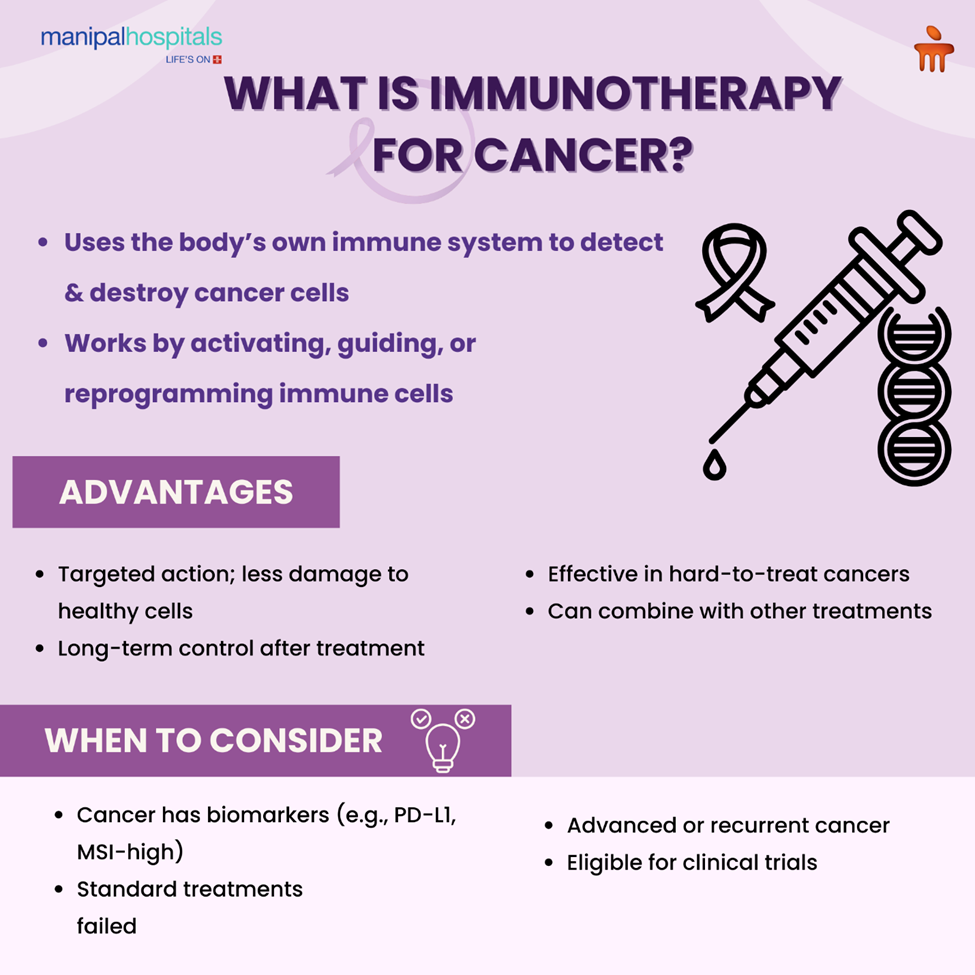
Historically, cancer was treated with surgery, chemotherapy, and radiation. Immunotherapy for cancer has emerged as a novel breakthrough. Rather than killing tumours directly, immunotherapy acts to strengthen or direct the immune system to better identify and destroy cancer cells.
Immunotherapy for cancer includes new therapies ranging from immune checkpoint inhibitors to advanced cell-based treatments. Immunotherapy may provide longer responses and less toxicity in some cases. With this blog, a leading medical oncologist in Vijayawada highlights how immunotherapy is poised to become the mainstream treatment in modern oncology and form the basis of powerful interventions against cancer.
Synopsis
- How Immunotherapy Works in the Body
- Types of Immunotherapy Used in Cancer Treatment
- Advantages of Immunotherapy for Cancer Treatment Over Conventional Treatments
- Cancers That Are Sensitive to Immunotherapy
- When to consider Immunotherapy for Cancer Treatment?
- Possible Risks and Side Effects
- Conclusion
How Immunotherapy Works in the Body
The work of the immune system is to guard the body against invading organisms like viruses, bacteria, and even abnormal cells. Simply put, cancer arises when some of these abnormal cells evade detection and grow uncontrollably. This is because cancer cells have the ability to send out signals that inhibit immune function. Immunotherapy for cancer treatment solves this by making natural defences stronger or reprogramming them to identify and destroy cancer better. The method applied varies with the type of therapy administered. But the aim is to regain the immune system's capacity to attack cancer cells without damaging healthy tissues.
Types of Immunotherapy Used in Cancer Treatment
Immunotherapy is a general class of anticancer treatments that exploit and amplify the body's immune response to recognize and target cancer cells using multiple mechanisms. Each approach involves attacking a distinct component of the immune system, targeting the cells. Blending medical specificity with the body's own defenses, these forms of immunotherapy are offering new hope for cancer therapy when traditional methods have hit a wall.
Immunotherapy for cancer is primarily classified as:
1. Immune Checkpoint Inhibitors
The immune system has "checkpoints" that are proteins on immune cells to prevent attacking healthy cells. The cancer cells can use these checkpoints to evade immune attack. Immune checkpoint inhibitors suppress these proteins so the immune cells can recognize and target cancer cells.
