Do you suffer from planning your day around access to toilets because the urge to urinate can appear suddenly and without warning? That sudden urgency can be a sign of overactive bladder, a common condition that affects people of all ages but becomes more frequent with advancing years. This blog will help you understand the typical overactive bladder symptoms, likely causes, and practical treatment options to help you act early and regain control.
Synopsis
- What is an Overactive Bladder?
- How Does the Bladder Work?
- What Causes an Overactive Bladder?
- Typical overactive bladder symptoms
- How Is Overactive Bladder Diagnosed?
- First-Line Management: Simple Changes That Often Help
- Medications: When Lifestyle Measures Aren’t Enough
- Overactive Bladder Treatment: When You Need More Help
- Practical Tips You Can Start Today
- When Should You See a Specialist?
- Conclusion
What is an Overactive Bladder?
Overactive bladder is a clinical diagnosis defined by a pattern of urinary urgency with or without urinary frequency and nocturia, with or without urge incontinence, in the absence of an infection or other obvious pathology. The condition reflects inappropriate bladder muscle activity or an altered sensory threshold so that the bladder signals urgency before it is fully or comfortably filled. The key clinical elements to recognise are sudden urgency and, in some people, accidental leakage associated with that urgency.
How Does the Bladder Work?
Your bladder stores urine until you decide to pass it. Signals travel between the bladder and your brain to tell you when it’s time. In an overactive bladder, the bladder muscle (detrusor) is overly sensitive or contracts unexpectedly. That gives you a sudden, often urgent need to pass urine, even when the bladder is not full. This mismatch of signals is why urgency feels so out of your control.
What Causes an Overactive Bladder?
There isn’t always a single clear cause. Some common overactive bladder causes include:
-
Idiopathic causes: Many cases have no identifiable cause but relate to increased bladder sensitivity or involuntary bladder muscle contractions.
-
Bladder irritation: Infections, bladder stones, or tumours can trigger urgency.
-
Neurological conditions: Parkinson’s, stroke, multiple sclerosis, and spinal injuries may alter bladder control.
-
Lifestyle and medical factors: High caffeine or alcohol intake, some medications, constipation, and obesity can make symptoms worse.
-
Post-menopausal changes or pelvic organ prolapse in women can also contribute to symptoms.
Your doctor will check for reversible causes first because treating the underlying issue often improves symptoms.
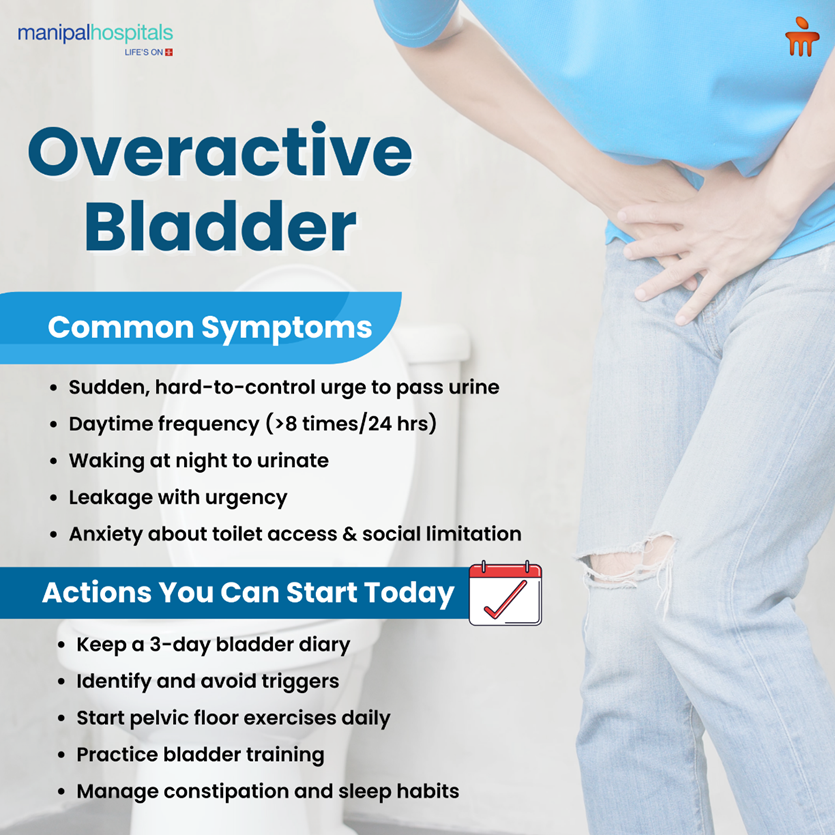
Typical overactive bladder symptoms
Recognising the common signs helps you and your clinician move quickly from uncertainty to a diagnostic plan. The most frequent overactive bladder symptoms include
-
A sudden need to pass urine that is difficult to defer, described clinically as urgency
-
Increased daytime urinary frequency, often defined as more than eight voids in 24 hours
-
Nocturia, the need to wake at night to pass urine one or more times
-
