.png)
Do you know what immediate steps make the biggest difference in the survival and long-term health of a baby born early? In India, preterm births account for about 13.6% of all deliveries, with over 3.5 million preterm neonates annually facing high risks of hypothermia and mortality without prompt intervention. The first 60 minutes after birth are critical for preterm neonates.
Effective golden hour care reduces complications like hypothermia, hypoglycaemia, infection, and respiratory failure. Clear protocols for neonatal resuscitation and processes for the early stabilization of preterm infants are the backbone of better outcomes. This blog explains practical steps, tests, and priorities that neonatal teams use during the golden hour to stabilise preterm neonates safely.
Synopsis
- Golden Hour Care for Preterm Babies
- Core Components of Golden Hour Care
- Essential Steps in Golden Hour Care
- Thermoregulation: A Priority
- Airway and Respiratory Support
- Circulation, Vascular Access, and Fluids
- Metabolic Management
- Infection Prevention and Antibiotics
- Monitoring, Documentation, and Communication
- Family Involvement and Kangaroo Care
- Transport and Transfer Considerations
- Training, Checklists, and Quality Improvement
- When to Escalate Care?
- Conclusion
Golden Hour Care for Preterm Babies
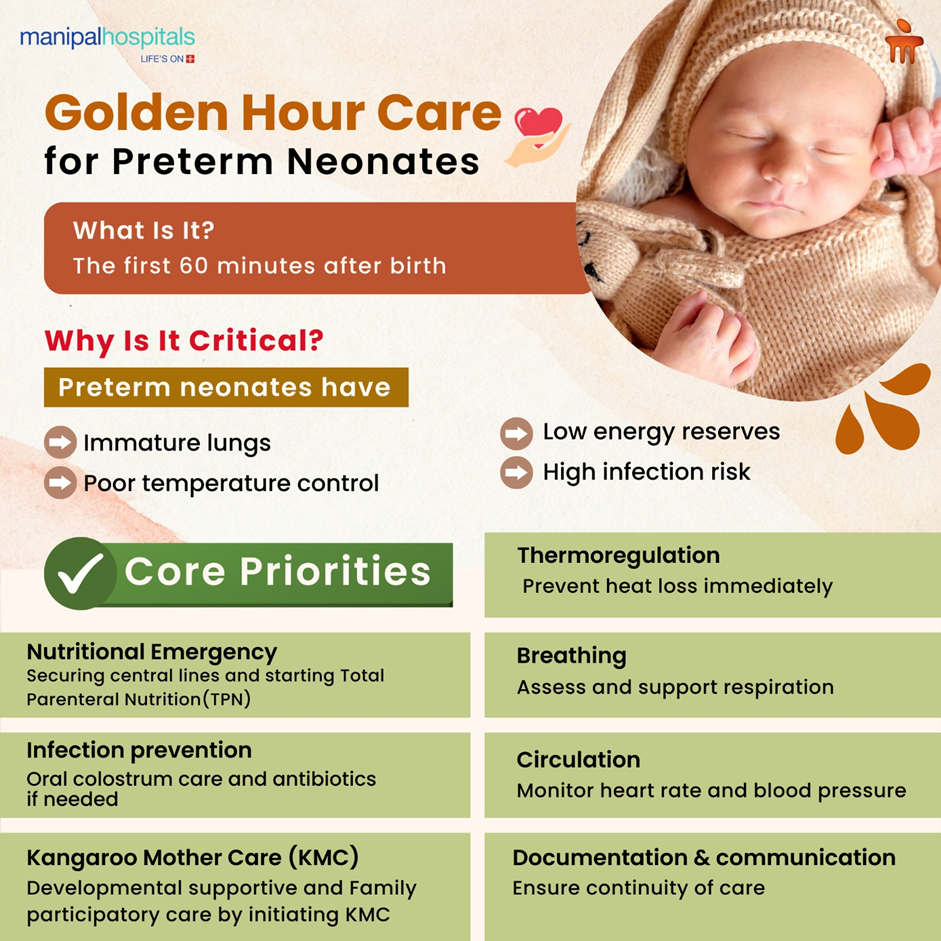
For preterm neonates, organs are immature. Lungs may lack surfactant, skin is thin, and metabolic reserves are low. A sudden cut in nutrition from the mother makes it a nutritional emergency, too. Each minute of delay in stabilisation increases the risk of brain injury, sepsis, and oxygen-related problems. That is why structured golden hour care and rapid neonatal resuscitation when needed are standard practice in modern neonatal units.
