Have you ever wondered why one kind of cholesterol is called “good” and another “bad”? Understanding what is cholesterol and the difference between HDL vs LDL cholesterol matters because those simple labels guide prevention and treatment choices that protect the heart. In plain language: cholesterol itself is not the enemy; it is a fat-like substance the body needs, but the balance between different types determines whether it helps or harms. This blog explains good cholesterol vs bad cholesterol, why the difference matters for heart risk, how tests work, and practical steps to manage levels for long-term health.
Synopsis
- What Is Cholesterol?
- LDL and HDL
- Why the Difference Between Good and Bad Cholesterol Matters
- How Cholesterol Is Measured - What The Numbers Mean
- Typical Cholesterol Targets (General Guide)
- Common Causes Of High LDL And Low HDL
- How to Lower Bad Cholesterol and Improve Good Cholesterol
- When Medication Is Needed
- Conclusion
What Is Cholesterol?
Cholesterol is a waxy molecule produced by the liver and carried in the blood inside particles called lipoproteins. The body uses cholesterol to build cell walls, make hormones, and create vitamin D. Problems start when too much cholesterol travels in the wrong carriers and deposits inside artery walls, forming plaques that narrow vessels and reduce blood flow.
LDL and HDL
Clinicians explain cholesterol in terms of carriers:
-
LDL (low-density lipoprotein) is commonly called “bad cholesterol” because high LDL levels are linked to plaque build-up and heart disease.
-
HDL (high-density lipoprotein) is called “good cholesterol” since it helps remove cholesterol from artery walls and carries it back to the liver for disposal.
When comparing LDL vs. HDL cholesterol, the goal is to keep LDL levels low and HDL at a healthy level. The risk comes mainly from high LDL, especially small, dense LDL particles, which promote plaque build-up in the arteries and increase the chance of heart disease. This is why LDL is commonly referred to as “bad cholesterol.”
Why the Difference Between Good and Bad Cholesterol Matters
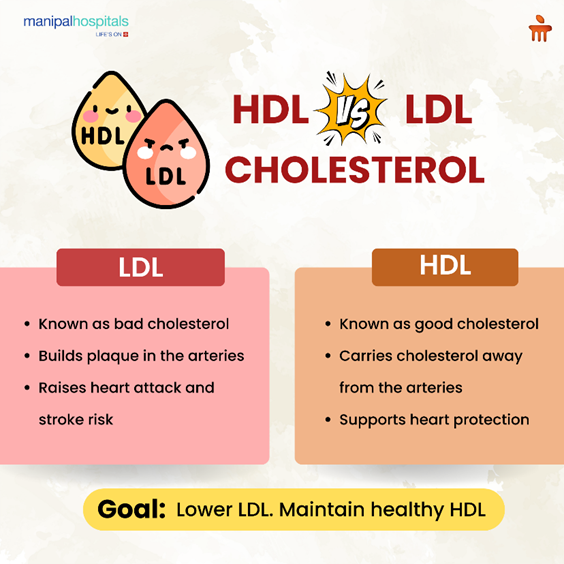
Thinking about good vs bad cholesterol is useful because it turns abstract lab numbers into action. High LDL (bad cholesterol) increases the chance of plaque formation, heart attack, and stroke. Higher HDL (good cholesterol) is associated with lower risk, although HDL-raising drugs have not always reduced events. The safe path is a combined approach: lower LDL, improve lifestyle, and manage other risks such as blood pressure and diabetes.
In practical terms, clinicians focus on cholesterol management for heart health because lowering LDL with diet, exercise, and, when needed, statin treatment clearly reduces cardiovascular events. HDL vs LDL cholesterol matters mostly because it helps identify who needs treatment and how aggressive that therapy should be.
How Cholesterol Is Measured - What The Numbers Mean
A standard lipid profile usually reports:
-
Total cholesterol.
-
LDL cholesterol (the “bad” number).
-
HDL cholesterol (the “good” number).
-
Triglycerides (another fat linked to risk).
Target numbers depend on overall heart risk. For people at high risk (previous heart attack, diabetes), doctors aim for lower LDL levels than for someone with no risk factors. Remember that tests are one snapshot, trends over time, and how numbers change with lifestyle or medication matter more than a single reading.
