
Fever is the body’s common alarm. Most fevers are short-lived and harmless, but sometimes a high or persistent fever signals a serious condition. Acute febrile illness or AFI is a broad term for illnesses that cause sudden fever and may progress rapidly. Timely recognition and early diagnosis can be life-saving because they allow treatment before complications such as sepsis or organ dysfunction develop. This article explains common fever causes, how doctors diagnose AFI quickly, what treatments you may be offered, and clear signs that mean you should seek urgent medical care.
Synopsis
- What is Acute Febrile Illness
- Why Early Diagnosis Matters
- Common Causes
- How AFI Becomes Dangerous
- Signs to Watch For
- How Doctors Diagnose AFI
- Early Diagnostic Tests You May Be Offered
- Immediate Management and Treatment
- When to Seek Emergency Care
- Hospital Admission Criteria
- Prevention and Public Health Measures
- Practical tips for caregivers
- Conclusion
What is Acute Febrile Illness
Acute febrile illness refers to any condition that causes a recent onset of fever, typically within days, and often with other symptoms such as headache, body aches, or gastrointestinal upset. AFI is a working diagnosis used by clinicians to prompt targeted testing. Because the causes range from self-limited viral infections to treatable bacterial or parasitic diseases, identifying the cause early matters for choosing the right therapy.
Why Early Diagnosis Matters
Early diagnosis changes the outcome because some causes of AFI respond to specific, time-sensitive treatments. Identifying treatable infections quickly reduces the chance of complications such as sepsis, organ failure, or prolonged hospital stay. In outbreaks and in areas with high prevalence of vector-borne diseases, rapid diagnosis also helps public health responses and prevents spread to others. For you, a prompt diagnosis means a clearer treatment plan and usually faster recovery.
Common Causes
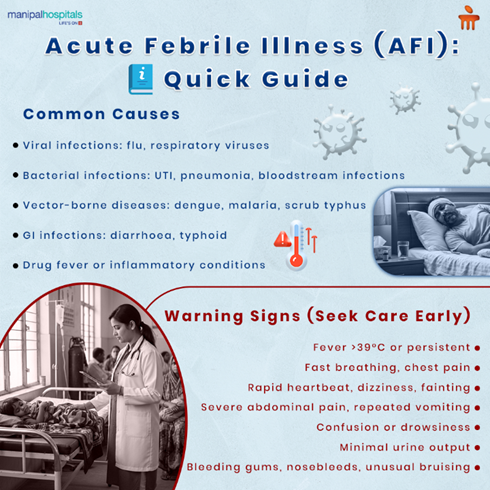
Acute fever can come from many sources. The likely cause depends on geography, exposures, season, and any underlying health problems.
-
Viral infections, such as influenza or other respiratory viruses.
-
Bacterial infections, including urinary tract infections, pneumonia, and bloodstream infections.
-
Vector-borne diseases, such as dengue, malaria, or scrub typhus, are endemic in certain areas.
-
Gastrointestinal infections that cause fever along with diarrhoea or vomiting.
-
Drug fever or inflammatory conditions that present with sudden fever.
-
Less commonly, early presentations of autoimmune disease or malignancy.
Your doctor will weigh these possibilities based on your history and local patterns of disease.
How AFI Becomes Dangerous
Most fevers settle with time or simple treatment, but AFI becomes dangerous when the infection spreads or the immune response becomes harmful. Sepsis is one severe pathway where infection triggers widespread inflammation and organ dysfunction. Dehydration, delayed treatment of bacterial infections, or underlying chronic disease such as diabetes can also turn a routine fever into a critical illness. Recognising warning signs early prevents progression.
Signs to Watch For
Knowing when fever is just fever and when it may be serious helps you act quickly. Pay attention to the pattern and associated features:
-
High fever that does not fall with usual measures or returns rapidly after treatment.
-
Rapid breathing, difficulty breathing, or chest pain.
-
Fast heart rate, dizziness, or fainting.
-
Severe abdominal pain, persistent vomiting, or inability to keep fluids down.
-
Confusion, drowsiness, or new neurological symptoms such as weakness.
-
Little or no urine output, or signs of dehydration.
-
Bleeding from gums, nose, or unusual bruising, which can be a sign of some infections.
If you see any of these signs, follow the instructions on when to seek emergency care.
How Doctors Diagnose AFI
When you arrive at the clinic or hospital, the doctor will combine history, examination, and rapid tests to narrow down the causes and start treatment fast. A structured approach helps avoid delays that allow complications to develop.
-
Detailed history including travel, insect exposures, recent antibiotic use, and vaccination status.
-
Physical examination focused on the heart, lungs, abdomen, skin, and neurological state.Rapid bedside tests, such as point-of-care blood glucose, urine dipstick, and bedside haemoglobin measurement.
-
Laboratory tests, including complete blood count, basic metabolic panel, and inflammatory markers when indicated.
-
Microbiological tests guided by suspicion, such as blood cultures, urine culture, sputum tests, or targeted rapid tests for dengue, malaria, or influenza.
