In today’s world, minimally invasive procedures have received much recognition due to their ability to provide solutions for a number of medical illnesses across specialities without opting for traditional surgery. Interventional pulmonology is one such sub-speciality where pulmonologists manage a range of conditions such as lung cancer, severe asthma, emphysema, chronic bronchitis, airway obstructions, and pleural effusions. Most interventional pulmonology procedures are minimally invasive, which ensures patients experience little to no pain during the procedure. Some discomfort may occur afterwards, but it is usually manageable. In this blog, we will delve deeper into the intricacies of interventional pulmonary procedures.
Synopsis
- What Is Interventional Pulmonology?
- Indications for Interventional Pulmonology: When Do You Need?
- Key Diagnostic Procedures in Interventional Pulmonology
- Minimally Invasive Treatments in Interventional Pulmonology
- Managing Serious Lung Conditions
- Benefits of Minimally Invasive Lung Procedures
- Risks and Considerations
- Conclusion
What Is Interventional Pulmonology?
Interventional pulmonology is a specialised field within pulmonary medicine. This industry uses minimally invasive techniques to diagnose and treat various lung and airway disorders. Such alternatives to conventional surgery allow patients to enjoy quicker healing and reduced complications.
Common Conditions Treated with Interventional Pulmonology
Interventional pulmonology procedures can be recommended for diagnosing and treating various conditions. This includes
-
Central Airway Obstruction: Sometimes, the airways can become blocked by the presence of tumour, scar tissue, or other benign growths, affecting breathing.
-
Persistent Pleural Effusions: This is a build-up of fluid in the space around the lungs that can be drained using minimally invasive procedures.
-
Severe Asthma: Severe forms of asthma need interventions where doctors reduce the amount of muscle in the airway walls and make them less reactive to triggers.
-
Lung Cancer: Procedures like bronchoscopy or lung biopsy are used for diagnosing and staging of lung cancer, where tissue samples are taken to determine the extent of the cancer.
-
Recurrent Pneumothorax (collapsed lungs): This occurs when air leaks into the space between the lung and chest wall.
-
Chronic Obstructive Pulmonary Disease (COPD): Emphysema and chronic bronchitis are two common types of COPD, where minimally invasive techniques can be used to treat their symptoms.
