Pancreatic cancer, often dubbed a "silent killer," presents a significant challenge due to its insidious nature. Unfortunately, symptoms of pancreatic cancer often do not manifest until the disease has advanced, making early detection crucial but difficult.
At Manipal Hospitals, we believe in empowering our patients with knowledge, understanding that vigilance and early recognition of pancreatic cancer symptoms are the first step towards better outcomes.
Understanding the signs of pancreatic cancer is paramount for early intervention. This comprehensive guide sheds light on the key warning signs of pancreatic cancer you should be aware of, encouraging you to seek timely medical attention if any of these symptoms arise.
Synopsis
What is Pancreatic Cancer?
Pancreatic cancer begins when abnormal cells in the pancreas grow out of control and form a tumour. The most common type, adenocarcinoma, starts in the cells lining the ducts that carry digestive enzymes out of the pancreas. Because the pancreas is deep inside the body, tumours often grow quite large before they cause any noticeable pancreatic cancer symptoms.
The Silent Threat: 7 Warning Signs of Pancreatic Cancer
Persistent or worsening signs of pancreatic cancer warrant investigation. Here are seven critical pancreatic cancer symptoms you should never ignore:
|
Sign/Symptom |
Description |
Key Indicator |
|
Unexplained Weight Loss |
Losing a significant amount of weight (often 10% or more of body weight within a few months) without trying. |
Tumours affect digestion and metabolism, leading to loss of appetite and muscle wasting. |
|
Jaundice (Yellowing of Skin or Eyes) |
Skin and whites of the eyes turn yellow, often accompanied by dark urine, pale stools, and itchy skin. |
The tumour blocks the bile duct, causing bile backup. This is often one of the most visible pancreatic cancer symptoms, indicating a need for prompt pancreatic cancer treatment. |
|
Abdominal or Back Pain |
A dull ache in the upper abdomen that may radiate to the back. This pancreatic cancer symptom can be constant or intermittent, worsening after eating or lying down. |
Tumour pressing on nerves or organs. Reported by up to 80% of patients as a significant pancreatic cancer symptom. |
|
Changes in Stool |
|
The pancreas isn't producing enough digestive enzymes due to a tumour, leading to improper fat absorption, a key indicator among pancreatic cancer symptoms. |
|
New-Onset or Worsening Diabetes |
Sudden diagnosis of Type 2 diabetes in adults with no risk factors, or rapid worsening of existing diabetes, can be a potential sign of pancreatic cancer. |
A growing tumour impairs the pancreas's insulin production function, leading to elevated blood sugar, a subtle but critical pancreatic cancer symptom. |
|
Nausea, Vomiting, and Loss of Appetite |
|
Tumours can press on the stomach or small intestine, blocking food flow and contributing to weight loss, often linked to other pancreatic cancer symptoms. |
|
Fatigue |
Persistent and overwhelming tiredness that doesn't improve with rest can be another general pancreatic cancer symptom. |
Persistent and overwhelming tiredness that doesn't improve with rest can be another general pancreatic cancer symptom. |
Understanding the Causes of Pancreatic Cancer
While the exact origins of what causes pancreatic cancer are not fully understood, several risk factors have been identified. Understanding what causes pancreatic cancer can help in identifying at-risk individuals:
|
Risk Factor |
Explanation/Impact |
| Smoking |
|
| Obesity |
|
| Diabetes |
|
| Chronic Pancreatitis |
|
| Family History |
|
| Age | The risk increases with age, with most diagnoses of pancreatic cancer occurring after age 45. The median age at diagnosis is 70. |
| Heavy Alcohol Consumption |
|
Diagnosing Pancreatic Cancer
Early and accurate diagnosis is critical for effective pancreatic cancer treatment, and can significantly influence whether pancreatic cancer is curable in your case.