Combining clinical judgement with rapid diagnostic tests improves the chance of reaching a clear diagnosis quickly.
Early Diagnostic Tests You May Be Offered
Timely testing gives doctors specific answers and reduces unnecessary treatments. The exact tests depend on the likely causes.
-
Blood tests, including full blood count and markers such as C-reactive protein.
-
Blood cultures are obtained when a bacterial bloodstream infection is suspected.
-
Rapid antigen or molecular tests for respiratory viruses and for dengue or malaria in appropriate settings.
-
Urine tests and cultures for suspected urinary infections.
-
Chest X-ray when cough or breathing problems are present.
-
Stool tests for gastrointestinal causes if diarrhoea is a major symptom.
Your clinician will explain the rationale for the chosen tests and how quickly to expect results.
Immediate Management and Treatment
Initial management aims to stabilise you and begin effective therapy while diagnostic tests are underway. Early targeted treatment is often life-saving.
-
Supportive care with fluids and fever control to prevent dehydration and organ stress.
-
Empirical antimicrobial therapy, when bacterial infection or sepsis is suspected, is started promptly after blood cultures, where possible.
-
Specific antiviral or antimalarial therapy when indicated by testing or clinical suspicion.
-
Oxygen therapy or hospital-level monitoring if breathing or oxygenation is compromised.
-
Close observation and repeat reassessment to modify treatment as test results arrive.
Starting the right treatment early reduces complications and shortens recovery.
When to Seek Emergency Care
Some signs require urgent assessment and immediate treatment. Do not wait if these occur.
-
Severe breathlessness or inability to breathe normally.
-
Confusion, reduced responsiveness, or sudden changes in alertness.
-
Very low blood pressure, fainting, or collapse.
-
Signs of poor perfusion, such as cool, clammy skin or a very rapid heart rate.
-
Severe and persistent vomiting or inability to drink fluids.
-
New severe bleeding or rapidly spreading skin redness or bruising.
If any of these appear, go to the nearest emergency department or call emergency services.
Hospital Admission Criteria
Not all cases of AFI require admission, but some clearly do. Admission allows close monitoring, intravenous medicines, and rapid escalation of care.
-
Evidence of sepsis or organ dysfunction.
-
Inability to maintain oral fluids or severe dehydration.
-
Severe respiratory compromise requiring oxygen.
-
High-risk patients such as the elderly, young children, pregnant women, or those with serious chronic diseases.
-
Failure to respond to initial outpatient therapy or when close observation is necessary.
Your clinician will discuss the reasons for admission and what to expect during the hospital stay.
Prevention and Public Health Measures
Preventing AFI means reducing exposure, using vaccines, and acting promptly when symptoms begin. Community measures also lower the risk for others.
-
Vaccination where available, including influenza and pneumococcal vaccines for at-risk groups.
-
Mosquito control and using repellents in areas with vector-borne diseases.
-
Safe food and water practices to prevent gastroenteritis.
-
Early medical review for high-risk exposures and when fever persists beyond a few days.
-
Hygiene measures, including hand washing, are used to reduce the spread of respiratory or enteric infections.
Prevention reduces illness for you and for the community.
Practical tips for caregivers
When you care for someone with an acute fever, practical steps help comfort and minimise complications.
-
Keep fluids available and encourage regular small sips.
-
Use paracetamol for fever and discomfort following dosing advice; avoid combining multiple medicines without advice.
-
Note the pattern of fever and associated symptoms to inform the doctor.
-
Keep the environment ventilated and avoid crowding the patient with visitors if an infectious cause is likely.
-
Follow instructions about when to return for review or go to emergency care.
Clear, calm care often makes a big difference while tests are arranged.
Conclusion
Acute febrile illness can be harmless or life-threatening depending on the cause and how quickly it is recognised. Early diagnosis and timely treatment improve outcomes and prevent progression to sepsis or organ failure. If you or someone you care for develops a high or persistent fever, especially with warning signs listed above, seek medical attention promptly. Working with a physician such as Dr. Basavaraj Kuntoji will help ensure the right tests are done and the appropriate treatment started without delay.
FAQ's
A sustained temperature above 39 degrees Celsius or a fever accompanied by severe symptoms such as breathlessness, confusion, or fainting should prompt urgent review.
Progression varies by cause and individual health. In some cases, deterioration can occur within hours. Early assessment and treatment reduce this risk.
No. Many AFI cases are viral and do not need antibiotics. Doctors start antimicrobial therapy when bacterial infection is likely or when sepsis cannot be excluded.
Rapid diagnostic tests for malaria, dengue, and some respiratory viruses can give quick results and guide immediate treatment decisions.
If the fever lasts more than 48 to 72 hours, or if you have any worrying symptoms listed earlier, consult a clinician promptly rather than waiting.





















 8 Min Read
8 Min Read





.png)