Timely interventions during this window set the stage for survival and reduce the need for prolonged intensive care.
Core Components of Golden Hour Care
Successful golden hour care rests on several tightly linked tasks. For preterm neonates, teams prioritise warmth, breathing, circulation, maintaining euglycemia, and infection prevention. Training, equipment readiness, and teamwork are non-negotiable.
The key elements are:
-
Immediate thermoregulation to prevent heat loss
-
Airway support and respiratory assessment, including CPAP or intubation if required
-
Rapid vascular access and initiating total parenteral nutrition
-
Maintaining strict asepsis, starting oral colostrum care and antibiotics when needed
-
Family communication and kangaroo care planning at the earliest
Essential Steps in Golden Hour Care
Below is a practical checklist used in many neonatal units. Use it as a reference for what clinicians aim to complete within the first hour.
|
Step |
Timing |
Purpose |
|
Immediate drying and warming under a radiant warmer or in a plastic wrap |
Seconds after birth |
Prevent heat loss and start thermoregulation in preemies |
|
Assess breathing and tone; provide tactile stimulation |
First 30 seconds |
Determine the need for neonatal resuscitation |
|
Provide CPAP if breathing is inadequate; intubate if required |
Within 1–5 minutes if needed |
Support lungs and oxygenation |
|
Place the pulse oximeter and monitor the heart rate |
Within 1–2 minutes |
Guide oxygen delivery and resuscitation steps |
|
Secure vascular access (umbilical or peripheral) |
Within the first 10–20 minutes |
For fluids, glucose, or medications |
|
Check bedside glucose and correct if low |
Within 10 minutes |
Prevent hypoglycaemic injury |
|
Start empiric antibiotics if maternal risk factors or clinical signs |
Within the first 30 minutes |
Reduce the risk of early-onset sepsis |
|
Stabilise temperature using an incubator or skin-to-skin |
Ongoing during golden hour |
Maintain thermoregulation in preemies |
|
Document events, times, and parental communication |
Throughout the first hour |
Ensure continuity of care and audit performance |
Thermoregulation: A Priority
Preventing heat loss is the single most effective early action for preterm neonates. Use plastic wrap or bags for very preterm babies, warmed radiant warmers, preheated transport incubators, and minimal exposure. Thermoregulation in preemies reduces pulmonary stress, conserves energy, and lowers infection risk. Staff must measure axillary or skin temperature promptly and adjust warming devices to keep core temperature in the target range.
Airway and Respiratory Support
Most preterm neonates benefit from noninvasive respiratory support as a first approach when breathing is inadequate. Early use of continuous positive airway pressure reduces the need for mechanical ventilation.
Teams should be ready for neonatal resuscitation algorithms:
-
clearing the airway
-
positive pressure ventilation
-
and intubation if there is a poor response
-
Use pre-oxygenation carefully and titrate oxygen using pulse oximetry targets specific for minutes after birth
Circulation, Vascular Access, and Fluids
A rapid heart rate check guides the need for chest compressions or medications. For settled babies, secure vascular access, commonly an umbilical catheter, is required to allow safe fluid boluses, glucose administration, and drug delivery. Fluid management must balance the risk of underperfusion against fluid overload. Early protocols guide isotonic and glucose boluses when needed as part of the early stabilization of preterm infants.
