Patient-Friendly Summary
Kyphosis is a condition where your spine curves excessively forward, causing a rounded back. When non-surgical treatments aren't effective, Posterior Instrumented Kyphosis Correction can help. This surgery uses specialised rods and screws to realign your spine, reduce pain, improve your posture, and enhance your quality of life. Recovery typically takes 4-7 days in the hospital, followed by a gradual return to normal activities over several months. At Manipal Hospitals, our expert spine surgeons provide personalised care using advanced techniques for optimal results.
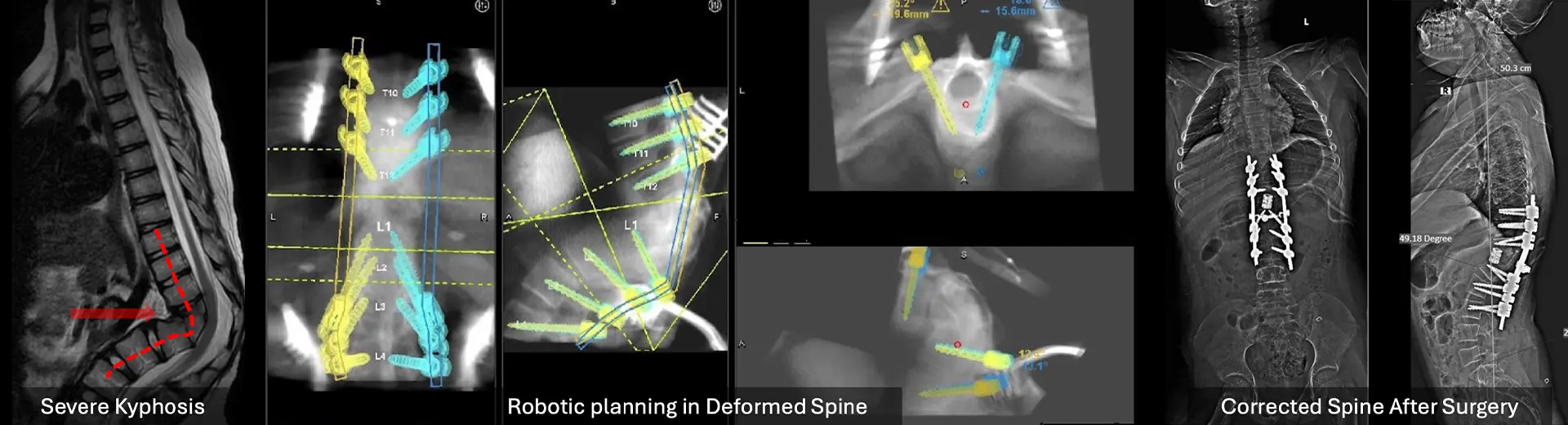
Introduction: Why Kyphosis Correction Matters
Kyphosis significantly impacts both physical health and emotional wellbeing. Beyond the visible hunched posture, untreated kyphosis can lead to chronic pain, limited mobility, breathing difficulties, and even neurological problems. The excessive forward curvature of the spine, typically in the thoracic (upper back) region, progressively worsens if left untreated, leading to significant postural deformities that can severely compromise quality of life. For patients whose kyphosis doesn't respond to conservative treatments like physical therapy and bracing, surgical intervention becomes essential to prevent further deterioration and associated complications. Posterior Instrumented Kyphosis Correction offers hope to those struggling with severe or progressive kyphosis, not only correcting spinal alignment but also preventing future complications, ultimately restoring patients' confidence and ability to live an active life.
What Is Posterior Instrumented Kyphosis Correction?
Posterior Instrumented Kyphosis Correction is a specialised surgical procedure that addresses abnormal forward curvature of the spine. Through an incision in the back (posterior approach), surgeons use advanced implants (rods and screws) to carefully realign vertebrae to their natural position. This transformative surgery not only restores spinal alignment but also relieves pain and enhances mobility for patients suffering from kyphosis.
The procedure typically includes spinal fusion, which permanently stabilises the corrected spine alignment. The specialised implants serve as anchor points, allowing surgeons to execute precise adjustments through the posterior approach. During surgery, the abnormal spinal curvature is methodically corrected while simultaneously promoting spinal fusion, ensuring long-term stability of the newly aligned spine.