-
Haemoptysis: This is the medical term for coughing up blood or blood-stained mucus from the lungs/airways.
Key Diagnostic Procedures in Interventional Pulmonology
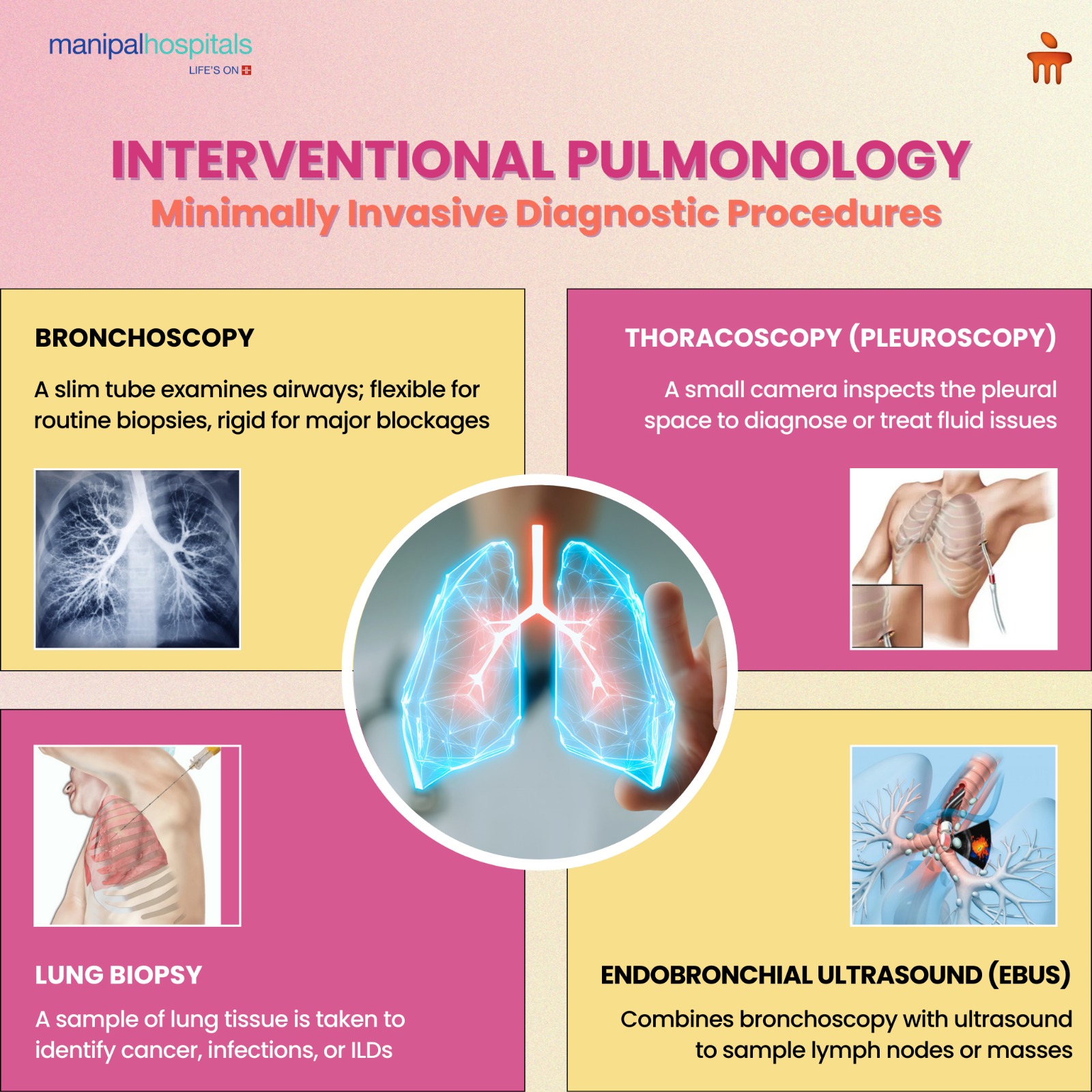
Bronchoscopy uses a bronchoscope. This is a slim tube that inspects the lungs through the airways.
Flexible Bronchoscopy: This is frequently used to diagnose lung illnesses through biopsies, identify infections, or eliminate obstructions. A pliable tube is utilised and typically carried out under local anaesthesia accompanied by sedation.
Rigid Bronchoscopy: It includes an inflexible tube and is utilised in serious situations, like controlling major airway blockages or profuse bleeding. Typically, general anaesthesia is necessary for this procedure.
2. Thoracoscopy (Pleuroscopy)
Thoracoscopy is a procedure where a small camera is used to observe the pleural space between the lungs and chest wall. It aids in identifying issues such as pleural effusions and carrying out treatments like pleurodesis, which manage repetitive fluid accumulation in the pleural cavity.
3. Lung Biopsy
A lung biopsy is a procedure that is used to diagnose conditions such as lung cancer, respiratory infections, and inflammatory lung diseases (ILDs). An affected lung tissue is retrieved for examination to identify the type of cells present, which helps in determining the appropriate treatment plan.
4. Endobronchial Ultrasound (EBUS)
EBUS is a technique that combines bronchoscopy with ultrasound to see structures surrounding the airways. Sampling lymph nodes or masses near the airways is especially valuable for diagnosing and staging lung cancer.
Minimally Invasive Treatments in Interventional Pulmonology
1. Cryotherapy
Cryotherapy employs intense cold to eliminate abnormal tissues. Freezing and removing problematic tissue is a successful method for treating airway tumours, clearing obstructions, or controlling bleeding.
2. Thermal Ablation
Electrocautery, argon plasma coagulation (APC), and laser therapy are popular methods. It can eliminate or decrease airway blockages from tumours or other growths.
3. Navigational Bronchoscopy
This sophisticated method utilises imaging technologies such as CT scans to direct the bronchoscope to hard-to-access parts of the lungs. It is frequently used for the biopsy or treatment of small lung lesions on the outer edges that can't be easily reached with regular bronchoscopy.