Typical Cholesterol Targets (General Guide)
Consider the following ranges:
|
Measure |
Desirable (general) |
Notes |
|
LDL (bad cholesterol) |
Less than 100 mg/dL (lower if high risk) |
Primary target to reduce heart risk |
|
HDL (good cholesterol) |
40 mg/dL or higher (men), 50 mg/dL or higher (women) |
Higher is generally better |
|
Total cholesterol |
Less than 200 mg/dL |
Combines LDL, HDL and others |
|
Triglycerides |
Less than 150 mg/dL |
High levels often accompany low HDL |
Common Causes Of High LDL And Low HDL
Several factors influence the balance of good vs bad cholesterol:
-
A diet high in saturated and trans fats raises LDL.
-
A sedentary lifestyle lowers HDL and raises triglycerides.
-
Smoking reduces HDL and worsens overall risk.
-
Genetics: Some people inherit high LDL (familial hypercholesterolemia) and need aggressive treatment.
-
Conditions such as obesity, poorly controlled type 2 diabetes, and hypothyroidism affect lipid levels.
Understanding causes helps tailor cholesterol management for heart health rather than using one-size-fits-all advice.
How to Lower Bad Cholesterol and Improve Good Cholesterol
Simple, evidence-based steps help most people:
-
Follow a heart-healthy eating plan. Diets rich in vegetables, whole grains, legumes, nuts, fish, and healthy oils lower LDL. For many, a Mediterranean-style diet or targeted steps like a diet to lower LDL cholesterol (reduce saturated fat, remove trans fats, increase soluble fibre) are effective.
-
Increase physical activity. Regular aerobic exercise raises HDL and lowers triglycerides. Supervised programs and brisk walking are practical starting points.
-
Quit smoking. Smoking cessation rapidly improves HDL and reduces cardiovascular risk.
-
Maintain a healthy weight. Losing excess weight helps both LDL and HDL and lowers triglycerides.
-
Consider medications when lifestyle is insufficient. Statins are the first-line drugs to lower LDL and have a strong track record of preventing heart attacks and strokes.
A few tips you can try:
-
If diet is the main focus, try increasing soluble fibre (oats, beans) and adding fatty fish twice weekly.
-
To raise HDL naturally, encourage regular aerobic exercise and smoking cessation, and consider how to raise HDL organically by combining movement and healthy fats.
-
If family history shows very high LDL, discuss early medical therapy; this is not a “diet-only” situation.
When Medication Is Needed
Lifestyle changes help most, but medication is common and evidence-based for many people:
-
Statins reduce LDL and lower the chance of a heart attack and stroke. They are recommended for people with existing heart disease, diabetes, over a certain age, or with very high LDL levels.
-
Additional drugs (ezetimibe, PCSK9 inhibitors) may be added when LDL remains high despite statins or when genetic forms of high cholesterol are present.
-
Doctors choose therapy based on overall cardiovascular risk; cholesterol numbers alone are part of that assessment.
Medication decisions are personalised. The aim is not to chase a single number but to reduce the chance of heart events over the coming years. If you search for the best heart hospital in Salem or the best heart hospital near me, prioritise centres that offer comprehensive lipid clinics, cardiac risk assessment, and long-term follow-up.
Lifestyle Is Not Optional
Even when medications are used, lifestyle steps make treatment more effective and often allow lower doses. Combining diet to lower LDL cholesterol, regular exercise, weight control, and stopping smoking reduces both LDL and overall cardiovascular risk. That combination is the cornerstone of cholesterol management for heart health.
FAQ's
When people ask what bad cholesterol is, they usually mean LDL cholesterol; high levels increase plaque and heart risk.
What is cholesterol used for? It helps build cells, make hormones, and support vitamin D production. It is essential, but balance matters.
For LDL vs HDL cholesterol, concentrate on diet to lower LDL cholesterol (less saturated fat, more fibre) and how to raise HDL naturally (exercise, stop smoking, healthy fats).
No. One high number prompts further checks and a discussion of risk factors. Trends and overall heart risk determine treatment.
If someone searches for a heart hospital in Salem or the best heart hospital near me, choose a centre with cardiology clinics that offer lipid management, risk assessment, and access to advanced therapies.





















 7 Min Read
7 Min Read

__Its_Type_and_Benefits.png)