|
Test Type |
Purpose/What it Detects |
|
Blood Tests |
|
|
CT Scan (Computed Tomography) |
Provides detailed cross-sectional images to locate tumours, assess their size, and check for spread to other organs, aiding in planning pancreatic cancer treatment. |
|
MRI (Magnetic Resonance Imaging) |
|
|
Endoscopic Ultrasound (EUS) |
An endoscope with an ultrasound probe is passed down the throat to get close-up images of the pancreas. It can also be used to guide a biopsy for definitive diagnosis of pancreatic cancer. |
|
Biopsy |
A small tissue sample is taken (often during EUS or CT-guided) and examined under a microscope to confirm the presence of cancer cells, which is essential before starting pancreatic cancer treatment. |
|
PET Scan (Positron Emission Tomography) |
Used to detect cancer cells by showing metabolic activity, often combined with CT (PET-CT) to pinpoint areas of spread, crucial for staging and determining the best pancreatic cancer treatment. |
Pancreatic Cancer Treatment Options
The approach to pancreatic cancer treatment is highly individualised and depends on the stage of the cancer, its location, and the patient's overall health. Modern advancements have significantly expanded the arsenal against this disease, leading to improved outcomes for many patients.
|
Treatment Type |
Mechanism/Application |
Goal |
|
Surgery (e.g., Whipple procedure) |
Removal of the tumour and surrounding affected tissues. Procedures like pancreaticoduodenectomy (Whipple) or distal pancreatectomy are key forms of pancreatic cancer treatment. |
Often, the best chance for a cure is for early, localised, resectable pancreatic cancer. Manipal Hospitals' surgical oncology teams have high success rates in this form of pancreatic cancer treatment. |
|
Chemotherapy |
Uses anti-cancer drugs to kill cancer cells throughout the body or slow their growth. Administered intravenously or orally as part of pancreatic cancer treatment. |
Shrink tumours before surgery (neoadjuvant), kill remaining cells after surgery (adjuvant), or control advanced disease progression, making it a versatile pancreatic cancer treatment. |
|
Radiation Therapy |
Uses high-energy X-rays or other particles to destroy cancer cells or inhibit their growth. It can be external beam or internal (brachytherapy) as a component of pancreatic cancer treatment. |
Shrink tumours before surgery, kill residual cells after surgery, or alleviate symptoms like pain in advanced stages of pancreatic cancer. |
|
Targeted Therapy |
Drugs designed to specifically attack cancer cells by targeting unique molecular pathways or proteins involved in cancer growth, offering a precise pancreatic cancer treatment. |
Block specific growth signals or processes unique to cancer cells, often with fewer side effects than traditional chemotherapy. Requires genetic testing for this type of pancreatic cancer treatment. |
|
Immunotherapy |
A newer approach that uses medications to boost the body's own immune system, enabling it to recognise and fight cancer cells more effectively, expanding options for pancreatic cancer treatment. |
Unleash the immune system's power to attack cancer cells. Effective in a subset of patients with specific tumour characteristics for pancreatic cancer. |
|
Palliative Care |
Focuses on providing relief from the symptoms and stress of a serious illness, improving quality of life for both the patient and the family, and is an integral part of holistic pancreatic cancer treatment. |
Manage pain, nausea, fatigue, and other symptoms to enhance comfort and well-being at any stage of pancreatic cancer treatment. |
Advancements in personalised medicine, coupled with multidisciplinary care teams, mean that the 5-year survival rate for pancreatic cancer has improved by over 30% in the last two decades, offering renewed hope for many patients seeking effective pancreatic cancer treatment.
Is Pancreatic Cancer Curable?
The question "Is pancreatic cancer curable?" is complex. While pancreatic cancer is often aggressive, it is curable, especially when detected at an early, localised stage. For patients whose cancer is confined to the pancreas and can be surgically removed as part of their pancreatic cancer treatment, the 5-year survival rate can be as high as 40% or more, depending on various factors and treatment efficacy.
