Have you ever felt so short of breath that even sitting still feels like hard work?
Respiratory failure is that frightening point when the lungs can no longer keep oxygen up or carbon dioxide down, which doctors call hypoxemic respiratory failure or hypercapnic respiratory failure. It can come on suddenly from pneumonia, a pulmonary embolism, severe asthma, or overdose, or develop slowly in conditions like COPD or neuromuscular disease. This blog will help you identify early signs that matter because timely treatment with oxygen therapy, noninvasive ventilation, or mechanical ventilation and specialist care can be lifesaving and greatly improve recovery.
Synopsis
What is Respiratory Failure?
Have you ever felt suddenly unable to get enough air, no matter how hard you breathe? That frightening sensation is what puts respiratory failure on the emergency map. In simple terms, respiratory failure happens when the lungs cannot do their primary job: move oxygen into the blood and remove carbon dioxide from it. When this balance fails, either oxygen falls too low (hypoxemic respiratory failure), carbon dioxide rises too high (hypercapnic respiratory failure), or both problems happen together.
Respiratory Failure Patterns
There are two broad patterns to know:
-
Acute respiratory failure: Comes on quickly and can be life-threatening; it needs urgent hospital care.
-
Chronic respiratory failure: Develops slowly over weeks to months and may be managed with long-term supports such as home oxygen or ventilatory assistance.
Anyone can develop respiratory failure, but it is more likely in people with chronic lung disease, weakened immunity, or conditions that weaken the breathing muscles.
Respiratory Failure Causes
Several illnesses and exposures can tip the lungs into failure. Below are the common causes, explained in a clear, practical way.
Pneumonia
Pneumonia inflames and fills the air sacs with fluid or pus, blocking oxygen transfer into the blood. In older adults or people with weak immunity, pneumonia can rapidly cause hypoxemic respiratory failure if not treated promptly.
Chronic Obstructive Pulmonary Disease (COPD)
Long-standing airflow blockage from COPD (emphysema, chronic bronchitis) progressively reduces the lung’s ability to move air. Exacerbations or infections can push someone with COPD into chronic or acute on chronic respiratory failure.
Asthma
Severe asthma attacks cause intense narrowing of airways. Without quick treatment, airflow drops dramatically, and oxygen levels fall; that’s one route to acute respiratory failure.
Respiratory Syncytial Virus (RSV)
RSV is usually mild in adults but can cause severe lower-respiratory infection in infants, older adults, and those with lung disease, sometimes progressing to respiratory failure.
Pulmonary Embolism
A blood clot in the lung suddenly blocks blood flow through part of the lung (a pulmonary embolism). The affected lung cannot exchange gas properly, and the strain on the heart can cause rapid deterioration and respiratory failure.
Drug Overdose or Sedatives
Overdoses of opioids or sedative medicines directly depress the brain’s breathing centre. Breathing slows or stops, carbon dioxide builds up, and hypercapnic respiratory failure may follow unless the overdose is reversed quickly.
Neuromuscular Disorders
Diseases such as ALS, muscular dystrophy, or high spinal cord injury progressively weaken the muscles that power breathing. Over time, this neuromuscular respiratory failure becomes the limiting factor, with rising carbon dioxide and low oxygen.
There are other causes, such as chest wall deformities, severe trauma, or advanced heart failure, but the items above are the most frequently encountered in clinical practice.
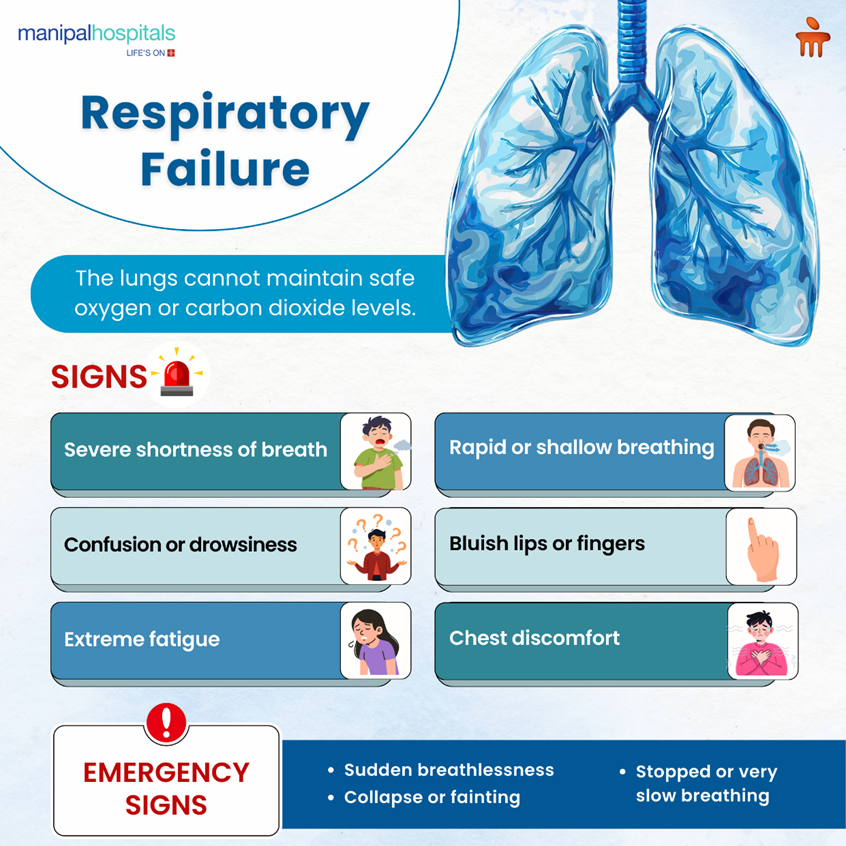
Respiratory Failure Symptoms
Recognising the early signs of respiratory failure can save a life. Look out for:
-
Shortness of breath, at rest or with minimal activity, worse than usual
-
Rapid, shallow, or irregular breathing
-
Confusion, drowsiness, or reduced alertness (a sign of low oxygen or high carbon dioxide)
-
Bluish discolouration of the lips, face, or fingernails (cyanosis)
-
Rapid heart rate, sweating, or chest discomfort
-
Severe fatigue or weakness that makes breathing inefficient
In severe cases, the person may stop breathing (respiratory arrest). If any of these symptoms appear suddenly or progress quickly, seek emergency medical help immediately.