Types Of Kyphosis Correction Procedures
1. Posterior Spinal Fusion with Instrumentation
-
Most common approach for kyphosis correction
-
Uses rods, screws, and bone grafts to stabilize and realign the spine
-
Creates permanent fusion to maintain the corrected posture
-
Ideal for progressive kyphosis, structural deformities, or significant pain
-
Provides excellent long-term stability through permanent fusion of the treated vertebrae
-
Allows for significant correction of the kyphotic deformity in a single procedure
2. Osteotomy-Based Correction
For severe or rigid deformities requiring greater spinal flexibility:
-
Smith-Petersen Osteotomy (SPO): Removes posterior elements for mild to moderate deformities. This technique involves the removal of a small portion of the posterior spinal elements to increase flexibility and allow for controlled correction.
-
Pedicle Subtraction Osteotomy (PSO): Removes a wedge of vertebral body bone for greater correction. This more extensive procedure provides significant correction capabilities for severe, rigid deformities by removing a wedge-shaped section of the vertebra.
-
Vertebral Column Resection (VCR): Reconstructs multiple vertebrae in extreme cases. This highly complex procedure involves the complete removal of one or more vertebrae and is reserved for the most severe and rigid deformities that cannot be adequately corrected with other techniques.
-
Each osteotomy technique is carefully selected based on the severity of the deformity, the patient's overall health, and the degree of correction needed.
3. Growth Modulation Surgery
Specifically for children with growing spines:
-
Uses tethering systems and guided growth implants
-
Provides gradual correction over time
-
Reduces need for early spinal fusion
-
Preserves natural spine motion and growth potential
-
Involves less invasive techniques than traditional fusion procedures
-
May be followed by definitive fusion surgery once skeletal maturity is reached, if needed
4. Hybrid Techniques
-
Combining different surgical strategies for complex cases
-
Incorporates posterior fusion with anterior support elements
-
Uses interbody devices or cages for enhanced stability
-
Addresses complex deformities that may involve multiple spinal regions
-
May be performed as single or staged procedures depending on complexity
-
Customised approach based on individual patient anatomy and deformity characteristics
Benefits of Kyphosis Correction
-
Improved Posture and Alignment: Restoration of natural spinal curves enhances overall body alignment and physical appearance
-
Significant Pain Reduction: Alleviates chronic back pain associated with kyphotic deformities by removing abnormal stress on spinal structures
-
Prevention of Further Deformity: Stabilises the spine to halt progression of the curvature, particularly important in growing individuals
-
Enhanced Mobility and Quality of Life: Improves functional capacity for daily activities, work, and recreational pursuits
-
Better Organ Function: Particularly improved lung capacity as the corrected posture creates more space for the lungs to expand fully
-
Reduced Pressure on Nerves: Alleviates compression of spinal nerves that can cause radiating pain, numbness, or weakness
-
Psychological Benefits: Improved self-image and confidence from corrected posture and reduced visible deformity
Who Needs Kyphosis Correction?
Conditions Requiring Surgical Intervention
1. Congenital Kyphosis
-
Present at birth due to spinal malformations
-
Often requires intervention during childhood or adolescence
-
Usually caused by failure of vertebral formation or segmentation during embryonic development
-
Highly variable in severity and progression rate
-
Early detection and treatment are critical to prevent severe deformity
2. Scheuermann's Kyphosis
-
Developmental disorder is common in adolescents
-
Causes excessive thoracic curvature and pain
-
Characterised by wedging of at least three adjacent vertebrae
-
Typically presents during growth spurts with progressive deformity
-
Often accompanied by back pain that worsens with activity and improves with rest
3. Post-Traumatic Kyphosis
-
Results from spinal fractures or injuries
-
Surgery restores stability and prevents progression
-
Often develops gradually after vertebral fractures heal in a collapsed position
-
May cause both mechanical pain and neurological symptoms
-
Surgical correction is more complex due to altered anatomy from the initial trauma
4. Degenerative Kyphosis
-
Affects older adults with osteoporosis or disc degeneration
-
Causes pain, poor posture, and reduced mobility
-
Often accompanied by multiple compression fractures in osteoporotic patients
-
Progressive deterioration of spinal alignment with age
-
Frequently associated with forward head posture and difficulty maintaining an upright position
5. Neuromuscular Kyphosis
-
Associated with conditions like cerebral palsy or muscular dystrophy
-
Surgery improves posture and function
-
Results from muscle imbalance and inability to maintain proper posture
-
Often rapidly progressive during growth periods
-
May be associated with pelvic obliquity and scoliosis
6. Post-Surgical Kyphosis
-
Develops as a complication after previous spinal surgeries
-
Requires revision surgery to restore proper alignment
-
Can result from inadequate fixation, implant failure, or adjacent segment degeneration
-
May develop gradually as adjacent segments compensate for fused levels
-
Often, more technically challenging to correct than primary deformities
When Is Surgery Recommended?
