A short, clear message: screening saves lives. When found early, breast cancer is far more treatable and often curable. A simple, routine check can catch changes long before symptoms appear more prominently. If you are over 40 or have a family history, it’s wise to opt for regular breast cancer screening. Timely clinical evaluation of the breast with a mammogram test can help with early detection and offer you the best chance at treatment and a recovery journey.
Synopsis
- Breast Cancer Screening: How Important Is It?
- Who Should Get Screened for Breast Cancer?
- What Does a Breast Cancer Screening Include?
- How is Breast Cancer Treated When Detected Early?
- The Mammogram Test: How to Prepare And What to Expect?
- What Happens if Your Screen is Abnormal?
- Screening for High-Risk Individuals
- Life After Screening, Prevention, and Healthy Habits
- When to See a Doctor Urgently?
- Conclusion
Breast Cancer Screening: How Important Is It?
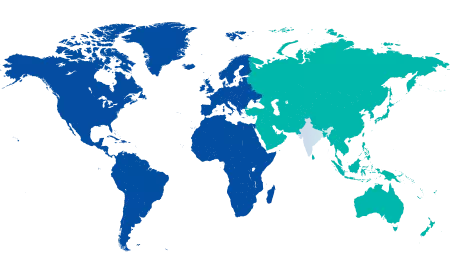
Most people think breast cancer always presents with a lump you can feel. That’s not true. Many early cancers are too small to notice. Modern screening detects tiny changes in tissue architecture, sometimes years before a lump forms. That’s why early detection of breast cancer matters – it increases your treatment options, reduces the need for aggressive therapy, and greatly improves survival and quality of life. In India, awareness and access to care are improving, but late diagnosis is still a concern, especially for people residing semi-urban and remote areas. A screening programme is easy, quick, and designed to find trouble early, before it becomes a crisis. Self-breast examination (SBE) is also equally important for women to notice any changes that may occur to their breasts.
Who Should Get Screened for Breast Cancer?
Screening recommendations vary with age, risk, and guidelines, but here are practical, commonly used suggestions you can follow:
-
If you are between 40 and 49, discuss screening with your doctor and consider an annual or biennial mammogram test based on your risk profile.
-
If you are 50 to 69, routine mammography every one to two years is widely recommended.
-
If you have a strong family history of breast or ovarian cancer, or a known genetic risk (BRCA1/2), talk to a cancer specialist about earlier or more frequent screening, and possibly an MRI in addition to mammography.
-
If you are younger and notice any breast changes, lumps, persistent pain, nipple discharge, or skin changes, don’t wait for a scheduled screen. Get checked immediately.
Screening is not only for older women. If you have risk factors, you and your doctor may agree on a personalised schedule for screening.

What Does a Breast Cancer Screening Include?
A standard screening visit usually involves a few steps:
-
Clinical breast exam: A trained clinician inspects and palpates the breasts and lymph nodes for any suspicious signs. This takes only a few minutes but is an important part of the check.
-
Mammogram test (mammography): A low-dose X-ray of the breast that detects abnormalities invisible to touch. Modern digital mammography is quick and comfortable; results are read by specialised radiologists. Additional imaging if needed: Ultrasound is used to characterise a finding on mammography, especially useful in younger women with dense breast tissue. MRI may be used for high-risk cases. If an abnormality is found, your doctor will arrange a biopsy to take a small tissue sample and send it for pathology. A biopsy is the only way to confirm cancer.
Each step is designed to be minimally invasive, rapid, and accurate. The goal is clear: find problems early and treat them effectively.
How is Breast Cancer Treated When Detected Early?
Catching carcinoma of the breast early changes everything. Small tumours often require less extensive surgery, and lymph nodes may be spared. Some early cancers are treatable with lumpectomy and targeted radiation rather than a full mastectomy. Systemic therapies (chemotherapy, hormonal therapy, targeted drugs) are more effective when the tumour burden is low. Survival rates improve dramatically with early-stage diagnosis.
