What is Instability Secondary to Trauma, Infection, Inflammatory, or Neoplastic Pathologies?
Instability refers to the weakening of the spine caused by conditions such as trauma, infection, inflammation, or neoplastic (tumour-related) pathologies. Accidents and falls result in spinal misalignment through fractures or ligament destruction. Tuberculosis and osteomyelitis infections attack vertebrae, increasing the breakdown of spinal structures and raising the chance of vertebral collapse. Rheumatoid arthritis and other inflammatory diseases erode spinal structures, reducing stability and causing substantial pain.
Neoplastic conditions, such as tumours, can damage bone structures, leading to spinal deformities. Symptoms include severe pain, nervous system impairment, and reduced mobility. Diagnosis uses imaging procedures and clinical exams before healthcare professionals determine treatments, ranging from braces to surgeries for stabilisation.
What Is Occipito-Cervical Fusion for Instability Secondary to Trauma, Infection, Inflammatory, or Neoplastic Pathologies?
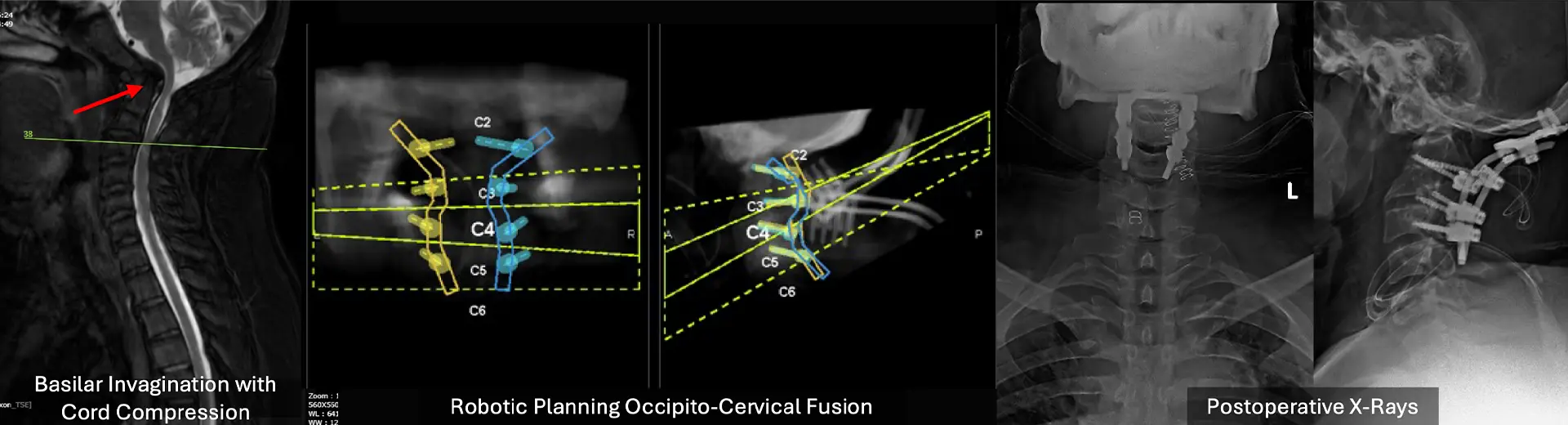
Occipito-cervical fusion surgery stabilises the skull (occiput) and upper cervical spine joints. This junction serves essential roles in head mobility, posture maintenance, and neurological control. The surgical fusion prevents excessive joint movement that endangers the spinal cord after structural stability is compromised from trauma, infection, inflammatory conditions, or tumours.
The procedure uses plates, rods, and screws to stabilize the skull and cervical vertebrae. The surgery also promotes natural bone fusion for long-term stability. This treatment relieves pain, prevents neurological decline, and restores function by supporting the craniovertebral junction.
Surgery becomes necessary when instability worsens, neurological symptoms progress, or pain resists initial treatment. The primary objective is functional stabilisation and preservation of neurological capacities to improve quality of life. Modern techniques have improved outcomes, effectively correcting spinal misalignment and controlling instability-related issues.
What Health Conditions Require Occipito-Cervical Fusion?
Occipito-cervical instability can arise from various pathological conditions that compromise spinal integrity. When these conditions lead to progressive instability, fusion surgery becomes essential to prevent neurological complications and restore function.
Common Conditions Requiring Occipito-Cervical Fusion:
-
Traumatic Injuries Leading to Instability: Severe accidents, such as motor vehicle collisions or falls, can cause fractures or ligamentous injuries at the craniovertebral junction. If conservative management fails, fusion surgery stabilises the region, preventing further damage.
-
Infectious Causes of Cervical Instability: Conditions like tuberculosis, osteomyelitis, or abscess formation can erode vertebral structures, leading to instability. Surgical stabilisation is necessary in such cases to restore spinal integrity and prevent neurological decline.
-
Inflammatory Conditions Affecting the Craniovertebral Junction: Diseases like rheumatoid arthritis can weaken ligaments and bones in the upper cervical spine. When instability progresses to a stage where nerve compression occurs, occipito-cervical fusion is the definitive treatment.
-
Neoplastic Pathologies Leading to Spinal Instability: Tumours, whether primary or metastatic, can destroy vertebral bone, leading to instability and spinal cord compression. Fusion surgery helps restore structural integrity while preventing further deterioration.