IMPORTANT: Surgery is considered when one or more of these factors are present
-
Severe curvature (greater than 70-80 degrees): Extreme kyphosis creates significant mechanical stress on the spine and may compromise respiratory function
-
Chronic pain unresponsive to conservative treatment: Persistent pain that significantly affects quality of life despite medication, physical therapy, and activity modification
-
Neurological symptoms (numbness, weakness, tingling): Signs of nerve or spinal cord compression require urgent attention to prevent permanent neurological damage
-
Breathing difficulties due to chest compression: Severe kyphosis can restrict lung expansion, leading to reduced respiratory capacity and potential cardiopulmonary complications
-
Significant functional limitations affecting daily activities: Inability to perform routine activities due to pain, stiffness, or postural constraints
-
Failed non-surgical treatment like bracing, especially in growing children: Continued progression despite appropriate conservative management, particularly concerning in skeletally immature patients
The Surgical Procedure: What To Expect
Pre-Surgery Preparation
-
Comprehensive medical assessments (blood tests, imaging studies)
-
Evaluation by spine anesthesiologists to identify potential risks and optimise pain control
-
Customised surgical planning based on your specific condition, integrating 3D imaging and computer modelling when appropriate
-
Fasting instructions to ensure safe anaesthesia
-
Medication adjustments to minimise bleeding risk and potential interactions
-
Nutritional optimisation to promote wound healing and recovery
-
Smoking cessation recommendations to improve fusion success rates
-
Patient education about the procedure, recovery process, and rehabilitation expectations
Step-by-Step Surgical Process
Anaesthesia and Positioning
-
General anaesthesia ensures you're comfortable and pain-free throughout the procedure
-
Careful positioning on the operating table with protective padding for all pressure points
-
Creation of a sterile surgical field to minimise infection risk
-
Placement of neuromonitoring electrodes to track nerve function during surgery
Accessing the Spine
-
Midline incision along the back over the affected segments
-
Gentle retraction of muscles to expose the vertebrae
-
Careful dissection of soft tissues to minimise blood loss and preserve muscle function
-
Identification of key anatomical landmarks to guide instrumentation placement
Correcting the Deformity
-
Placement of pedicle screws as anchor points, carefully navigated to ensure proper trajectory and depth
-
Custom-contoured rods attached to screws, shaped specifically to match the desired spinal curvature
-
Osteotomy (bone removal) if needed for severe cases, is carefully executed to maintain spinal stability
-
Gradual, controlled realignment of the spine with continuous neuromonitoring to protect the spinal cord
-
Sequential tightening of the construct to achieve optimal correction while distributing forces safely
Fusion and Stabilisation
-
Application of bone grafts to promote fusion between the treated vertebrae
-
May use your own bone (harvested from the pelvis) or synthetic substitutes
-
Meticulous preparation of the fusion surfaces to optimise bone healing
-
Additional structural support with interbody devices when needed for anterior column stability
-
Final tightening and securing of all hardware components
Closure and Dressing
-
Final inspection of hardware placement and deformity correction
-
Careful closure of tissues with multiple layers of sutures or staples
-
A sterile dressing was applied to protect the surgical site
-
Placement of surgical drains, if necessary, to prevent fluid accumulation
-
Application of a spinal brace is indicated for additional external support
Recovery Timeline
Callout Box: Recovery Milestones
Hospital Stay (4-7 Days)
-
First 24-48 hours: Monitoring in ICU with specialised nursing care
-
Early mobilisation: Within 4-6 hours post-surgery to prevent complications
-
Physical therapy: Begins within 24-48 hours with gentle movements and breathing exercises
-
Pain management: IV medications transitioning to oral pain relievers
-
Wound care and monitoring for signs of infection or other complications
-
Training in proper body mechanics for safe movement during healing
Early Recovery (First Month)
-
Limited bending, twisting, or lifting (typically restricted to 5 pounds)
-
Short walks with a gradual increase in distance as tolerated
-
Basic self-care activities with modifications as needed
-
Regular wound checks and suture/staple removal
-
Initial follow-up imaging to confirm proper alignment
Intermediate Recovery (2-3 Months)
-
Structured physical therapy program focusing on core strengthening
-
Gradual return to light household activities
-
Driving may be permitted (if not taking narcotic pain medication)
-
Progressive increase in walking distance and duration
-
Continued medication management for comfort
Advanced Recovery (3-6 Months)
-
More intensive rehabilitation to restore strength and flexibility
-
Return to non-contact recreational activities
-
Resumption of most normal daily activities with some precautions
-
Follow-up imaging to assess fusion progress
-
Possible return to sedentary or light-duty work
Long-Term Recovery (6-12 Months)
-
Final fusion maturation and maximum functional improvement
-
Gradual return to more demanding physical activities as approved by the surgeon
-
Potential return to contact sports or heavy physical labour (if appropriate)
-
Long-term maintenance exercises to support spinal health
-
Regular follow-up appointments to monitor long-term outcomes
Am I A Candidate For Kyphosis Correction?