Beyond survival, early detection often preserves breast appearance, shortens recovery, and reduces long-term side effects. In short, screening gives you choices, and choices matter.
The Mammogram Test: How to Prepare And What to Expect?
Preparing for a mammogram is simple. On the day:
|
|
|
|
|
After the test, your doctor will interpret the images. If everything is normal, you’ll be told the next screening interval. If something needs clarification, an ultrasound or a short clinical review may be arranged.
What Happens if Your Screen is Abnormal?
An “abnormal” screen does not mean cancer. Many findings are benign. The usual pathway after an abnormal mammogram includes targeted ultrasound and, if needed, a guided biopsy. This process may sound worrying, but it is the responsible way to confirm what the imaging suggests.
Biopsy results give you clarity. If cancer is confirmed, a multidisciplinary team, including surgeons, medical oncologists, radiation oncologists, and pathologists, will create a personalised treatment plan. Early-stage cancers have excellent outcomes with current treatments.
Screening for High-Risk Individuals
If you have a strong family history or known genetic mutations, your screening plan needs to be tailored. Earlier and more sensitive tests, like MRI, may be recommended. Genetic counselling helps clarify risk and options, including preventive strategies for certain high-risk people.
If you’re unsure about your risk, a brief consultation with a surgical oncologist or genetic counsellor at Manipal Hospitals can help determine a plan that fits you.
Life After Screening, Prevention, and Healthy Habits
Screening is one part of a broader approach to reducing risk. Small, sustained lifestyle steps make a difference:
-
Maintain a healthy weight and stay active. Exercise lowers recurrence and overall cancer risk.
-
Limit alcohol intake. Even moderate alcohol increases breast cancer risk.
-
Breastfeeding, if possible, is protective.
-
Follow a balanced diet rich in fruits, vegetables, and whole grains.
-
Discuss hormone replacement therapy with your doctor; long-term use may increase risk and needs careful consideration.
Combine screening with healthy habits, and you give yourself the best chance.
When to See a Doctor Urgently?
Don’t wait for your scheduled screen if you notice any of the following:
-
A new lump or thickening in the breast or underarm.
-
Persistent nipple discharge, especially if bloody.
-
Skin changes, dimpling, ulceration, or redness that doesn’t improve.
-
Sudden retraction of the nipple or changes in breast size or shape.
-
Ongoing pain in one part of the breast that’s new and unexplained.
These signs need prompt clinical evaluation, even if your last screen was normal.
Conclusion
A breast cancer screening visit is short. A routine mammogram test, paired with a clinical exam, gives you early warning; so don’t wait for symptoms to appear. Screening puts time on your side and opens up simpler, less invasive treatment choices.
At Manipal Hospital Jayanagar, we offer expert screening services, modern digital mammography, compassionate clinical exams, and rapid follow-up when needed. If you’re ready to take the step, book a screening with us today!
Take charge of your health with timely screening. Visit Manipal Hospitals for advanced breast cancer detection, expert oncologists, and compassionate care close to home.
FAQ's
For most women aged 50–69, every one to two years is recommended. If you’re 40–49, discuss individual risk and screening intervals with your doctor. High-risk women may need earlier or more frequent tests.
No test is perfect. Mammography detects most cancers but is less sensitive in dense breast tissue. That’s why your clinical exam and, if needed, ultrasound or MRI are important complements.
If you find a lump, don’t wait for routine screening. See a clinician urgently for a diagnostic work-up, which may include mammography, ultrasound, and biopsy if indicated.
Mammography is safe while breastfeeding, but images may be harder to interpret due to milk-filled tissue. Tell the technologist about breastfeeding; ultrasound can also be very useful.
Inform your doctor. You may need earlier screening, genetic counselling, or an MRI in addition to mammography. A personalised plan ensures the best surveillance for your situation.





















 8 Min Read
8 Min Read