Respiratory Failure Treatment
Treatment depends on what caused the failure and whether it is acute or chronic. The goals are to restore safe oxygen and carbon dioxide levels, treat the underlying illness, and support breathing until the lungs recover.
1. Oxygen Therapy
If oxygen is low, supplemental oxygen therapy is the first step. In hypoxemic conditions, carefully titrated oxygen restores blood oxygen and eases organ stress.
2. Ventilatory Support
If oxygen alone is insufficient or the patient cannot breathe effectively, ventilatory support is needed:
-
Noninvasive ventilation (NIV): Devices such as CPAP or BiPAP deliver positive pressure through a mask. NIV is often used for COPD exacerbations, cardiogenic pulmonary oedema, or early hypercapnic failure.
-
Mechanical ventilation: Invasive support via an endotracheal tube in the ICU when NIV fails or is inappropriate. Mechanical ventilation takes over breathing and buys time for treatments to work.
3. Medications
Treatment is tailored to the cause:
-
Antibiotics for bacterial pneumonia
-
Bronchodilators and steroids for asthma or COPD exacerbations
-
Antivirals for specific viral infections when indicated
-
Thrombolysis or anticoagulation for pulmonary embolism in select cases
-
Naloxone for opioid overdose to reverse respiratory depression
4. Treat Underlying Conditions
Long-term management of COPD, heart failure, or neuromuscular disease reduces future risk. For neuromuscular causes, options include noninvasive ventilation at night and assisted cough techniques.
5. Pulmonary Rehabilitation and Lifestyle Changes
After the acute phase, many patients benefit from pulmonary rehab, supervised exercise, breathing retraining, and education. Quitting smoking, vaccination, nutrition, and exercise support recovery and reduce recurrence.
When to See A Pulmonologist?
You should consult a specialist if you experience:
-
Recurrent or worsening shortness of breath despite basic treatment.
-
Need for oxygen at home or repeated hospital admissions for breathing problems.
-
Complex conditions such as advanced COPD, respiratory muscle weakness, or unclear causes of hypoxemia.
Early specialist involvement often means better long-term breathing and fewer emergencies. At Manipal Hospitals, our best pulmonologists in Kanakapura Road, Bangalore can provide diagnostic testing (ABG, sleep studies, advanced imaging), long-term ventilation plans, and coordinated pulmonary rehabilitation.
Conclusion
Respiratory failure is a serious condition that ranges from a sudden emergency to a slowly progressive limitation. The key points to remember are: recognise worsening shortness of breath early, treat the underlying cause (pneumonia, COPD, pulmonary embolism, overdose, or neuromuscular disease), and use appropriate supports such as oxygen therapy, noninvasive ventilation, or mechanical ventilation when required. For long-term management, pulmonary rehab and specialist care make a real difference.
If you or someone you care for has worrying breathing symptoms, don’t delay, seek urgent assessment at Manipal Hospital Kanakapura Road and, where needed, specialist pulmonology care for a clear treatment pathway and ongoing support.
FAQ's
Hypoxemic respiratory failure means low oxygen in the blood; hypercapnic respiratory failure means high carbon dioxide. Many patients have features of both; treatment is tailored to which problem predominates.
Often yes, when it’s caused by treatable problems like pneumonia, asthma attacks, or opioid overdose, timely treatment and ventilatory support can lead to full recovery. Chronic causes may need long-term support but can be managed to improve quality of life.
The process is done under sedation and analgesia in the ICU, so the patient is comfortable. The aim is to support breathing safely while the underlying illness is treated.
Many can, with the right supports: nocturnal noninvasive ventilation, cough assist devices, home oxygen (if needed), and regular specialist follow-up. A pulmonologist coordinates these services.
Key steps: stop smoking, stay up to date with vaccinations (flu, pneumococcal, COVID-19), manage chronic lung and heart conditions, avoid opioid misuse, and seek early care for infections.





















 8 Min Read
8 Min Read