Is shoulder stiffness creeping in, making simple movements like lifting your arm or reaching behind your back a challenge?
Frozen shoulder, also called adhesive capsulitis, often starts with mild discomfort and ends with marked stiffness that can make daily tasks difficult. The positive news is that most people recover with a combination of physiotherapy for frozen shoulder, simple self-care, and selective procedures when needed. This blog explains what causes frozen shoulder, how it typically progresses, and the most effective shoulder stiffness treatment options so you know when to try these measures and when to see a specialist.
Synopsis
What is Frozen Shoulder?
Frozen shoulder (adhesive capsulitis) is a condition where the connective tissue (the capsule) that surrounds the shoulder joint becomes thickened, tight, and inflamed. That process reduces the joint’s capacity to move; first, pain limits motion, and then stiffness becomes the dominant problem. Most cases affect one shoulder, although both can be involved in some people. A typical course spans many months, and recovery can be slow but is usually achievable with the right approach.
Who Gets It and Why?
You might expect frozen shoulder only after a major injury, but it often follows relatively minor events or comes on without a clear trigger. Risk is higher if you have:
-
A recent period of shoulder immobility (for example, after surgery or fracture)
-
People with diabetes are at increased risk and often have a more prolonged course
-
Thyroid disease, heart disease, or other systemic conditions
-
Middle age, particularly in people between 40 and 60 years
Although the exact cause is not fully known, a mix of inflammation and resulting capsule scarring leads to the loss of motion. Immobilisation after injury or medical illness is a common contributor because a lack of movement allows the capsule to tighten.

Early Signs of Frozen Shoulder
Early identification helps you act sooner and reduces frustration. Look out for:
-
Gradual onset of aching pain in the shoulder, often worse at night
-
Increasing difficulty reaching overhead, behind the back, or out to the side
-
A sense that the shoulder is ‘tightening’ and daily tasks (dressing, grooming) are getting harder
If you notice these early signs of frozen shoulder, start gentle movement and book a clinical review; early physiotherapy often shortens the painful phase.
The Stages and Typical Timeline
Frozen shoulder usually evolves through phases: a painful “freezing” phase, a stiff “frozen” phase, then gradual improvement in the “thawing” phase. Timelines vary, but a typical pattern looks like this:
|
Stage |
What Happens |
Typical Duration |
|
Freezing |
Increasing pain and gradual loss of motion |
Weeks to 9 months |
|
Frozen |
Pain may lessen; marked stiffness limits activity |
4–12 months |
|
Thawing |
Gradual return of motion and function |
Months to 2 years |
Overall recovery commonly takes from several months up to two years, though many people regain good function with consistent treatment.
How Do Doctors Diagnose It?
Diagnosis is mainly clinical: your doctor examines active and passive shoulder movement (in adhesive capsulitis, both are limited) and asks about onset, pain pattern, and any recent immobilisation. Imaging, such as X-rays, rules out other causes (arthritis or fracture). Ultrasound or MRI may be used occasionally if the diagnosis is unclear or to look for rotator cuff tears or other shoulder problems. Early, accurate diagnosis helps target the right shoulder stiffness treatment and avoid unnecessary tests.
Choose These Frozen Shoulder Treatment Options
Treatment blends pain control, guided stretching, and interventions for those who do not respond to conservative care. The main aims are to reduce pain, preserve or restore range of motion, and help you return to normal activities.
1. Physiotherapy for Frozen Shoulder (First-Line)
A carefully supervised exercise programme is the cornerstone. A physiotherapist will teach the best exercises for frozen shoulder, gentle stretches, range-of-motion work, and strengthening once pain settles. Consistency matters: daily practice of prescribed stretches speeds recovery and avoids long-term restriction. Heat before stretching and ice after can help with comfort.
-
Start with gentle pendulum moves and passive stretching.
-
Progress to active-assisted and active range of motion as pain improves.
-
Commit to short daily sessions rather than occasional intense stretching.
2. Medication and Injections
Painkillers such as paracetamol or NSAIDs reduce inflammation and make exercise easier. Steroid injection for frozen shoulder (intra-articular corticosteroid) often gives fairly rapid pain relief, particularly useful in the painful freezing phase, and can permit more effective physiotherapy. Recent analyses show injections speed early recovery in pain and motion, though long-term differences may be smaller.
3. Hydrodilatation (Distension Arthrography)
Hydrodilatation for frozen shoulder involves injecting fluid into the joint to stretch the tight capsule, usually under imaging guidance. Many clinical services combine this with steroid injection; evidence suggests it helps improve motion and pain for selected patients who struggle with exercise alone.
4. Procedures: Manipulation and Surgery
If conservative measures fail after an adequate trial (often several months), procedures can restore motion more quickly.