Metabolic Management
Hypoglycaemia is common and harmful to the brain. Check bedside glucose early, especially if the baby is tiny or growth-restricted or the mother had diabetes. If glucose is low, give an appropriate bolus followed by infusion while monitoring. Electrolytes and calcium should be corrected promptly if abnormal. These actions are key to the early stabilization of preterm infants. Since preterms are in a catabolic state, they immediately start breaking down their protein and fat stores to generate energy, and these components are already less due to prematurity. Hence, starting protein and lipid infusion at the earliest is very crucial.
Infection Prevention and Antibiotics
Maternal chorioamnionitis, prolonged rupture of membranes, or clinical instability in the newborn raises suspicion for sepsis. Early empiric antibiotics are considered while cultures are obtained. Strict hand hygiene, sterile procedures for lines, and minimal handling reduce infection risk. Early antibiotic decisions should be reviewed frequently to stop therapy if infection is not confirmed.
Monitoring, Documentation, and Communication
Continuous monitoring of heart rate, oxygen saturation, and temperature is essential. Document events, times, interventions, and parental updates. Clear handover notes enable a smooth transition to the neonatal intensive care unit. This documentation supports safe golden hour care and helps teams review performance.
Family Involvement and Kangaroo Care
When the infant is stable, early skin-to-skin contact supports thermoregulation, breastfeeding, and bonding. For very unstable or extremely preterm babies, parental presence at the bedside and clear, honest communication are vital. Explain interventions, expected course, and milestones used to assess stability.
Transport and Transfer Considerations
If the birth occurs outside a tertiary centre, initial golden hour care focuses on stabilisation for safe transfer. Use warmed transport incubators, maintain respiratory support, secure lines, and monitor during transfer. Communication with the receiving neonatal team before transport ensures seamless continuation of care.
Training, Checklists, and Quality Improvement
Routine simulation training, checklists, and post-event debriefs improve performance. Units that audit golden hour care measures, such as time to first temperature, time to first glucose, and adherence to resuscitation protocols, show measurable improvements in outcomes for preterm neonates.
When to Escalate Care?
Escalate to higher levels of support if:
-
The baby fails to respond to initial measures
-
Requires increasing respiratory support
-
Has worsening metabolic derangements
Early involvement of neonatology, paediatric cardiology, or surgery may be needed depending on the underlying cause.
Conclusion
Golden hour care for preterm neonates is a defined set of time-critical actions that reduce complications and improve long-term outcomes. Prioritise temperature control, targeted neonatal resuscitation, early glucose and fluid management, infection prevention, and clear team communication. Practised protocols and trained teams make the difference.
For expert golden hour care, advanced monitoring, and prompt neonatal interventions, contact Manipal Hospital Kanakapura Road. Our neonatal specialist provides 24/7 specialised stabilisation, continuous neonatal EEG monitoring where needed, and coordinated transport services.
Book a neonatal stabilisation consult at Manipal Hospital Kanakapura Road to ensure immediate expert care for preterm births.
FAQ's
The golden hour is the first 60 minutes after birth. For preterm neonates, it is the period when team actions like warming, breathing support, glucose checks, and infection screening have the greatest impact.
Yes, when the baby is stable. Skin-to-skin supports thermoregulation in preemies and breastfeeding. If the infant needs respiratory or vascular support, present parental contact as soon as the clinical team clears it.
Glucose should be checked within the first 10 to 30 minutes for at-risk preterm neonates and earlier if there is poor tone or respiratory difficulty. Prompt correction prevents brain injury.
A trained neonatal team led by a neonatologist or trained pediatrician typically manages neonatal resuscitation. Team roles include airway, circulation, medication, and documentation.
Ask about the baby’s temperature, breathing method, plans for monitoring, whether antibiotics or glucose were started, and when you can hold or feed the baby. Clear updates reduce anxiety and help parents participate in care.





















 7 Min Read
7 Min Read