Wearable tech like smartwatches, fitness trackers, and even the most talked about prototype worn by a famous CEO are promising to change the way we monitor heart health. This is because watches can do more than just tell time these days. These tools say they can find everything from irregular heartbeats to early signs of cardiovascular risk, which could let users know about problems before they become emergencies. Experts are split, though, because of the hype around things like a prototype that uses Near-Infrared Spectroscopy (NIRS) wearable heart health devicesto measure brain blood flow.
A radiologist from one of Delhi's top medical schools recently called this kind of unproven technology "fancy toys for billionaires" because it doesn't have any scientific proof. So, can these devices really tell you how healthy your heart is? This blog looks at the abilities and limits of arterial screening, as well as what doctors really think about it. This is especially important if you are in Bangalore, where getting screened for cardiac care in Bangalore is much easier in places like Manipal Hospitals Bangalore.
Synopsis
The Promise: How Wearables Monitor and Predict Heart Issues
Wearable devices have evolved from basic step counters to sophisticated health guardians. At their core, they use sensors like photoplethysmography (PPG) for heart rate (HR) tracking, electrocardiogram (ECG) capabilities for rhythm detection, and algorithms to estimate metrics like blood oxygen (SpO2), heart rate variability (HRV), and even pulse wave velocity (PWV), a key indicator of arterial stiffness. For example, devices like the various smartwatches can find atrial fibrillation (AFib), a common irregular heartbeat that raises the risk of stroke. Studies have shown that they can do these tasks with 98–99% accuracy in real life. Pulse wave velocity devices and arterial stiffness measurement devices are especially interesting for figuring out long-term heart disease risk.

