Life is busy, and many common signs are easy to shrug off as tiredness or a busy week. Diabetes is a long-term condition that affects how your body handles blood sugar, and early detection changes outcomes. You will learn to recognise the typical diabetes symptoms, understand the main causes, and see clear, evidence-based diabetes treatment options and diabetes prevention tips that you can discuss with your doctor.
Synopsis
- What Is Diabetes
- Types of Diabetes
- Recognising Diabetes Symptoms
- Why Early Diagnosis Matters
- Common Causes and Risk Factors
- How Diabetes is Diagnosed
- Diabetes Treatment Options
- Practical Lifestyle Steps You Can Start Today
- Monitoring and Follow-up
- When to Seek Urgent Care
- Preventing Diabetes
- Questions to Ask Your Doctor
- Conclusion
What Is Diabetes
Diabetes is a condition in which the body cannot regulate blood sugar properly. Insulin is the hormone that helps move sugar from the bloodstream into cells for energy. When insulin is missing, insufficient, or the body does not respond well to it, blood sugar rises. Over time, high blood sugar can harm the heart, kidneys, eyes, and nerves. Understanding the basic problem helps you see why testing, treatment, and lifestyle matter.
Types of Diabetes
There are different forms of diabetes, and each needs a distinct approach.
Type 1 Diabetes
Type 1 diabetes occurs when the immune system attacks the insulin-producing cells in the pancreas and stops them from working. People with this condition need insulin therapy because their bodies make little or no insulin.
Type 2 Diabetes
Type 2 diabetes happens when the body becomes less sensitive to insulin or does not make enough of it. It is more common in adults but increasingly seen in younger people. Lifestyle changes and medicines are the mainstay of treatment for many people with type 2 diabetes.
Other Types
There are other, less common types, such as gestational diabetes during pregnancy and forms caused by rare genetic conditions. For any type, early diagnosis and a clear plan help reduce complications.
Recognising Diabetes Symptoms
Knowing typical diabetes symptoms helps you seek tests early. Symptoms can be subtle at first and build over time.
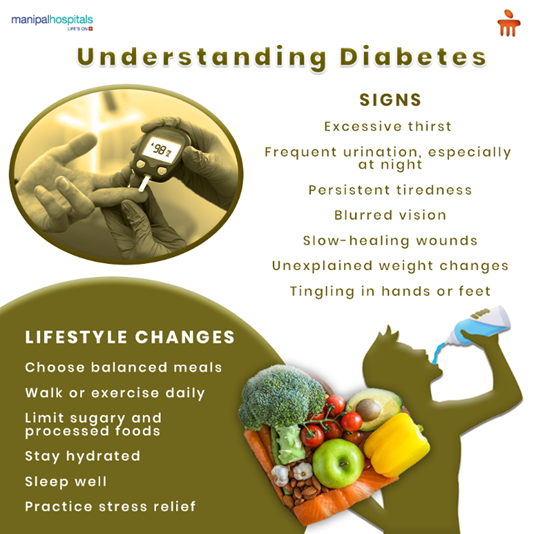
Common symptoms include:
-
Frequent urination, especially waking at night to pass urine.
-
Excess thirst, the feeling of needing to drink more than usual.
-
Blurry vision or changes in eyesight.
-
Fatigue that is not explained by sleep loss.
-
Increased hunger or weight change, including unintentional weight loss.
-
Slow wound healing, with cuts or infections that take longer to settle.
If you notice more than one of these signs, or the symptoms come on quickly, arrange a check with your doctor for diabetes diagnosis tests.
Why Early Diagnosis Matters
Catching diabetes early reduces the risk of serious complications. Treating high blood sugar promptly lowers the chance of heart disease, kidney damage, vision loss, and nerve problems. Early diagnosis also gives you a chance to use lifestyle measures effectively and to start medications that protect organs. For many people, a timely diagnosis makes long-term control simpler and more effective.
Common Causes and Risk Factors
Understanding causes helps you target prevention and screening. Some causes are unavoidable, while others relate to lifestyle.
Key risk factors include:
-
Family history of diabetes or strong genetic predisposition.
-
Overweight and central fat around the waist.
-
Low physical activity.
-
Unhealthy diet high in processed foods and sugars.
-
Age, with a higher risk as people grow older, for type 2 diabetes.
-
Certain medical conditions, such as high blood pressure or abnormal cholesterol.
-
Pregnancy-related glucose intolerance that can lead to gestational diabetes.
If you have multiple risk factors, ask your doctor about regular blood sugar monitoring and personalised diabetes prevention tips.
How Diabetes is Diagnosed
Doctors use simple blood tests for diabetes diagnosis. These are routine and widely available.
Common tests include:
-
Fasting plasma glucose, measured after an overnight fast.
-
An oral glucose tolerance test, which checks blood sugar two hours after a glucose drink.
-
Haemoglobin A1c, which estimates average blood sugar over the past two to three months.
-
Random blood glucose if symptoms are present.
Your clinician will explain which test is most appropriate based on symptoms and context. A confirmed diagnosis usually requires repeat testing or a combination of results.
Diabetes Treatment Options
Treatment is tailored to the type of diabetes and to your individual needs. Goals are to normalise blood sugar, relieve symptoms, and prevent complications.
Lifestyle Measures
Lifestyle is the foundation of care for most people with diabetes. A steady, balanced diet, regular physical activity, and weight optimisation improve blood sugar control and often reduce medicine requirements.