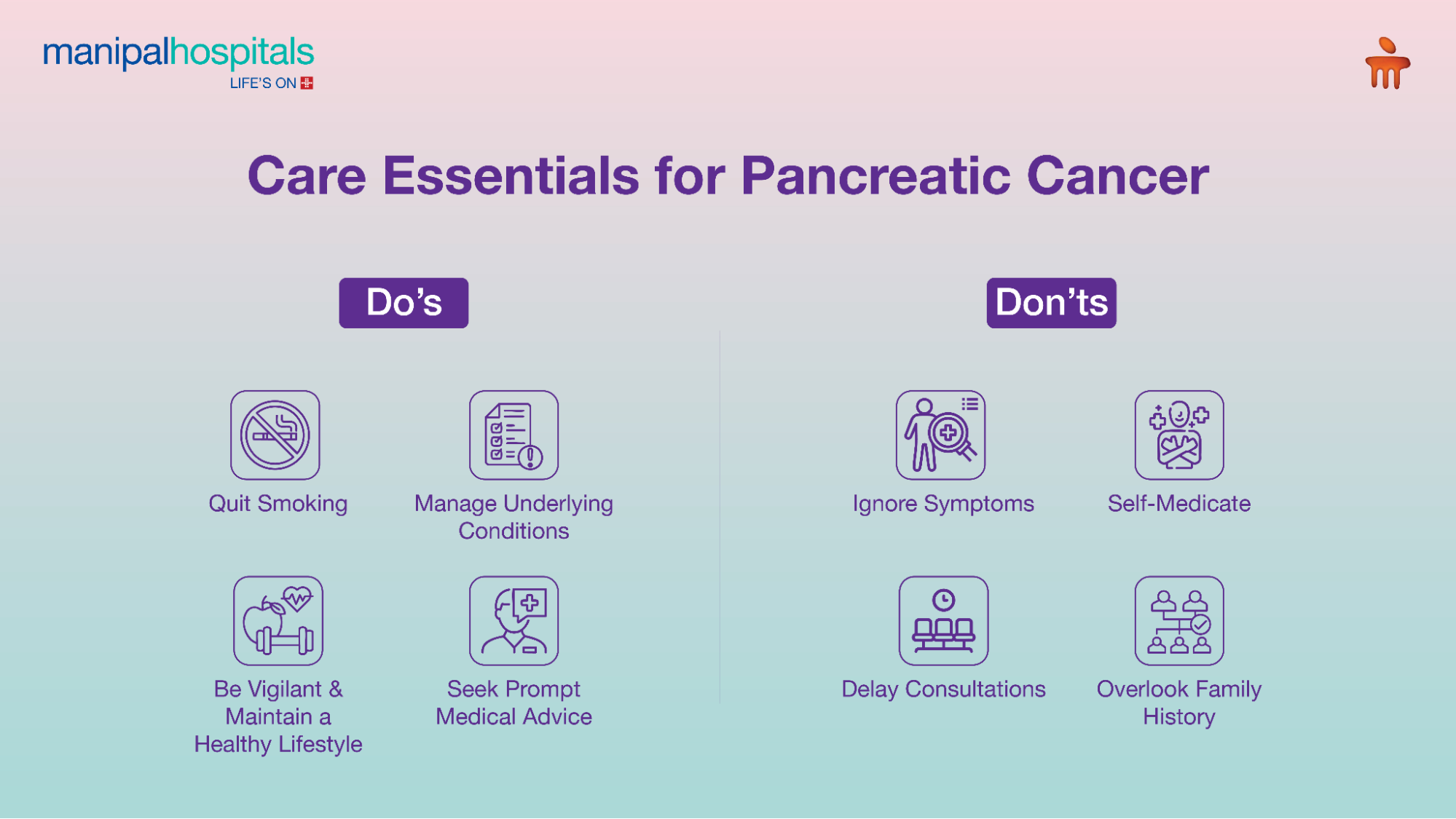
Care Essentials: Do's and Don'ts
|
Do's |
Don'ts |
|
|
|
If you are experiencing these concerning pancreatic cancer symptoms, it's crucial to seek timely medical advice.
FAQ's
Individuals with a history of smoking, obesity, chronic pancreatitis, long-standing diabetes, or a family history of pancreatic cancer are at higher risk. These are key factors in understanding what causes pancreatic cancer.
Reducing risk factors like quitting smoking, maintaining a healthy weight, and managing diabetes can significantly lower your chances of developing pancreatic cancer.
Early detection of pancreatic cancer symptoms dramatically improves treatment success rates. When caught at a localised stage and resectable, 5-year survival rates can increase significantly.
Recovery time varies but can range from several weeks to a few months. It depends on the type of surgery, the patient's overall health, and potential complications.
Currently, there's no routine screening test for pancreatic cancer for the general population to detect early pancreatic cancer symptoms. However, surveillance programs involving endoscopic ultrasound or MRI may be recommended.





















 7 Min Read
7 Min Read