What are Adult Degenerative Scoliotic Deformities?
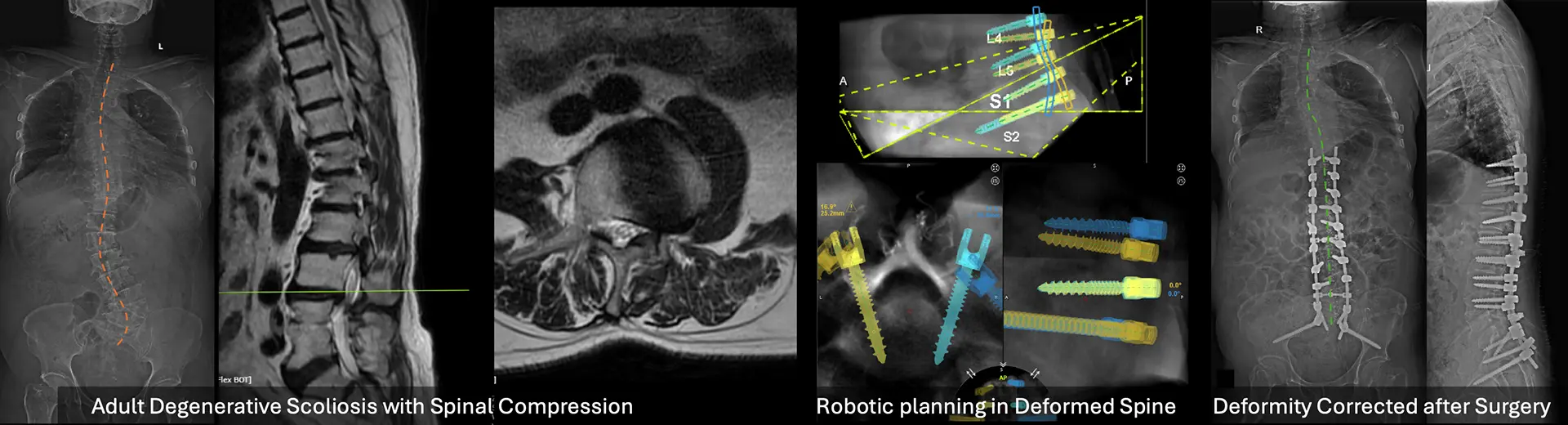
Adult degenerative scoliotic deformities refer to spinal curvature that develops later in life due to age-related changes. Unlike adolescent scoliosis, this condition arises from the gradual degeneration of spinal discs, facet joints, and bones, leading to a sideways curvature, often in the lumbar region. Patients may experience chronic back pain, stiffness, and nerve compression, causing leg pain or numbness.
Poor posture, spinal imbalance, and restricted mobility can significantly affect daily activities. This condition affects individuals over 50 years of age and may worsen over time without appropriate management, which includes physiotherapy, pain relief, and, in severe cases, spinal surgery.
What is Posterior Instrumented Scoliosis Correction for Adult Degenerative Scoliotic Deformities?
Experienced spine surgeons in Bangalore perform posterior instrumented scoliosis correction to address adult degenerative scoliosis in patients suffering from spinal degeneration due to age-related damage to spinal discs and joints. It may cause nerve compression symptoms, discomfort, and postural problems.
This procedure uses metal implants and spinal fusion to provide stability, correct abnormal curvature, and prevent future deterioration. The posterior approach involves accessing the spine through an incision in the back. Spine surgeons prefer this technique as it offers direct access to affected spinal areas for stabilisation and realignment. It provides durable support for the weakening spinal structure and proves beneficial in adult degenerative scoliosis.
Benefits of the Procedure:
Patients with adult degenerative scoliosis gain significant benefits from posterior instrumented scoliosis correction through improved spinal alignment, functional capability, and quality of life. These are the main advantages patients receive from this surgery.
-
Significant pain relief: The procedure helps decompress pinched nerves caused by curvature and degeneration, reducing radiating pain, numbness, or weakness in the legs and back. It also stabilises the spine, which minimises the chronic mechanical pain linked to spinal instability.
-
Improved spinal alignment and posture: By correcting the abnormal curvature, the surgery restores natural spinal alignment. This improves posture, reduces leaning or tilting, and enhances the ability to walk, stand, and perform daily activities comfortably.
-
Enhanced quality of life: Many patients report major improvement in performing everyday tasks without assistance. Pain-free movement and improved posture can restore the freedom to enjoy hobbies, social interactions, and regular routines.
-
Prevention of further spinal deformity: Stabilising the spine with surgical implants prevents further deterioration of discs and vertebrae. This protects nearby spinal structures and reduces the risk of worsening curvature over time.
-
Surgeons create personalised treatment plans based on curve severity, bone quality, and overall health to ensure optimal correction with minimal complications and long-term benefits.