Medicines for Type 2 Diabetes
A range of oral and injectable medicines helps lower blood sugar in type 2 diabetes. Your doctor selects drugs based on overall health, heart and kidney risk, and how high your blood sugar is.
Insulin Therapy
People with type 1 diabetes require insulin therapy. Some people with type 2 diabetes also need insulin when other measures are insufficient. Insulin comes in several forms with different durations of action, and your diabetes team will help you choose the right regimen.
Monitoring and Support
Regular blood sugar monitoring helps you see how diet, activity, and medicines affect glucose. Many people use fingerstick testing or continuous glucose monitoring when recommended. Education, diabetes nursing support, and a dietitian’s guidance improve outcomes.
Treating Complications
If complications appear, specific treatments target the organs involved, such as eye checks and kidney monitoring. Early action keeps complications manageable.
Practical Lifestyle Steps You Can Start Today
Small, consistent changes often make the biggest difference. These steps help both prevention and long-term control.
-
Move daily. Aim for moderate aerobic activity most days and include some strength training twice weekly.
-
Choose whole foods by including whole grains, vegetables, legumes, lean proteins, and healthy fats in your daily diet.
-
Watch portion sizes. Avoid frequent high-sugar snacks and sugary drinks.
-
Lose weight if advised. Losing even a small amount of excess weight improves insulin sensitivity.
-
Limit alcohol and avoid smoking. Both increase cardiovascular risk and complicate diabetes care.
-
Keep regular medical follow-up and do the recommended screening tests.
Monitoring and Follow-up
Monitoring helps you and your clinician adjust diabetes treatment options over time. Regular checks also pick up complications early.
Monitoring includes:
-
Regular blood sugar monitoring as advised, including HbA1c tests every few months.
-
Blood pressure and cholesterol checks to lower heart risk.
-
Kidney function tests and urine checks for protein.
-
Regular eye checks for retinopathy and foot checks for nerve or circulation problems.
A clear follow-up plan reduces anxiety and improves long-term health.
When to Seek Urgent Care
Some symptoms need prompt attention because they may signal dangerously high or low blood sugar or an acute complication.
Look for these signs and get urgent care if they occur:
-
Severe breathlessness, chest pain, or sudden confusion.
-
Very high blood sugar with vomiting and abdominal pain, which may indicate diabetic ketoacidosis in type 1 diabetes.
-
Very low blood sugar with fainting, seizures, or prolonged inability to swallow.
-
Sudden vision loss or severe leg pain with pale skin and cold extremities.
-
Timely emergency care can be life-saving and prevent lasting harm.
Preventing Diabetes
For many people, preventing type 2 diabetes is possible with sustained changes. Interventions that reduce weight and increase activity are the most powerful.
Core prevention tips include:
-
Aim for regular physical activity and reduce sedentary time.
-
Maintain a balanced diet rich in fibre, vegetables, and lean protein.
-
Keep a healthy weight and lose weight if overweight.
-
Monitor blood sugar if you have risk factors and follow your doctor’s recommendations.
-
Manage blood pressure and lipids to reduce overall cardiovascular risk.
These diabetes prevention tips are realistic and effective when followed consistently.
Questions to Ask Your Doctor
When you get a diagnosis or a test result, these questions help you get clear next steps and a plan that fits your life.
-
Which type of diabetes do I have, and how was this determined?
-
What are my target blood sugar numbers, and how often should I check?
-
Which diabetes treatment options do you recommend first and why?
-
Do I need a referral to a specialist, dietitian, or diabetes educator?
-
What lifestyle changes will be most helpful for me right now?
Conclusion
Diabetes can be effectively managed when identified early and treated wisely. By recognising the signs, understanding your risk factors, choosing the right treatment options, and following simple prevention strategies, you can take strong control of your health. Partner with your doctor to build a personalised plan that suits your lifestyle. With consistent care, you can minimise complications and maintain long-term well-being.
Take the next step toward better diabetes management—consult Manipal Hospitals today.
FAQ's
A combination of fasting glucose, oral glucose tolerance test, or haemoglobin A1c is used for diabetes diagnosis. Your clinician will advise which test is most suitable.
In many people, early and sustained weight loss plus activity can put type 2 diabetes into remission or reduce medicine needs. Ongoing follow-up is essential.
No. Insulin therapy is required for people with type 1 diabetes and for some with type 2 diabetes. Many people with type 2 diabetes start with lifestyle changes and oral medicines.
No. Insulin therapy is required for people with type 1 diabetes and for some with type 2 diabetes. Many people with type 2 diabetes start with lifestyle changes and oral medicines.
No. Insulin therapy is required for people with type 1 diabetes and for some with type 2 diabetes. Many people with type 2 diabetes start with lifestyle changes and oral medicines.
No. Insulin therapy is required for people with type 1 diabetes and for some with type 2 diabetes. Many people with type 2 diabetes start with lifestyle changes and oral medicines.
This depends on your treatment. People on insulin often check several times daily. Others on oral medicines may check less frequently. Discuss a plan for blood sugar monitoring with your clinician.
Regular activity, a balanced diet, weight control, avoiding smoking, and limiting alcohol are the most effective diabetes prevention tips.




















8.png)
 7 Min Read
7 Min Read




10.png)