy Diagnosis?
Diagnosis relies on careful history and targeted tests. A single seizure doesn’t always mean epilepsy. Recurrent, unprovoked seizures do.
A typical evaluation includes:
-
Detailed clinical history, often with eyewitness description of events
-
Neurological examination
-
An electroencephalogram (EEG) to detect abnormal brain electrical activity
-
Neuroimaging with MRI, to look for structural causes
-
Blood tests to rule out metabolic or infectious triggers
Advanced tests, ambulatory EEG, video-EEG monitoring, or specialised MRI protocols are used when the diagnosis is uncertain or when considering surgery. Accurate epilepsy diagnosis guides a clear treatment strategy and reduces unnecessary worry.
Treatment Options: Medicines, Devices, and Surgery
The first-line treatment for most people is medication. Anti-seizure medications (ASMs) control seizures for many. Selection depends on seizure type, age, sex, coexisting conditions, and potential side effects. With the right drug and dose, many people achieve long-term seizure freedom.
When seizures persist despite appropriate medicines, other options exist:
|
Medication adjustment |
Changing drugs or combining agents under specialist supervision. |
|
Ketogenic diet |
A high-fat, low-carbohydrate diet helps particular types of epilepsy, especially in children. |
|
Neurostimulation |
Vagus nerve stimulation (VNS) or responsive neurostimulation (RNS) reduces seizure frequency in selected cases. |
|
Epilepsy surgery |
For focal seizures arising from a well-defined area, surgery can remove or disconnect the focus and achieve a cure or a major reduction in seizures. Pre-surgical evaluation is thorough and multidisciplinary. |
Each option has benefits and risks. A neurologist explains the likely outcome and the most suitable path for you.
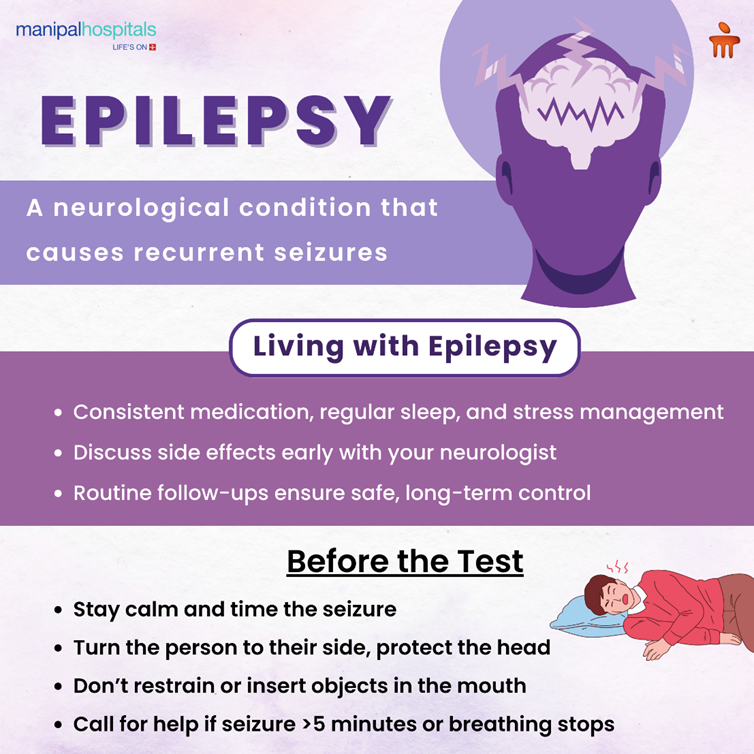
Living with Epilepsy: Practical Steps and Everyday Life
Seizures can affect daily routines, but careful planning restores confidence.
-
Medication adherence is essential. Skipping doses increases seizure risk. Regular follow-up helps adjust doses, monitor side effects, and check interactions with other medicines.
-
Sleep, stress management, and regular meal patterns also influence seizure control. Poor sleep and missed meals are common seizure triggers. Aim for consistent routines.