PWV tells you how fast blood pressure waves move through arteries. Faster speeds mean stiffer vessels, which are linked to a higher risk of problems from heart disease. Wearable arterial stiffness devices, like the Omron HeartGuide, use PPG or oscillometry to let you monitor your arteries at home. These instruments could help you find problems like high blood pressure or aging blood vessels early. Digital pulse wave velocity devices use AI to make predictions more accurate. In large trials, like one major heart study, some of them got AFib predictions right 84% of the time.
Real-world success stories abound, where one account found out how a wearable's EKG alert detected stable angina, preventing a second heart attack through timely surgery. In the same way, educational materials show that wearables can help find breathing or heart problems early by tracking SpO2 and VO2 max, with AI improving accuracy for issues like kidney injury (up to 90%). On X, users share anecdotes: one neighbor flagged a critically low heart rate, leading to life-saving open-heart surgery. Another post from a neurologist describes an asymptomatic 60-year-old detecting Mobitz type 2 heart block via ECG, prompting immediate pacemaker implantation.
The Reality Check: Accuracy, Reliability, and Doctor Views
While promising, doctors caution that wearables aren't infallible. Pros include continuous monitoring, tracking HR round-the-clock to spot trends invisible in clinic visits, and empowerment for users to manage habits like exercise or sleep. Evidence supports their use in cardiovascular risk assessment, prevention, and management, with devices showing clinical-grade HR accuracy during rehab. A JACC review affirms consumer wearables' role in deriving metrics like HRV, which reflects autonomic function and stress resilience.
But the cons are big. Wrist-based devices can be wrong because of movement, skin tone, or a faulty fit. They often overestimate or underestimate during intense activity. They're not meant to be used for diagnosis; false positives for AFib could lead to tests that aren't needed and raise healthcare costs. For heart patients, chest straps are better than wrist wearables for measuring respiratory rate or heart rate, but they aren't perfect either. Problems like data privacy, a lack of standardization, and relying too much on something without clinical proof still remain as the biggest cons.
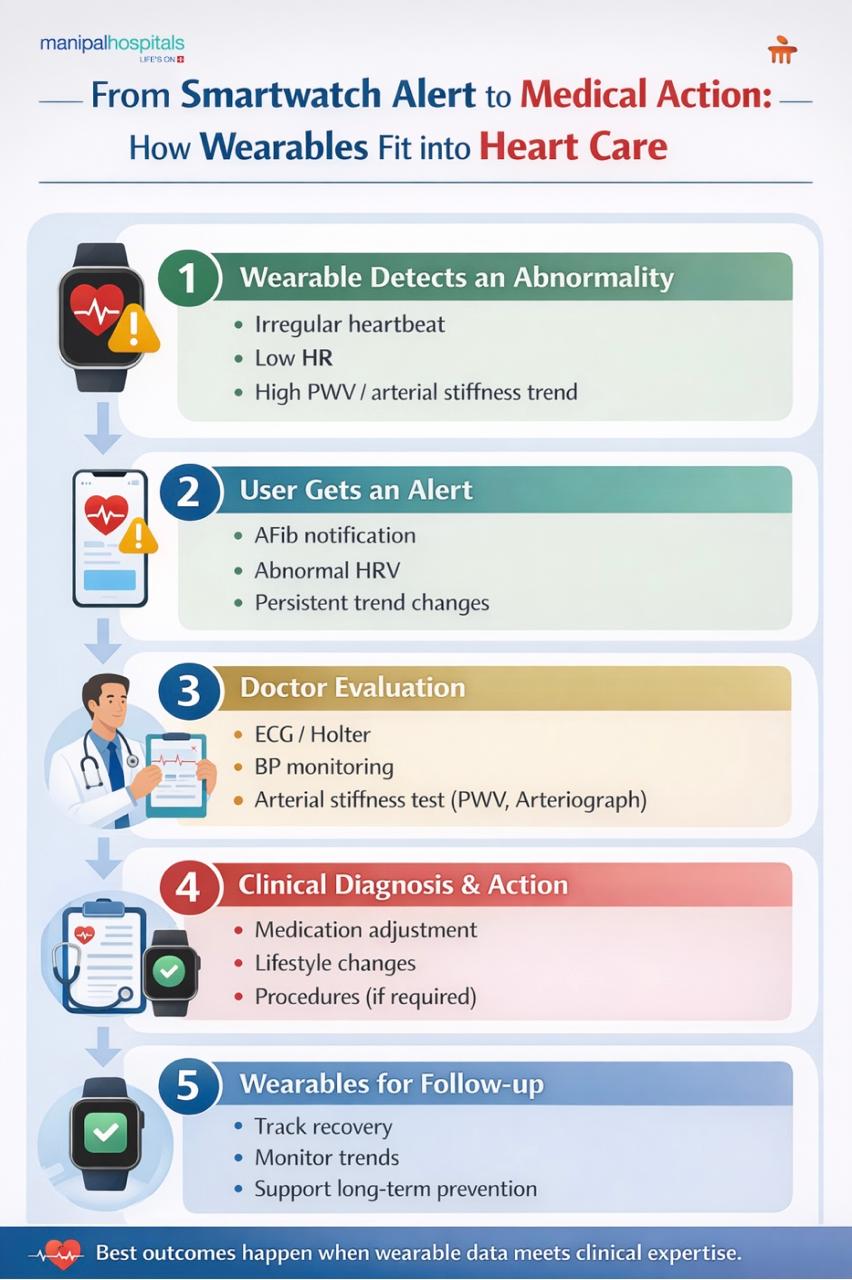
Medical experts emphasize balance. They see wearables improving arrhythmia detection with AI, but they stress they complement, not replace, professional care. A university health doctor notes devices aren't as precise as office equipment, and users may misinterpret data.
But seasoned experts warn of EMF emissions causing anxiety or health risks, based on personal tests, and echo the thought that claiming smartwatches' radar frequencies induce depression and could promote skin cancer. Endeavor Health promotes wearables for AFib alerts; however, they tie it to professional follow-up.
For heart failure management, wearables like smart shirts or vests monitor impedance for fluid buildup, predicting readmissions with 87% sensitivity. Yet, a study on older athletes found arrhythmias often unrelated to exercise volume, linked instead to heart scarring, highlighting wearables' limits in causation.
|
Metric |
Accuracy Pros |
Reliability Cons for Wearables |
|
Heart Rate (HR) |
Clinically acceptable during exercise (correlation ≥0.90) |
Influenced by motion artifact, less accurate in low perfusion |
|
Atrial Fibrillation (AFib) |
98-99% sensitivity in studies |
False positives in general population need ECG confirmation |
|
Pulse Wave Velocity (PWV) / Arterial Stiffness |
Predicts CV risk with AI (up to 90% for related issues) |
Requires calibration, affected by user factors like skin tone |
|
Blood Pressure (BP) |
Estimates within 6-8 mmHg error |
Not cuff-accurate; dynamic states reduce precision |
What Doctors Want You to Know: Practical Advice
Doctors all agree: Don't use wearables as oracles; use them as tools. If you notice something strange, don't try to figure it out yourself; get help from a professional. Devices help people with heart problems keep track of their habits, but they need to be checked against medical-grade tests. In or near cardiac care in Bangalore, you can get arterial stiffness tests done at local hospitals for affordable prices. These tests use devices like the Arteriograph and combine wearables with clinical screening for full care.
Dr. Anand Shenoy, Consultant - Interventional Cardiology at Manipal Hospital, Old Airport Road, commented, “Wearable cardiovascular devices utilize various sensors to monitor heart rate, rhythm, sleep, and activity. Sophisticated algorithms analyze heart rate variability to assess autonomic nervous system function while also flagging potential issues like atrial fibrillation. Factors such as movement and skin tone limit the accuracy of these devices, despite their benefits for longitudinal self-monitoring and lifestyle changes. Calorie expenditure estimates are often inaccurate, particularly during specific activities or in individuals with certain conditions. Consequently, wearable data should be viewed as trend indicators, not definitive medical diagnoses, because clinical tools are still required for thorough evaluations.”
Future trends? Integrating AI could improve predictions, such as using a smartwatch to find Takotsubo cardiomyopathy, but there are still problems with regulations and fairness. If wearables are not available to everyone, they could make health disparities worse. Some experts believe that the future of cardiac care is wearable and data-driven, but it's ultimately based on facts. If you're considering one, start with FDA-cleared options and pair with regular checkups. Your heart, and doctors, will thank you.
FAQ's
Wearable devices can detect early warning signs like irregular heart rhythms, abnormal heart rate trends, or increased arterial stiffness. However, they do not predict heart disease with certainty. Doctors view them as supportive tools that highlight risks, not definitive predictors or diagnostic devices.
Many smartwatches can detect atrial fibrillation with high sensitivity, up to 98–99% in controlled studies. However, false positives are possible, especially in healthy individuals. Any alert should always be confirmed through medical tests such as ECG or Holter monitoring.
No. Wearables cannot replace clinical investigations like ECGs, echocardiograms, or blood pressure monitoring. Doctors emphasize that wearable data should complement medical evaluation, not replace professional diagnosis, especially when symptoms or abnormal alerts are present.
An abnormal reading should prompt attention, not panic. Wearables are early warning tools meant to prompt medical consultation. Doctors advise against self-diagnosis and recommend confirming findings through professional evaluation and medical-grade testing.
Yes, wearables can help patients track heart rate, activity levels, sleep, and recovery trends. For conditions like heart failure or arrhythmias, they support monitoring and follow-up. However, doctors stress they must be used alongside regular medical care.






















 6 Min Read
6 Min Read



.png)