-
Manipulation Under Anesthesia (MUA): the shoulder is gently moved while the patient is anaesthetised to break adhesions; it can be effective but requires experienced teams.
-
Arthroscopic Capsular Release: keyhole surgery to cut the tightened capsule and free the joint; often paired with physiotherapy for best results. Both approaches have shown good outcomes in patients with refractory stiffness.
5. Combined Approach
Teams commonly use a combined strategy: local steroid injection to reduce pain, immediate physiotherapy to stretch, and escalation to hydrodilatation or MUA/arthroscopy if improvement stalls. Recent reviews and surgeon consensus reflect this multimodal practice.
Frozen shoulder does not have a one-size-fits-all solution. Treatment is usually planned based on the stage of stiffness, the level of pain, and how much the condition is affecting daily life. The following outlines the commonly used treatment approaches for frozen shoulder:
|
Treatment |
When It’s Used |
What It Does / Notes |
|
Physiotherapy for frozen shoulder |
First-line for most stages |
Improves ROM and function; requires daily work |
|
Steroid injection for frozen shoulder |
Painful early phase |
Rapid pain relief; helps therapy |
|
Hydrodilatation for frozen shoulder |
When exercise plus injection is insufficient |
Stretches the capsule under imaging |
|
Manipulation under anaesthesia |
Refractory cases |
Breaks adhesions quickly; needs anaesthesia |
|
Arthroscopic capsular release |
Persistent, severe stiffness |
Directly releases capsule; surgical recovery required |
Home Care: What You Can Do Today
Simple measures reduce pain and keep progress steady while you work with a therapist:
-
Use heat for 10–15 minutes before stretching to loosen tissues.
-
Use ice after sessions if pain flares.
-
Maintain good posture and avoid slouching.
-
Keep using the arm for light daily activities; too much rest worsens stiffness.
-
Follow the best exercises for frozen shoulder your therapist gives you, even when progress feels slow.
Small, regular actions matter more than occasional forceful stretching.
When to see a Specialist
See a shoulder specialist if you have:
-
Progressive loss of movement despite several weeks of guided physiotherapy.
-
Severe pain that stops you from participating in rehab.
-
A history of other shoulder problems (rotator cuff tear) or a systemic condition like diabetes that complicates recovery.
-
A need for quicker restoration of function (for work or daily tasks), procedures can shorten the timeline.
Specialist teams will tailor a stepwise plan and discuss the risks and benefits of injections or procedures.
Recovery and Outlook
Recovery can be frustratingly slow, but most people regain useful shoulder movement and pain control. Early physiotherapy and occasional use of injections improve early outcomes. People with diabetes or those with long periods of immobilisation may need longer to recover and should expect a more gradual programme. With consistent rehabilitation and appropriate escalation when needed, many people return to normal activities within months to a couple of years.
Conclusion
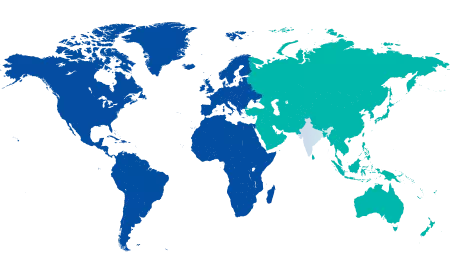
If a frozen shoulder is starting to interfere with everyday life, getting the right help early can change how smoothly recovery goes. At Manipal Hospitals Jayanagar, you are guided by the best orthopaedic specialists in Jayanagar and physiotherapists who take the time to understand your pain, stiffness, and daily routine before planning treatment. From supervised exercises and targeted pain relief to more advanced options when needed, care is paced carefully and explained clearly.
Book a consultation with our Sports Medicine Experts at Manipal Hospitals Jayanagar to receive a practical plan that fits your life. Working closely with orthopaedic and rehabilitation teams, they support safe recovery, restore mobility, and help you return to daily activities or sports with confidence without unnecessary delays or guesswork.
FAQ's
Typical duration spans months to two years, including freezing, frozen, and thawing phases. Some people improve faster with active physiotherapy and appropriate interventions.
Gentle, guided stretching is important. Forceful, aggressive stretching can aggravate pain; follow a physiotherapist’s plan and increase range gradually.
Steroid injections reduce pain and often speed early recovery, but they are usually part of a broader plan (exercise, possibly hydrodilatation, or surgery) rather than a cure on their own.
Surgery (arthroscopic capsular release) or manipulation under anaesthesia is considered when months of guided physiotherapy and injections fail to restore adequate motion and function. These options generally have favourable outcomes when performed by experienced teams.
Recurrence is uncommon, though some people may notice lingering stiffness. Continued home exercises and attention to shoulder use reduce the chance of future problems.





















 8 Min Read
8 Min Read