If someone around you were bitten by a snake, would you feel confident about what to do next or unsure which advice to trust?
Snake bites require fast, correct action, yet myths about snake bite first aid are widespread and can be dangerous. This blog separates myths from facts, explains typical snakebite symptoms, and outlines evidence-based steps for initial care. You will also learn about the clinical pathways for snakebite treatment and longer-term snakebite management, with a clear note on where to seek specialist care in Bhubaneswar if needed.
Synopsis
Why Snake Bite First Aid Matters?
Incorrect first aid, such as applying tourniquets, cutting the bite site, or attempting to suck out venom, can increase tissue damage, delay definitive care, and complicate later snake bite treatment. So understanding which actions are helpful and which are harmful is critical. Health systems treat snake envenoming as a time-sensitive emergency; prompt transport to a facility with antivenom and supportive care is the cornerstone of effective snake bite management.
Common Snake Bite Symptoms
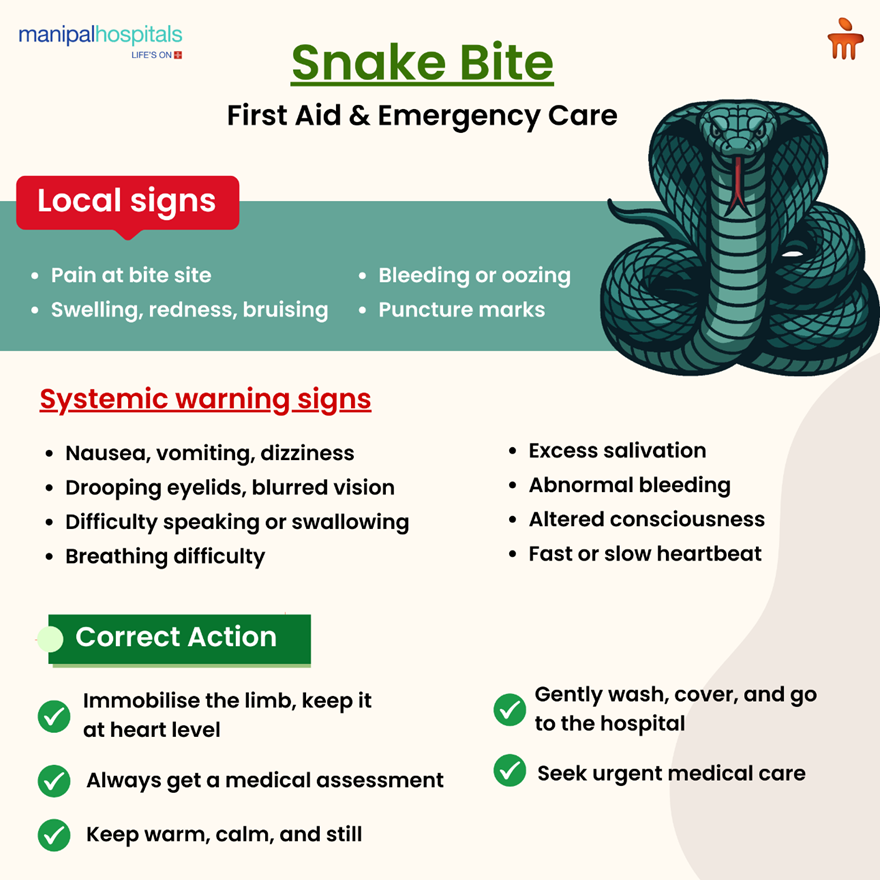
Recognising the range of snake bite symptoms helps determine whether a bite is likely to involve significant envenoming and informs urgency. Early local signs at the bite site may include pain, swelling, redness, bruising, and puncture marks.
Systemic snake bite symptoms that suggest envenoming include
-
Vomiting
-
Dizziness
-
Difficulty speaking or swallowing
-
Drooping eyelids
-
Rapid or slow heartbeat
-
Lightheadedness
-
Excessive salivation
-
Altered consciousness
-
Bleeding from gums or puncture sites
Some venoms produce neurotoxic effects that impair nerve and muscle function, while others cause bleeding and clotting disturbances or direct tissue destruction. A lack of severe systemic symptoms shortly after a bite does not exclude later development, so observation and prompt evaluation are essential.
Myths VS. Facts
There are many traditional first-aid ideas that sound sensible but do real damage. Below is a list of the most common myths so you know what to avoid.
|
Myth |
Fact |
What to do instead |
|
Apply a tourniquet to stop venom spread |
Tourniquets can cause local tissue death, increase compartment pressure, and cause loss of limb if left tight |
Keep the limb immobile and at heart level, remove tight clothing or jewelry, and do not apply a tourniquet |
|
Cut and suck the wound to remove venom |
Cutting increases tissue injury and risk of infection; sucking removes negligible venom and wastes time |
Clean the bite with soap and water, cover with a sterile dressing if available, and seek immediate medical care |
|
Apply ice or cold packs to the bite |
Cold may worsen tissue injury and does not neutralise venom |
Avoid local cooling; keep the patient calm and still, and prioritise rapid transport |
|
Use herbal remedies or alcohol to neutralise venom |
No evidence supports traditional remedies as effective; they can delay proper care |
Do not rely on traditional remedies; proceed to clinical assessment and antivenom when indicated |
|
Observe at home if the snake was nonvenomous |
Some bites appear harmless initially, but develop complications; species identification is often uncertain |
Seek medical assessment; professionals can observe or treat as needed based on clinical criteria |
Immediate Steps for Safe, Evidence-Based Snakebite First Aid
-
Ensure safety first by moving the victim away from the snake and preventing further bites, and if the snake is present, do not attempt to capture or kill it.