-
Work and education plans adapt to individual needs. Disclosure choices vary; some prefer to inform employers or teachers, others share only when necessary. Laws and workplace policies differ, but many people with epilepsy work successfully across professions.
-
Driving regulations exist to protect everyone. Local rules determine when driving may resume after seizure freedom; follow the legal requirements and guidance from your neurologist.
Seizure First Aid: What to Do When Someone Has A Seizure?
Knowing seizure first aid is empowering. Follow these steps if someone has a convulsive seizure:
-
Stay calm and time the seizure.
-
Place the person on their side to protect the airway once convulsions stop.
-
Cushion the head; remove nearby dangerous objects.
-
Do not restrain movements or put anything in the mouth.
-
Call emergency services if the seizure lasts more than five minutes, if breathing doesn’t resume, if repeated seizures occur without recovery in between, or if injury occurs.
-
Reassure the person as they regain awareness and stay with them until they are fully alert.
Basic knowledge reduces panic and improves safety. Consider sharing seizure first aid training with family, colleagues, and teachers.
Mental Health, Stigma, and Social Support
Epilepsy affects emotions as well as the body. Anxiety, depression, and social isolation are common but treatable. Mental health support is an essential part of care. Talk openly about mood changes and seek help early.
Stigma remains a barrier in many communities. Misconceptions about epilepsy can limit opportunities and increase isolation. Education reduces fear. Encourage informed conversation at home, work, and school. Accurate information from a neurologist helps peers and colleagues understand the condition and provide meaningful support.
When to See a Neurology Specialist?
If seizures occur, consult neurology without delay. Early specialist involvement improves outcomes, especially when seizures continue despite initial treatment. Expect a thorough assessment, tests to define seizure type and cause, and a personalised management plan. If surgery or advanced therapies are under consideration, the team will explain the evidence, the process, and the likely benefits and risks.
Why Early and Sustained Care Changes Outcomes
Early diagnosis and consistent treatment reduce seizure frequency and the risk of injury. Many people reach long-term seizure freedom with first-line medicines. Others achieve major improvement with diet, neurostimulation, or surgery. Delays in assessment or interrupted care increase the chance of uncontrolled seizures and complications. Regular follow-up, adherence to therapy, and open communication with your neurologist make a measurable difference.
Conclusion
Epilepsy is a medical condition with clear pathways to control. Modern epilepsy treatment, when guided by an accurate epilepsy diagnosis, helps most people lead independent lives. Knowing seizure first aid, maintaining treatment routines, and seeking specialist care when seizures persist are practical steps that matter. Please remember this: Epilepsy doesn’t define ability or future prospects. With the right medical team and community support, life continues with purpose and possibility.
If you or someone you know needs evaluation, the neurology team at Manipal Hospital Bhubaneswar offers comprehensive assessment, EEG and neuroimaging services, and access to medical, dietary, stimulation, and surgical options. Book a neurology appointment at Manipal Hospitals, Bhubaneswar. Early assessment saves time and improves outcomes.
FAQ's
Not necessarily. A single unprovoked seizure requires evaluation, but a diagnosis of epilepsy usually follows two or more unprovoked seizures or a single seizure plus a high risk of recurrence based on tests.
Many people achieve full seizure control with the right medication and dose. Others may need adjustments, combinations, or alternative treatments. Regular follow-up helps optimise results.
Yes. With seizure control, most people work, marry, and raise families successfully. Safety considerations and local regulations (for example, driving rules) affect specific choices, but epilepsy itself isn’t a barrier to a fulfilling life.
Call emergency services if a convulsive seizure lasts more than five minutes, if another seizure follows immediately, if the person doesn’t start breathing normally after the seizure, if injury occurs, or if the person is pregnant or has diabetes.
Epilepsy is not contagious. Some forms have genetic links, while others result from brain injury or unknown causes. Family history may increase risk, but it doesn’t always mean that a child will develop epilepsy.






















 6 Min Read
6 Min Read


















