A small, painful lump near the vagina is upsetting and often feels embarrassing. Vaginal boils are common, usually treatable skin infections that cause a red, tender, pus-filled lump on the vulva or around the labia. Most boil episodes resolve with basic care and simple treatments, but some require medical procedures or medicines. Knowing the likely causes, how doctors assess the problem, effective vaginal boils treatment, and safe home remedies helps you act quickly and avoid complications. This blog explains what to watch for, what you can do at home to ease discomfort, and when you must see a clinician.
Synopsis
What are Vaginal Boils?
A vaginal boil is a localised skin infection that begins in a hair follicle or oil gland and forms a tender, pus-filled lump. These lumps can appear on the vulva, labia, or near the perineum. A boil is also called a furuncle if it involves a single hair follicle, and multiple linked boils are known as carbuncles. Boils are usually caused by bacteria that enter the skin through minor breaks. You can feel a boil as a firm, painful nodule that becomes softer as pus accumulates.
Common Causes
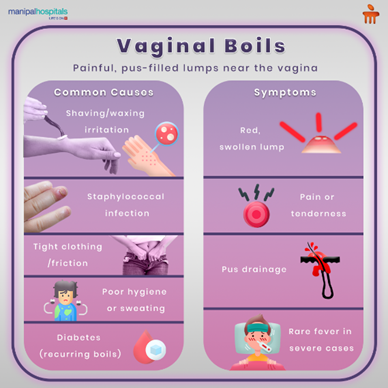
Understanding the usual triggers helps you take targeted steps to reduce risk and manage a current episode. Many causes are preventable or treatable.
-
Shaving irritation from razors or waxing can damage the skin and allow bacteria to enter.
-
Staphylococcal infection, especially by Staphylococcus aureus, is the most common bacterial cause of boils.
-
Tight clothing or repeated friction can rub the skin and create tiny breaks.
-
Poor hygiene or heavy sweating encourages bacterial growth in warm, moist folds.
-
Diabetes, especially when blood sugar is not well controlled, increases the risk of recurrent boils.
-
Trauma to the area, such as insect bites or minor cuts, can be an entry point for bacteria.
Symptoms
Boils have recognisable features that help you and your doctor identify them early. Symptoms often develop in stages and may change over a few days.
-
Red, swollen lump that is painful or tender to touch.
-
Pus drainage from the lump as it comes to a head.
-
Local warmth and increasing tenderness.
-
A rare fever or feeling unwell occurs when the infection is more severe or spreading.
-
In some cases, repeated boils in the same area suggest an underlying risk such as diabetes or skin carriage of Staphylococcus.
If you notice sudden swelling, rapid increase in pain, fever, or spread of redness beyond the immediate area, seek medical attention.
How Doctors Assess Vaginal Boils
When you see a clinician, the first step is a careful history and physical examination to confirm the diagnosis and to look for factors that increase risk. Your doctor will ask about recent shaving or waxing, prior similar lumps, diabetes or other chronic illnesses, sexual activity, and any new products you used on the skin. Examination focuses on the size, location, and tenderness of the boil and whether nearby lymph nodes are enlarged.
Simple tests help guide treatment when needed. These may include:
-
A swab of pus for culture to identify the bacteria and to check antibiotic sensitivity.
-
Blood sugar tests are done if boils recur or if you have symptoms suggesting diabetes.
-
Imaging is only performed in rare cases where a deep abscess or spread beneath the skin is suspected.
Treatment Options
Most small boils improve with local care, but some need medical procedures or antibiotics. Treatment aims to relieve pain, drain pus safely when required, and remove the cause so recurrence is less likely.
-
Warm compresses and sitz baths help the boil come to a head and drain naturally while easing pain. Apply warmth for 10 to 15 minutes several times daily.
-
Incision and drainage performed by a clinician may be necessary for larger or persistent boils. This procedure is done under sterile conditions to remove pus safely and promote healing. This is the usual incision and drainage approach for sizeable abscesses.
-
Antibiotics may be prescribed when there is spreading redness, systemic symptoms such as fever, multiple boils, or if culture shows bacteria sensitive to specific drugs. Take the full course exactly as directed.
-
Topical antiseptic washes can reduce local bacterial load when advised by your doctor.