-
Please promptly contact emergency medical services or arrange swift transport to the nearest equipped facility.
-
Keep the victim still and calm, because movement increases venom spread through the lymphatic system; immobilise the bitten limb with a splint if possible, and keep it at the level of the heart rather than raised.
-
Remove tight clothing, jewelry, or anything that could constrict the limb as swelling develops.
-
Wash the bite area gently with soap and water if available and cover with a clean dressing; do not cut the wound, suck it, or apply ice.
-
Do not give the victim alcohol, caffeinated beverages, or any medication unless directed by medical personnel; avoid painkillers such as aspirin that may worsen bleeding if venom affects clotting.
-
If the snake is safely visible from a distance, try to memorise its appearance for later identification, but do not attempt capture. Photographs taken at a safe distance may help clinicians identify the species.
-
Monitor breathing, pulse, and level of consciousness, and be ready to perform basic life support if the victim becomes unresponsive.
These steps form the backbone of correct snake bite first aid and set the patient on the fastest path to definitive snakebite treatment.
How Do Emergency Services Assess and Manage Snake Envenoming?
On arrival, clinicians prioritise airway, breathing, and circulation and take a focused history, including time of bite, circumstances, visible snake features, and first aid applied.
Evaluation includes examination of the wound, measurement of limb swelling, documentation of snake bite symptoms, and baseline blood tests such as a full blood count, coagulation profile, renal and liver function tests, and, where available, tests for muscle breakdown (creatine kinase).
Management follows protocols: supportive care for airway or breathing compromise, intravenous access and fluid resuscitation for hemodynamic instability, pain control with appropriate analgesics, tetanus prophylaxis, and targeted use of antivenom when indicated.
-
Antivenom is the specific therapy for venomous bites when systemic or progressive local effects occur. It neutralises circulating venom and reduces morbidity and mortality, but it carries a risk of allergic reactions.
-
Decisions about antivenom depend on the presenting snakebite symptoms, laboratory evidence of envenoming such as coagulopathy, and the clinical course.
-
For neurotoxic envenoming with respiratory compromise, early antivenom and supportive ventilation are lifesaving.
-
For bites causing bleeding or coagulopathy, antivenom, along with blood product support, may be required.
Wound care and, when necessary, surgical consultation for severe local tissue necrosis are parts of snake bite management.
Preventing Bites
Many bites happen during routine activities like farming, walking at night, or reaching into dark places. Reduce risk by:
-
Wearing shoes and long trousers when walking in rural or grassy areas
-
Using a torch at night
-
Avoiding sleeping on bare ground if snakes are common
-
Checking shoes and bedding before use
-
Teaching children to stay away from snakes and to alert adults rather than try to catch them
Community awareness and better access to emergency care are crucial; India’s recent national action plans reinforce prevention, training, and antivenom availability.
Conclusion
Correct snake bite first aid avoids actions that increase harm and focuses on rapid assessment, immobilisation, and prompt transport to a facility capable of delivering antivenom and supportive care. Recognising early snake bite symptoms and seeking care quickly allows clinicians to tailor snakebite treatment appropriately.
Manipal Hospital Bhubaneswar provides emergency antivenom therapy under monitored conditions and access to surgical, renal, and intensive care support required for complex cases. Prompt transfer to an equipped centre reduces complications and improves outcomes, so do not delay in seeking definitive care.
FAQ's
Antivenom is considered when there are progressive local signs such as expanding swelling and severe pain, clear systemic snake bite symptoms such as vomiting, drooping eyelids, breathing difficulty, or altered consciousness, laboratory evidence of coagulopathy or rising muscle enzyme levels; or when the bite is from a species known to cause severe envenoming; clinicians make the decision based on clinical assessment and tests.
Nonvenomous bites can still cause significant local injury and infection, and some species have variable venom potency. Therefore, all bites warrant medical assessment, wound cleaning, and observation rather than being dismissed as harmless.
No, attempting to catch or kill the snake increases the risk of additional bites; if it is safe to do so, take a photograph from a distance to help clinicians with identification, but do not approach the animal.
Observation periods vary by species and clinical findings, but patients are commonly watched for at least 24 hours for delayed systemic effects, and longer if initial tests indicate evolving coagulopathy, renal injury, or neurotoxic signs; clinicians use serial assessments and lab tests to determine safe discharge timing.
No reliable evidence supports traditional remedies for neutralising venom, and some practices, such as incisions, suction, or tight tourniquets, increase harm. The recommended immediate actions are immobilisation, gentle wound cleansing, and urgent transport for professional snakebite treatment.






















 7 Min Read
7 Min Read


