-
Targets often include PD-1, PD-L1, and CTLA-4.
-
Approved for cancers like melanoma, lung cancer, kidney cancer, and bladder cancer.
2. CAR T-Cell Therapy (Chimeric Antigen Receptor T-cell)
It is an extremely personalized immunotherapy cancer treatment. In this, doctors take a patient's T-cells, alter them in the laboratory so that they can carry special receptors that identify cancer cells, and then give them back to the patient. These:
-
Used primarily for some blood cancers, such as acute lymphoblastic leukaemia and some lymphomas.
-
Can cause powerful, long-term remissions but only in specialized centres.
3. Monoclonal Antibodies
These are proteins created in the laboratory to bind to unique targets on cancer cells. When they bind to their targets, they are able to:
-
Tag the cancer cell for killing by immune cells.
-
Switch off signals that allow cancer cells to grow.
-
Release poison directly into the cancer cells, like antibody-drug conjugates.
4. Cytokine Therapy
Cytokines are natural proteins that regulate cell growth and immune system function. In cancer therapies, synthetic versions such as interleukins and interferons may be administered to:
-
Increase immune cell production.
-
Enhance the cancer-killing attack of the immune system.
5. Oncolytic Virus Therapy
This therapy uses genetically modified viruses that infect and kill cancer cells selectively. Once these viruses lyse cancer cells, they release substances that enhance immune activation. An example is talimogene laherparepvec (T-VEC), which has been approved for melanoma.
Advantages of Immunotherapy for Cancer Treatment Over Conventional Treatments
Conventional cancer therapies such as chemotherapy and radiation kill cancer cells directly but in the process can also harm normal tissues. Cancer immunotherapy follows a different mechanism. It directs the immune system to specifically identify and eliminate cancer cells.
Key benefits are:
-
Precise action: Most immunotherapies target cancer cells or immune mechanisms exclusively and thus minimize harm to normal tissues.
-
Fewer side effects: Side effects are possible but different from those for chemotherapy and potentially less severe in some instances.
-
Long-lasting responses: The immune system will sometimes keep the disease under control indefinitely after treatment is complete.
-
Success in tough-to-treat cancers: Immunotherapy has worked for cancers that often had few, if any, other treatment options, including advanced melanoma.
-
Compatibility with other therapies: It may be used along with chemotherapy, targeted therapy, or radiation to enhance outcomes.
Cancers That Are Sensitive to Immunotherapy
Various types of cancer immunotherapy can be used for these:
-
Melanoma (skin cancer).
-
Non-small cell lung cancer.
-
Kidney cancer (renal cell carcinoma).
-
Bladder cancer.
-
Head and neck cancers.
-
Hodgkin lymphoma.
-
Some forms of leukaemia.
-
Merkel cell carcinoma.
-
Some colorectal cancers with certain genetic alterations.
-
Breast Cancer.
When to consider Immunotherapy for Cancer Treatment?
Physicians might prescribe cancer immunotherapy forms in the following cases:
-
The cancer has particular biomarkers (for example, PD-L1 expression, high microsatellite instability).
-
Chemotherapy or radiation treatments have failed.
-
The cancer is advanced, metastatic, or recurrent.
-
The patient has a cancer type with a good response to immunotherapy.
Possible Risks and Side Effects
There are risks associated with cancer treatment using immunotherapy. Since these treatments stimulate the immune system, they might, at times, get it to target healthy tissues as well as cancer cells.
Side effects that are common:
-
Fatigue.
-
Fever or chills.
-
Nausea.
-
Skin itching or rash.
-
Arthralgias or myalgias.
Less frequent but more serious effects:
-
Inflammation of organs like the lungs (pneumonitis), liver (hepatitis), or colon (colitis).
-
Hormonal gland issues involving the thyroid, pituitary, or adrenal glands.
Conclusion
Cancer immunotherapy is providing a successful alternative to conventional treatments. With numerous forms of immunotherapy available, it can provide enduring results for most patients. Though not for everyone, research continues to increase its scope and impact.
If you or your loved ones are seeking advanced cancer treatment options, talk to the oncology experts at Manipal Hospitals Vijayawada to determine if immunotherapy may be an option for you.
FAQ's
In contrast with chemotherapy, which destroys actively dividing cells (both healthy and unhealthy) directly, immunotherapy attacks cancer cells more selectively by stimulating or steering the immune system to identify and kill cancer cells. This targeted therapy may result in fewer side effects and longer durations of benefit.
The timeline varies by cancer type, treatment method, and individual response. Some patients notice improvement within weeks, while others may take several months. Doctors monitor progress using scans, blood tests, and symptom tracking.
For non-small cell lung cancer, PD-1 or PD-L1-targeting immune checkpoint inhibitors are frequently used and have demonstrated impressive benefits. Selection is based on tumour features and biomarker testing results.
Yes. In other instances, physicians use various combinations of immunotherapies or associate them with chemotherapy, targeted therapy, or radiation to enhance results. Combination therapy is generally based on clinical evidence and patient-specific factors.
Side effects of immunotherapy for cancer depend on the treatment type but can include fatigue, fever, chills, nausea, skin rash, and joint pain. Reporting new or unusual symptoms to your doctor as early as possible can aid in early management of these effects.





















 6 Min Read
6 Min Read