-
Reduction in neurological symptoms: By relieving pressure on compressed spinal nerves, the procedure often improves nerve-related symptoms like numbness, tingling, or muscle weakness, restoring strength and sensation in the lower limbs.
Indications for Posterior Instrumented Scoliosis Correction for Adult Degenerative Scoliotic Deformities:
This procedure is recommended for adults experiencing progressive spinal curvature due to degenerative changes. When non-surgical treatments fail to provide relief and the quality of life is affected, surgical correction becomes necessary. Below are the key clinical indications for considering this advanced spinal surgery:
-
Progressive Spinal Curvature: A noticeable increase in the degree of spinal curvature over time, often seen on serial X-rays, despite conservative treatment efforts.
-
Chronic Back Pain Unresponsive to Non-Surgical Treatments: Persistent, debilitating back pain that doesn't improve with medications, physiotherapy, or bracing and severely limits daily functioning.
-
Spinal Imbalance and Postural Deformity: Leaning forward or to one side, stooped posture, or difficulty maintaining an upright position due to spinal misalignment.
-
Neurological Symptoms from Nerve Compression: Tingling, numbness, burning pain, or muscle weakness in the legs due to nerves being pinched by the deformed spine.
-
Reduced Walking Tolerance or Leg Pain While Walking (Neurogenic Claudication): Pain, heaviness, or fatigue in the legs that worsens with walking and improves with rest, indicating spinal canal narrowing.
-
Failed Response to Conservative Management: Lack of improvement after prolonged non-surgical care like physical therapy, medications, or spinal injections.
-
Structural Deformity Causing Cosmetic or Functional Concerns: Visible spinal deformity that affects appearance or interferes with personal, social, or occupational life.
Key Aspects of the Surgical Procedure:
This complex spinal surgery is carefully planned and executed to safely correct the curvature, decompress nerves, and stabilise the spine. It involves several crucial steps and considerations to ensure the best outcomes for adult patients with degenerative scoliosis:
-
Posterior Surgical Approach: The surgery is performed through an incision along the back (posterior side), allowing direct access to the spine for correction and stabilisation.
-
Spinal Decompression: Bone and tissue pressing on spinal nerves are removed (laminectomy or foraminotomy), relieving nerve compression and associated symptoms like pain or numbness.
-
Spinal Instrumentation with Rods and Screws: Metal implants such as pedicle screws and rods are inserted into the vertebrae to realign and support the spine during and after correction.
-
Curve Correction and Realignment: Specialised tools are used to gradually straighten the curved spine, restoring natural alignment and improving overall balance and posture.
-
Spinal Fusion with Bone Grafting: Bone grafts (from the patient or donor) are placed along the spine to promote bone fusion over time, creating a solid, stable structure.
-
Use of Intraoperative Neuromonitoring: Real-time monitoring of spinal cord and nerve function ensures safety during surgery, helping avoid neurological injury during correction.
-
Postoperative Immobilization and Recovery Planning: Patients may require braces and physical therapy to aid recovery, support healing, and regain strength and function in the long term.
Will I Need Any Pre-Procedure Investigations?
Yes, a series of tests ensures patient safety and a personalised treatment plan. These include:
-
X-rays & MRI scans to assess spinal alignment.
-
Pulmonary function tests (PFTs) are used to evaluate breathing capacity.
-
Neurological assessments to detect nerve compression.
-
Blood tests & cardiac screening for anaesthesia safety.
What Happens During the Procedure?
-
Anaesthesia & Patient Positioning – The patient is placed face-down under general anaesthesia.
-
Incision & Exposure – A midline incision is made to access the spine.
-
Instrumentation Placement – Screws, rods, and hooks are inserted to straighten the spine.
-
Spinal Fusion – Bone grafting fuses vertebrae for long-term stability.
-
Closure & Recovery – The incision is closed, and post-operative monitoring begins.
How Long Does Recovery Take?
The recovery timeline for Posterior Instrumented Scoliosis Correction varies depending on the patient's overall health, age, the severity of scoliosis, and adherence to post-operative care guidelines. However, the general recovery process can be broken down into different stages:
1. Hospital Stay (First Few Days)
-
After surgery, patients typically stay in the hospital for 4 to 7 days for close monitoring.
-
Pain management is initiated using intravenous (IV) pain medications, which later transition to oral medications.
-
Physical therapy starts early to encourage movement and prevent complications such as blood clots or muscle stiffness.
-
Patients are assisted in sitting, standing, and taking short walks under supervision.
2. Early Recovery Phase (First 6 to 8 Weeks)
-
Limited physical activity: Patients are advised to avoid bending, twisting, and heavy lifting to protect the healing spine.
-
Use of braces (if recommended): In some cases, a spinal brace may be prescribed to provide extra support during the healing process.
-
Gradual improvement in mobility: Walking is encouraged, but strenuous activities must be avoided.
-
Pain management continues with prescribed medications as needed.