Your eligibility will be determined through:
Clinical Examination
-
Assessment of spinal curvature and posture using forward bending tests and standing evaluation
-
Evaluation of pain patterns, intensity, and factors that improve or worsen symptoms
-
Check for balance and gait issues that may indicate neurological involvement
-
Assessment of overall spinal alignment, including compensatory curves
-
Evaluation of the flexibility or rigidity of the deformity through manual testing
Comprehensive Imaging
-
X-rays to measure kyphotic angle (Cobb angle) in both standing and supine positions
-
MRI to assess spinal cord and nerve involvement, disc health, and soft tissue abnormalities
-
CT scan for detailed 3D bone structure evaluation, particularly important for surgical planning
-
Bone density studies to assess for underlying osteoporosis in adult patients
-
Flexibility X-rays to determine how correctable the deformity is without osteotomy
Neurological Assessment
-
Tests for nerve compression signs, including reflex testing and strength evaluation
-
Evaluation of sensory function in the extremities
-
Assessment of bladder and bowel function if spinal cord compression is suspected
-
Specialised testing, such as electromyography (EMG), if needed to quantify nerve function
-
Assessment of fine motor coordination and balance
General Health Evaluation
-
Age and overall health considerations to ensure safety during anaesthesia and recovery
-
Assessment of pre-existing conditions like diabetes, heart disease, or respiratory issues
-
Ability to tolerate anaesthesia and major surgery
-
Nutritional status and body mass index assessment
-
Psychological readiness and understanding of the recovery process
-
Support system evaluation to ensure adequate assistance during recovery
Potential Risks And Considerations
Safety Information
While Posterior Instrumented Kyphosis Correction is generally safe, potential risks include:
-
Infection (incision site or around implants): Occurs in approximately 1-5% of cases and is managed with antibiotics and possibly surgical debridement
-
Blood loss during surgery: Minimised through careful surgical technique and blood conservation strategies
-
Nerve injury (causing weakness, numbness, or tingling): Risk reduced through neuromonitoring and precise surgical technique
-
Fusion failure (rare): More common in smokers, patients with osteoporosis, or those with certain medical conditions
-
Hardware complications: Such as screw loosening or rod breakage, which may require revision surgery
-
Adjacent segment degeneration: Accelerated wear of the spinal segments above or below the fusion
-
Temporary post-operative discomfort: Managed through a comprehensive pain management protocol
Your surgeon will discuss these risks and how we minimise them through advanced techniques and expert care. We implement rigorous protocols to reduce complications, including prophylactic antibiotics, meticulous surgical technique, and specialised post-operative care.
Why Choose MIRSS?
Surgical Excellence
-
Advanced 3D imaging and robotic-assisted techniques for precision surgery, reducing complications and improving outcomes
-
Intraoperative neuromonitoring to protect spinal cord function during surgery
-
Minimally invasive approaches, when appropriate, to reduce recovery time and post-operative pain
-
Fellowship-trained surgeons specialising exclusively in complex spinal deformity correction
-
Regular participation in international spine surgery conferences to stay current with the latest techniques
Comprehensive Care Approach
-
Personalised treatment plans tailored to your specific condition, age, lifestyle needs, and goals
-
Multidisciplinary team including surgeons, physiotherapists, pain specialists, and rehabilitation experts
-
Cutting-edge facilities with the latest surgical and monitoring equipment
-
Dedicated spine surgery operating rooms with specialised staff and equipment
-
Pre-operative optimisation programs to ensure you're in the best possible condition for surgery
-
Specialised spine anaesthesia team experienced in complex deformity surgeries
Patient-Centered Recovery
-
Individualised rehabilitation programs are designed for optimal recovery based on your specific procedure and needs
-
Specialised pain management protocols for a comfortable post-surgical experience
-
Ongoing support throughout your recovery journey with regular follow-up appointments
-
Dedicated spine rehabilitation unit with therapists specialised in post-surgical spinal care
-
Patient education resources to support your understanding of the recovery process
-
Support groups connect you with others who have undergone similar procedures
Recognition and Outcomes
-
Accredited Centre of Excellence for spine surgery by national and international organisations
-
Published research on innovative kyphosis correction techniques
-
Lower complication rates than national averages for complex spinal procedures
-
High patient satisfaction scores reflect our commitment to quality care
-
Recognised leadership in spine surgery education and training