Urge urinary incontinence, where leakage accompanies or follows urgency
-
Associated anxiety about leaving home or being far from a toilet, which can affect quality of life
These symptoms vary in severity and pattern. Some people report only urgency and frequency without leakage, and others experience frequent small-volume voids that disrupt sleep and daily activities. Below summarises symptoms, likely clinical significance, and the initial action clinicians typically take.
|
Symptom |
Clinical significance |
Initial clinical action |
|
Sudden urgency to urinate |
Core feature of overactive bladder |
Review history, bladder diary, and urine test |
|
Daytime frequency (>8 voids/24h) |
May indicate reduced bladder capacity or high intake |
Measure fluid intake, keep a bladder diary, consider frequency-volume chart |
|
Nocturia (waking at night) |
Affects sleep; may reflect urine production or bladder storage |
Check for sleep apnoea, diabetes, and nocturnal polyuria; measure nocturnal urine volume |
|
Urge incontinence |
Urinary leakage with urgency |
Assess severity, perform a pelvic exam, postvoid residual, consider urodynamics if needed |
|
Painful urination or blood in urine |
Suggests infection, stones, or other pathology |
Urine microscopy/culture, ultrasound, or cystoscopy as indicated |
How Is Overactive Bladder Diagnosed?
Diagnosis starts with a careful history and simple tests. Expect:
-
A focused medical history and a symptom discussion.
-
A bladder diary (frequency/volume chart) to record how often you go, volumes, and any leakage.
-
Urine testing to rule out infection or blood.
-
Measurement of post-void residual urine in some cases.
-
Further tests (urodynamics, ultrasound, cystoscopy) only if initial measures are inconclusive or symptoms are severe.
These steps make sure treatment targets the right problem rather than guessing.
First-Line Management: Simple Changes That Often Help
Start with low-risk measures that are often very effective. You’ll usually be encouraged to try these for at least 6–12 weeks before moving to medication.
Bladder training and behaviour changes
Bladder training teaches your bladder to hold urine for longer and reduces the number of trips to the loo. It usually begins with a bladder diary and a plan to slowly increase the interval between voids. Evidence shows bladder training can reduce urgency and leakage for many people.
Pelvic floor muscle training (PFMT)
Strengthening your pelvic floor muscles helps control urgency and can reduce episodes of leakage. Work with a trained physiotherapist or continence advisor for the best results. Clinical studies show PFMT offers measurable benefit for many people with OAB symptoms.
Lifestyle measures to try now
-
Cut back on caffeine, alcohol, and fizzy drinks if they trigger urgency.
-
Spread your fluid intake throughout the day, and avoid drinking a lot before bedtime.
-
Treat constipation promptly; hard stools can press on the bladder.
-
Lose weight if you are overweight; even modest weight loss eases pressure on pelvic tissues.
These steps are simple, but they matter. Many people notice improvement without ever needing stronger treatment.