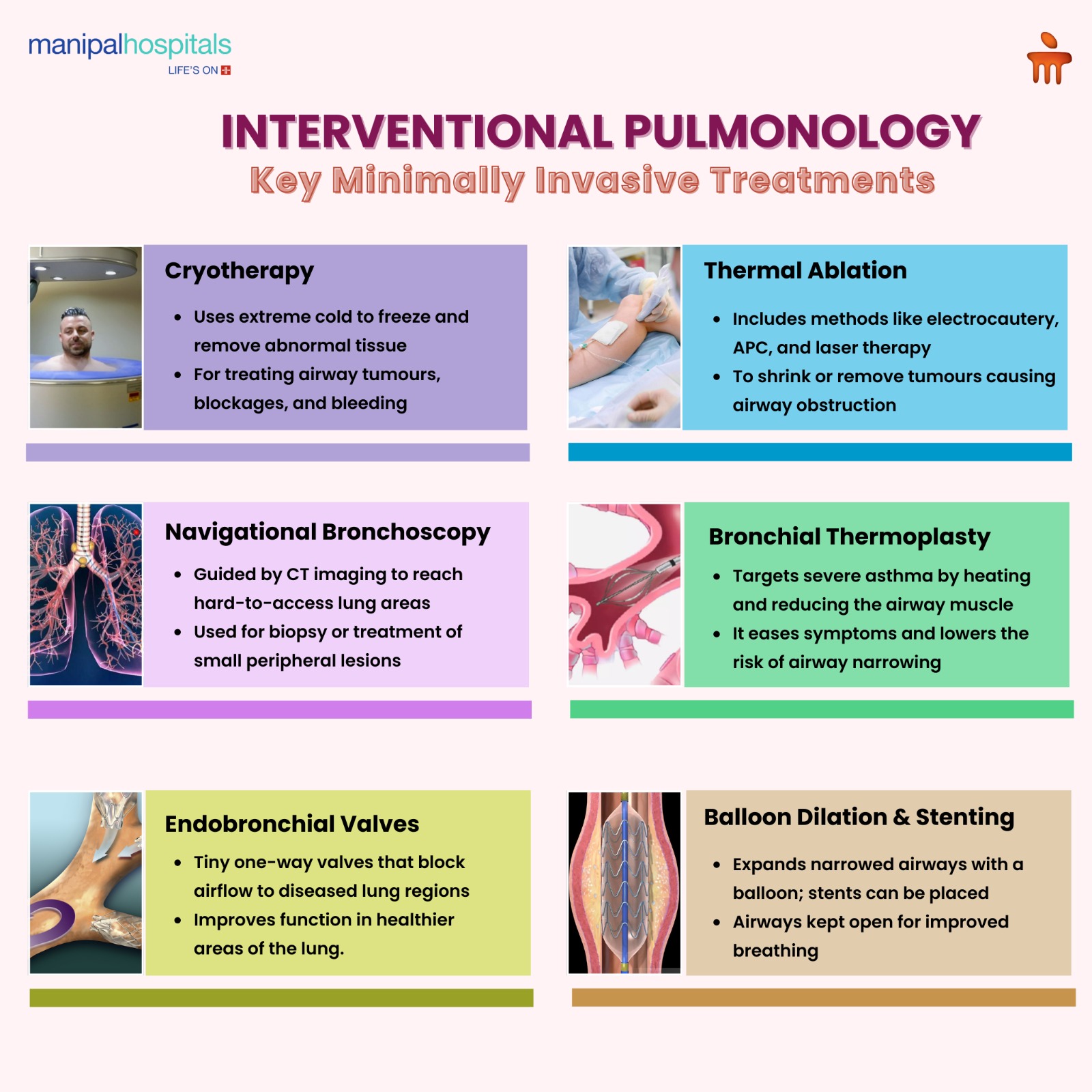
4. Bronchial Thermoplasty
This is a therapy for severe asthma. It heats the muscle bulk in the airways to melt and remove them. The risk of narrowed air passages is also decreased with this process. This, in turn, lessens asthma symptoms.
5. Endobronchial Valves
These are tiny gadgets inserted into the air passages. It stops the air from reaching unhealthy sections of the lung. As a result, the healthier regions can perform more effectively. They are often useful for patients with advanced emphysema to improve lung performance.
6. Balloon Dilation and Stenting
-
Balloon Dilation: This method uses a balloon to expand constricted air passages, facilitating breathing.