-
Avoid overusing harsh antiseptics that damage healthy skin.
-
Pain relief with paracetamol or nonsteroidal anti-inflammatory drugs helps comfort while the boil resolves. Use medicines according to dosing guidance and medical advice.
For recurrent infections, decolonisation strategies such as topical mupirocin inside the nostrils and chlorhexidine washes may be recommended by your clinician after tests confirm staphylococcal carriage.
Home Remedies That Help
Careful home measures ease pain and support healing while avoiding practices that make the problem worse. These steps are supportive and not substitutes for medical care when the boil is large, spreading, or accompanied by fever.
-
Use warm compresses or sitz baths two to three times daily to soften the lump and promote drainage. Ensure the water is comfortably warm and clean.
-
Keep the area clean with gentle, unscented soap and water. Pat dry, do not rub.
-
Apply sterile gauze to catch any discharge and change dressings frequently.
-
Wear breathable cotton underwear and loose clothing to reduce friction.
-
Avoid squeezing, popping, or attempting DIY drainage. This can push the infection deeper and increase scarring.
-
Stop shaving, waxing, or using hair removal creams on the area until fully healed. Consider trimming rather than shaving while healing.
-
If you use topical antiseptic creams, follow your clinician’s advice. Avoid home use of strong chemicals that irritate the skin.
When to Seek Medical Help
Most boils resolve with simple care, but some signs mean you should see a clinician promptly or go to emergency care. Early medical attention reduces the risk of spread and serious complications.
-
Rapidly increasing redness or pain extending away from the boil.
-
Fever or feeling generally unwell.
-
A boil that does not improve after several days of warm compresses or that enlarges.
-
Recurrent boils in the same area or several boils at once.
-
Any drainage that smells very foul or is accompanied by increasing swelling beneath the skin.
-
Difficulty walking or sitting because of pain.
If you have diabetes or a weakened immune system, seek care sooner because infections can progress more quickly.
Preventing Vaginal Boils
Prevention focuses on reducing friction, avoiding skin breaks, and limiting bacterial colonisation. Small changes in grooming and hygiene significantly reduce recurrence risk.
-
Prefer trimming to shaving and use a clean, sharp razor if you must shave. Shave in the direction of hair growth and use a gentle lubricant.
-
Avoid tight synthetic clothing that traps sweat. Choose breathable cotton for underwear.
-
Keep the groin area clean and dry, especially after exercise. Change out of wet clothes promptly.
-
Avoid scented products, harsh soaps, and douches that irritate fragile skin.
If you have frequent boils, have your blood sugar checked and discuss decolonisation and long-term strategies with your clinician.
Conclusion
Most vaginal boils are painful but treatable. With careful hygiene, warm compresses, and timely medical care, you can expect healing within days to a few weeks. Larger or recurrent boils require clinician care, which may include incision and drainage, appropriate antibiotics, and strategies to reduce recurrence, especially if diabetes is a factor. Use safe home remedies for comfort, avoid squeezing the lump, and seek prompt medical review for worsening pain, fever, or repeat episodes. With timely action, you can resolve the infection and reduce the chance of it coming back.
If you notice persistent pain, swelling, recurring boils, or signs of infection, consult a specialist for timely evaluation and treatment. Book an appointment with a Manipal Hospitals expert to receive safe and reliable care.
FAQ's
No. You should not squeeze or pop a boil. Doing so can push infection deeper, cause scarring, and spread bacteria. See a clinician for safe drainage if needed.
Small boils often improve in 3 to 7 days with warm compresses. Larger boils that require drainage may take 1 to 3 weeks to fully heal. Follow up if healing is slow.
The bacteria that cause boils can be passed by direct contact, but most cases relate to your own skin flora and local skin breaks. Maintain hygiene and avoid sharing towels if you have an active boil.
Most boils are not STIs. However, if you have unusual discharge, genital ulcers, or other concerning symptoms, get tested for STIs to rule out other causes.
If you have repeated boils in the same area, see your doctor. Recurrent infections may need testing for staphylococcal carriage, blood sugar screening for diabetes, and specialist advice for prevention.




















10.png)
 6 Min Read
6 Min Read








8.png)