Chronic Kidney Disease (CKD) gradually damages kidney function, often without any obvious signs until the condition becomes severe. Many patients are unaware they have it until much later. Early detection, timely treatment, and lifestyle changes to slow the damage can significantly improve quality of life. Through this blog, a leading nephrologist in Vijayawada provides information about CKD causes and various stages of progression and explains how the disease progresses with different symptoms.
Synopsis
Causes of CKD
Here are the primary causes that lead to the development of CKD:
-
Diabetes: Uncontrolled diabetes increases blood sugar levels, harming the blood vessels in the kidneys, which creates diabetic nephropathy, one of the primary reasons for CKD development.
-
High Blood Pressure (Hypertension): When hypertension persists, it damages blood vessels in the kidneys, gradually decreasing their ability to function properly. Hypertension is one of the primary factors contributing to the development of CKD.
-
Glomerulonephritis: Inflammation of the kidneys' filtering units causes glomerulonephritis. It can result from infections, autoimmune conditions, and additional health-related factors such as other medical conditions.
-
Polycystic Kidney Disease (PKD): PKD is a genetic disorder that causes fluid-filled cysts to form in the kidneys. As these cysts grow, they can damage the kidneys and result in CKD.
-
Chronic Urinary Tract Infections (UTIs): Repeated kidney infections or untreated UTIs can lead to kidney scarring, eventually causing CKD.
-
Obesity: Being overweight or obese increases the risk of developing diabetes, high blood pressure, and other health problems that can contribute to CKD.
-
Smoking: Smoking can damage blood vessels, including those in the kidneys, reducing kidney function over time and increasing the risk of CKD.
Stages of CKD: How the Disease Progresses
Chronic Kidney Disease is categorised into five stages, ranging from mild kidney damage to kidney failure. Managing CKD early can help slow its progression and prevent complications. Here’s a breakdown of the stages of CKD:
-
Stage 1: Mild Kidney Damage: In stage 1, kidney function is near normal, but there may be signs of kidney damage, such as protein or blood in the urine. The Glomerular filtration rate (GFR) is 90 or above. Treatment focuses on controlling blood sugar, blood pressure, and other contributing factors.
-
Stage 2: Mild to Moderate Kidney Damage: Kidney function declines, with a GFR between 60 and 89. Although symptoms may not be noticeable, some damage is occurring. Early intervention and lifestyle changes can slow the progression of CKD.
-
Stage 3: Moderate Kidney Damage: In stage 3, the kidneys are moderately damaged, and GFR falls between 30 and 59. Management of underlying conditions becomes even more critical at this stage.
-
Stage 4: Severe Kidney Damage: At this stage, kidney function is severely impaired, and GFR falls between 15 and 29. Dialysis may be discussed as a future treatment option.
-
Stage 5: End-Stage Renal Disease (ESRD): This is the final stage of CKD, with a GFR below 15. The kidneys can no longer maintain normal bodily functions, and dialysis or a kidney transplant becomes necessary. End-stage renal disease is a serious, life-threatening condition that requires intensive medical care.
Symptoms of CKD at Different Stages
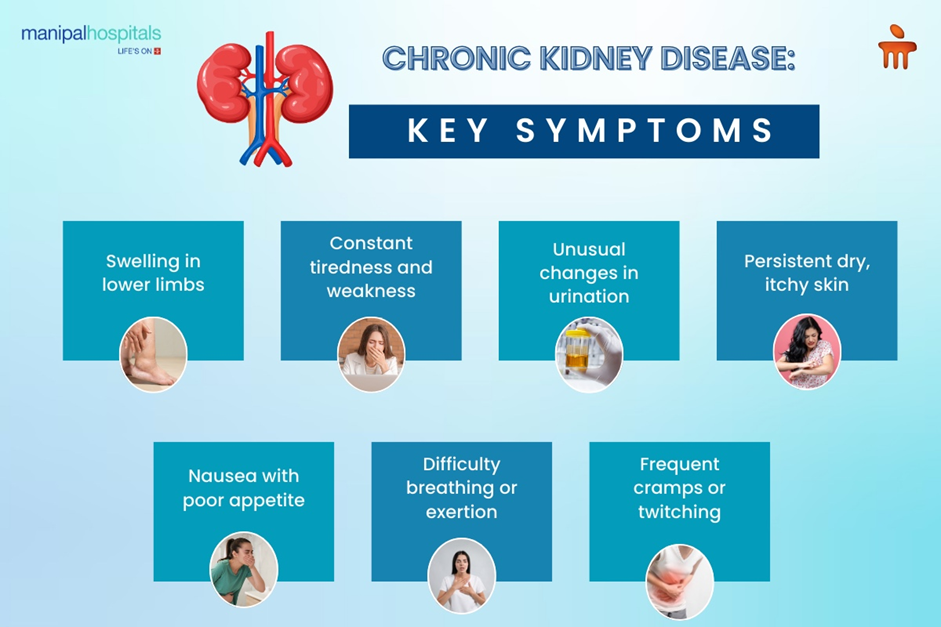
The symptoms of CKD may not appear until the disease has reached a more advanced stage. As CKD progresses, symptoms become more apparent and can affect daily life. Here are the symptoms of CKD at different stages:
-
Stage 1: Often, no symptoms are present. Mild damage may be detected through urine tests or imaging. Some people may experience slight changes in urine output.
-
Stage 2: Mild symptoms like fatigue, back pain, or slight swelling might appear. Blood pressure may rise, and trace amounts of protein might be present in the urine.
-
Stage 3: In this stage, symptoms such as swelling in the legs, ankles, or feet, changes in urine colour, and trouble sleeping can occur. High blood pressure may become harder to manage, and the patient may experience decreased appetite.
-
Stage 4: Symptoms become more pronounced, including chronic fatigue, nausea, shortness of breath, and frequent urination, especially at night. Fluid retention can cause significant swelling, and electrolyte imbalances may make concentration difficult.
-
Stage 5 (ESRD): At this stage, the symptoms are severe and may include confusion, severe swelling, persistent nausea and vomiting, difficulty breathing, and the need for dialysis. Without dialysis or a kidney transplant, kidney failure will occur.
Conclusion
Chronic Kidney Disease (CKD) is a progressive condition that can lead to kidney failure if not adequately managed. Understanding the causes of CKD, recognising its symptoms at different stages, and managing risk factors can help slow its progression. Early detection and treatment are key to maintaining kidney function and preventing complications. Regular screenings and lifestyle changes play a significant role in managing CKD and improving overall health.
FAQ's
The most common causes of CKD are diabetes, high blood pressure, glomerulonephritis, and polycystic kidney disease.
Managing CKD involves controlling blood sugar, maintaining healthy blood pressure, avoiding smoking, and eating a kidney-friendly diet. Regular monitoring is essential.
Symptoms include fatigue, swelling, changes in urination, nausea, and shortness of breath, which often worsen as the disease progresses.
CKD cannot be reversed, but it can be managed to slow its progression. Early detection and treatment are key to preventing further damage.
If you experience symptoms like persistent fatigue, swelling, or changes in urination, consult a doctor for a kidney function evaluation.





















 5 Min Read
5 Min Read