-
Patients may require assistance at home for daily activities such as dressing and cooking.
3. Intermediate Recovery (3 to 6 Months)
-
By this time, patients usually experience significant pain reduction and improved mobility.
-
Physical therapy becomes more intensive to rebuild strength, flexibility, and balance.
-
Patients can resume light daily activities, such as desk work and short walks, but high-impact activities are still restricted.
-
The fusion process in the spine continues as bone grafts heal and integrate with the vertebrae.
4. Long-Term Recovery (6 Months to 1 Year and Beyond)
-
Most patients regain full mobility and function within 6 to 12 months.
-
Regular follow-up visits with the surgeon are necessary to assess healing and spine alignment.
-
Patients are encouraged to engage in low-impact exercises, such as swimming or yoga, to maintain spinal flexibility and strength.
-
In some cases, full fusion of the spine may take up to 1 to 2 years, depending on individual healing rates.
At MIRSS, patients receive expert care, cutting-edge technology, and comprehensive post-operative support for the best possible outcomes. Consult our specialists today!
How to Know if I Am Eligible for Posterior Instrumented Scoliosis Correction for Adult Degenerative Scoliotic Deformities?
Eligibility is determined by spine specialists, spine surgeons, anaesthesiologists, and physiotherapists at MIRSS. Factors considered include:
Severity of Spinal Curvature (Cobb Angle Measurement)
-
Mild cases (10-25 degrees): Managed with physiotherapy.
-
Moderate cases (25-40 degrees): May require surgery.
-
Severe cases (above 40-50 degrees): Strong candidates for surgical correction.
Progression of the Condition
-
Rapidly worsening scoliosis necessitates early surgical intervention.
Impact on Daily Life
-
Chronic pain, mobility issues, and breathing difficulties increase the need for surgery.
Overall Health and Medical Fitness
-
Patients undergo cardiac, neurological, and pulmonary evaluations to assess surgery suitability.
Risks of Posterior Instrumented Scoliosis Correction for Adult Degenerative Scoliotic Deformities?
Like any major spinal surgery, Posterior Instrumented Scoliosis Correction carries certain risks and potential side effects. While most patients experience successful outcomes, it is important to be aware of the possible complications.
1. Infection - Post-surgical infections can occur in approximately 2-8% of cases. These can be superficial (affecting the skin) or deep (impacting the spinal hardware or bone grafts). Patients typically receive antibiotics to reduce this risk.
2. Blood Clots (Deep Vein Thrombosis - DVT) - Prolonged immobility after surgery increases the risk of blood clot formation in the legs, which can lead to pulmonary embolism if left untreated. Compression stockings, blood thinners, and early movement help prevent this.
3. Nerve Damage - Since the surgery involves working near the spinal cord and nerves, there is a small risk of nerve injury. This may result in numbness, weakness, or even loss of function in the legs, although such complications are rare.
4. Non-Union (Failure of Bone Fusion) - In some cases, the spinal bones may not fuse properly, leading to persistent pain or instability. Smoking, osteoporosis, and poor nutrition can increase this risk. If non-union occurs, a revision surgery may be required.
5. Pain and Stiffness - Some patients experience chronic pain or reduced spinal flexibility post-surgery, particularly in older adults or those with extensive spinal fusion. Physical therapy and regular movement help manage stiffness.
6. Hardware Complications - The metal rods, screws, and plates used in the procedure can sometimes become loose, break, or shift, requiring additional surgery. Regular follow-ups help detect such issues early.
7. Blood Loss - Spinal surgeries often involve significant blood loss, and some patients may need a blood transfusion during or after the procedure.
Why Choose MIRSS for Posterior Instrumented Scoliosis Correction?
Choosing the right medical centre for spinal surgery is crucial for achieving the best outcome. MIRSS offers world-class expertise, cutting-edge technology, and comprehensive post-surgical care to ensure a safe and successful recovery. If you are in search of the best spine surgery hospital in Bangalore, choose MIRSS for these reasons.
1. Expert Multidisciplinary Team
-
Highly experienced robotic spine surgeons, spine care specialists, and physiotherapists collaborate for successful outcomes.
-
Extensive experience in complex spinal deformity correction.
2. Cutting-Edge Surgical Technology
-
Intraoperative navigation systems for precise screw placement.
-
3D imaging and robotic-assisted surgery for enhanced surgical accuracy.
-
Neuro-monitoring technology to prevent neurological complications.
3. Comprehensive Pre- and Post-Operative Care
-
Pre-surgery evaluations, including X-rays, MRI scans, and physical assessments, ensure a well-prepared surgical approach.
-
Personalised rehabilitation programs involving physiotherapy and mobility training accelerate recovery.
4. Proven Track Record
-
Successfully treated numerous adult degenerative scoliosis cases, improving both function and aesthetics.
-
High success rates and patient testimonials highlight excellence in spinal corrective surgeries.