Medications: When Lifestyle Measures Aren’t Enough
If conservative steps don’t give adequate relief, medication is usually the next step. Two main drug classes are commonly used: antimuscarinics and beta-3 agonists. Both aim to reduce involuntary bladder contractions or increase bladder capacity. Your clinician will discuss the benefits and side effects so you can choose what suits you best. The AUA guideline supports offering these medications as a treatment option when needed.
Key points about medication:
-
Antimuscarinics can reduce urgency and leakage but may cause dry mouth, constipation, or blurred vision in some people.
-
Beta-3 agonists are an alternative with a different side-effect profile and may suit people who cannot tolerate antimuscarinics.
-
Your doctor will review other medications you take to avoid interactions.
-
If side effects are unacceptable, switching agents or adjusting the dose is common practice.
Overactive Bladder Treatment: When You Need More Help
If symptoms remain troublesome despite lifestyle changes and medication, several effective options exist. Your specialist will discuss suitability and likely benefits.
-
Botulinum toxin (Botox) into the bladder - A controlled injection into the bladder muscle can reduce involuntary contractions and improve urgency and leakage. Effects are temporary and may require repeat treatment. Some people need to learn intermittent self-catheterisation after treatment if emptying becomes difficult.
-
Sacral nerve modulation (neuromodulation) - This is a small device implanted under the skin that sends electrical pulses to nerves controlling bladder function. A trial phase is done first to see if it helps. For many, it reduces urgency and leakage when other measures fail.
-
Percutaneous tibial nerve stimulation (PTNS) - A less invasive nerve therapy that stimulates a nerve near the ankle to influence bladder control. It may help some people who prefer to avoid surgery.
-
Surgery - Surgery is rarely needed for uncomplicated OAB. It is considered only when other treatments fail and a clear surgical target exists. Your specialist will explain realistic outcomes and risks.
Practical Tips You Can Start Today
Begin with a short plan and build on it:
-
Keep a 3-day bladder diary to share with your clinician.
-
Try to identify triggers (caffeine, citrus, spicy foods) and cut them out for a trial period.
-
Practice pelvic floor exercises daily, and get instruction early so you do them correctly.
-
Try bladder training: if you currently go every hour, add 10 minutes and stick with the new interval for a week before increasing again.
Small, steady steps often give the best, sustainable results.
When Should You See a Specialist?
See your urology specialist if you have:
-
Sudden onset of severe symptoms
-
Blood in the urine, painful urination, or unexplained weight loss
-
Recurrent urinary infections
-
Symptoms that do not respond to first-line measures
Specialist assessment ensures serious causes are ruled out and that you get tailored treatment.
Conclusion
An overactive bladder can feel intrusive, but you don’t have to accept it as inevitable. Start with sensible lifestyle steps, bladder training, and pelvic floor work. If you need more help, safe and effective medical and procedural overactive bladder treatment options are available. The best approach is personalised: work with your clinician, keep a bladder diary, and review treatment choices together. If your symptoms reduce your quality of life, make an appointment; the right plan can bring real improvement. For coordinated urology and pelvic health services, consider a specialist consultation at Manipal Hospital Bhubaneswar.
FAQ's
Start a bladder diary for three days and cut back on likely triggers like caffeine. Try bladder training and pelvic floor exercises. If symptoms persist, see your doctor for tests and further advice.
Yes. When taught and done correctly, pelvic floor muscle training reduces urgency and leakage for many people. A physiotherapist or continence advisor can tailor the exercises to you.
Many people use medications safely for months or years. Your clinician will discuss possible side effects and monitor you. If side effects occur, there are alternative drug classes and non-drug options to try.
Botox often helps, but it can make it harder to empty the bladder for some people. In such cases, intermittent self-catheterisation may be needed. Your specialist will explain the trial period and follow-up.
Absolutely. Reducing bladder irritants, managing fluid timing, treating constipation, and losing excess weight often produce meaningful improvements. These measures are the foundation of management.






















 7 Min Read
7 Min Read



