-
Airway Stenting: Involves inserting stents to maintain open airways, particularly beneficial for tracheal or bronchial stenosis (narrowing).
Managing Serious Lung Conditions
|
Emphysema Treatment |
Interventional pulmonology provides less invasive options than surgery in cases of severe emphysema treatment. Experts use Bronchoscopic techniques and specialised valves to target the affected areas and improve lung function. For patients who are not candidates for traditional surgery, this method can enhance breathing and quality of life. |
|
Pneumothorax Management |
A pneumothorax, or collapsed lung, can be managed using a chest tube to remove extra air from the pleural space and allow the lung to expand again. Pleurodesis can be further performed to prevent recurrence of the disease. This procedure entails using a substance in the pleural space to form a seal, which causes the 2 layers to stick together and removes any room for air to build up. |
Benefits of Minimally Invasive Lung Procedures
Interventional pulmonology procedures come with several benefits.
-
Minimally Invasive: These procedures are less invasive than conventional operations.
-
Shorter Recovery Times: Patients recover quickly.
-
Reduced Risk of Complications: The risks of complications are much lower than those of invasive procedures.
-
Targeted Treatments: These interventions are directed towards the affected regions only.
-
Outpatient Basis: This process can be performed on an outpatient basis. Patients do not need to stay in the hospital for a prolonged time.
Risks and Considerations
Interventional pulmonology procedures are generally considered safe. However, being a medical procedure, certain risks are involved. For example:
-
Bleeding: Especially during or after biopsies.
-
Infection: Especially at the operation site.
-
Pneumothorax: Risk of lung collapse.
-
Anaesthesia-Related Complications: Possible anaesthetic reactions.
-
Airway Perforation: Airway puncture. However, this is quite rare.
-
Post-Procedural Pain or Discomfort: Some discomfort post-procedure.
Conclusion
Interventional pulmonology is constantly evolving. Innovations like robotic bronchoscopy and cutting-edge imaging techniques are making revolutions in the field. These advancements enhance the accuracy and efficacy of these procedures.
For the best possible treatment option, consult an expert pulmonologist in Jayanagar.
FAQ's
Interventional pulmonology can treat a range of conditions. This includes lung cancer, severe asthma, emphysema, chronic bronchitis, airway obstructions, and pleural effusions.
A bronchoscopy involves inserting a thin, illuminated tube, called a bronchoscope, through the mouth or nose and guiding it into the lungs. This allows our interventional pulmonologist to examine the airways, obtain tissue samples, or carry out medical treatments. Sedatives are usually administered before the procedure to help patients relax. Most patients can return to normal activities within a day or two, especially after a flexible bronchoscopy. If the procedure is extensive, you may need longer to recover.
Most interventional pulmonology procedures are minimally invasive. They are mostly performed under anaesthesia. This ensures patients experience little to no pain during the procedure. Some discomfort may occur afterwards but is usually manageable.
Cryotherapy uses extremely cold temperatures to destroy abnormal tissue in the lungs. It usually doesn't cause any pain and is carried out under sedation. Painkillers can be used to manage mild discomfort during or after the procedure.
Recovery time varies depending on the procedure and individual factors. However, most patients can return to normal activities within a day or two. This is especially applicable for a flexible bronchoscopy. If the procedure is extensive, you may need longer to recover.
Interventional pulmonology plays an important role in the diagnosis as well as treatment of lung cancer. Using lung biopsy and bronchoscopy, doctors can diagnose and stage the cancer. Laser therapy, cryotherapy, and stenting can be done further during the same procedure to control associated symptoms and manage the tumour.
Pleurodesis is a long-term remedy which helps to prevent the recurrence of pleural effusions. The procedure removes any potential for fluid or air to accumulate by sealing the gap between the lung and the chest wall. However, in rare scenarios, pleurodesis may not work where traditional methods can be carried out to treat the issue.
Adults (18 years of age and above) who have severe, chronic asthma that is not adequately managed by conventional therapies (like long-acting bronchodilators and inhaled corticosteroids) may consider bronchial thermoplasty. Bronchial thermoplasty can greatly reduce the frequency and intensity of asthma attacks, although it is not a cure.





















 6 Min Read
6 Min Read