Indications for Occipito-Cervical Fusion Surgery
Occipito-cervical fusion becomes essential when non-surgical treatments fail to eliminate spinal instability, pain, and neurological deficits affecting the craniovertebral zone. In these cases, medications and therapies have not controlled symptoms, necessitating surgical intervention.
Surgery is indicated to prevent spinal cord compression from unstable conditions, causing tingling, numbness, weakness, and postural problems. Without proper treatment, these conditions can progress to severe neurological impairment affecting arm and leg mobility.
Occipito-cervical fusion is also necessary when anatomical disruption from trauma, tumours, or inflammatory diseases weakens the spinal structure. If imaging confirms progressive vertebral displacement or spinal cord compression, stabilisation prevents further deterioration. The surgery provides a definitive solution by reinforcing the affected region, allowing patients to regain stability and improve long-term spinal health.
Key Aspects of Occipito‑Cervical Fusion
-
Patient Selection & Preoperative Imaging: High‑resolution CT and MRI assess bony anatomy, ligamentous integrity, and vertebral artery course. Dynamic radiographs confirm instability at the occiput–C1 or C1–C2 junction.
-
Anaesthesia & Neuromonitoring: General anaesthesia with intra‑operative neurophysiological monitoring (somatosensory and motor evoked potentials) safeguards spinal‑cord function throughout instrumentation.
-
Patient Positioning: The patient lies prone on a radiolucent frame with the head secured in a Mayfield clamp, ensuring neutral alignment and minimising venous engorgement. All pressure points are carefully padded.
-
Posterior Midline Exposure: A midline incision extends from the inion to C2/C3. Subperiosteal dissection of paraspinal muscles exposes the occipital bone, posterior arch of C1 (if present), and C2 laminae.
-
Occipital Plate Placement: The occipital keel is burred to create a flat surface. An occipital plate is positioned and fixed with bicortical screws, taking care to avoid the dural venous sinuses.
-
Cervical Screw Fixation: Bilateral C2 pedicle or pars screws are placed under fluoroscopic or navigational guidance. Lateral‑mass screws in C3 (and C4 if needed) provide additional caudal anchor points.
-
Rod Contouring & Connection: Pre‑contoured rods are seated into the occipital plate and cervical screw heads. Compression or distraction manoeuvres restore the desired occipito‑cervical alignment before locking.
-
Bone Grafting & Fusion Bed Preparation: Decortication of the occipital bone, C1 posterior arch (if intact), and C2 laminae creates a vascular bed. Autograft (or allograft) is laid to promote solid arthrodesis.
-
Wound Closure & Drainage: Layered closure of fascia, subcutaneous tissue, and skin is performed. A subfascial drain may be left to reduce hematoma risk.
-
Postoperative Immobilisation & Rehabilitation: Patients wear a rigid cervical collar (or halo vest in select cases) for 8–12 weeks. Early mobilisation with physiotherapy focuses on neck‑strengthening exercises and gradual return to activities.
Benefits of Occipito-Cervical Fusion for Instability
Occipito-cervical fusion effectively restores stability to the craniovertebral junction, preventing further spinal cord damage. By reinforcing this crucial region, patients can regain control over movement and reduce debilitating symptoms.
Key Benefits of Occipito-Cervical Fusion:
-
Restoration of Stability and Structural Support: The fusion strengthens the connection between the skull and cervical spine, preventing abnormal movements that could endanger neurological function. This allows for improved posture and balance.
-
Pain Reduction and Improved Quality of Life: Instability in the upper spine often leads to persistent pain. Stabilising the affected region alleviates discomfort and enables a return to daily activities.
-
Prevention of Neurological Deterioration: Uncontrolled movement at the craniovertebral junction can compress the spinal cord, causing progressive neurological decline. Fusion prevents further damage, safeguarding nerve function.
-
Enhanced Functionality and Postural Control: The procedure restores cervical spine alignment and strength, improving mobility, reducing fatigue, and enhancing head control.
Will I Need Any Pre-Procedure Investigations?
Occipito-cervical fusion requires thorough preparation to ensure a smooth surgical experience and optimal recovery. Before the procedure, a comprehensive evaluation assesses your overall health, spinal stability, and potential risk factors. Preoperative planning involves imaging tests, medication adjustments, and lifestyle modifications to enhance surgical success. You will receive detailed guidance on what to expect during your hospital stay and post-surgical care. Understanding these steps helps you approach the procedure confidently, ensuring your body is optimally prepared for surgery and recovery.
Comprehensive Medical Assessment
A detailed medical evaluation identifies pre-existing conditions that may affect surgery or recovery. Your healthcare team will assess your medical history, neurological function, and current medications. Laboratory tests, including blood work and coagulation profiles, help detect underlying conditions that may impact healing. If you have cardiovascular disease, diabetes, or other chronic illnesses, additional precautions minimise surgical risks. This assessment ensures you are physically prepared for the procedure and helps tailor the surgical plan to your specific needs.
Preoperative Imaging and Diagnostic Tests
High-resolution imaging plays a critical role in planning occipito-cervical fusion. X-rays, CT scans, and MRI scans provide detailed insights into spinal alignment, bone integrity, and potential nerve compression. These diagnostic tools help determine areas requiring stabilisation and guide implant placement. In cases involving tumours or infections, advanced imaging assesses disease extent and plans effective intervention. Accurate preoperative imaging is crucial for optimal surgical outcomes and reduced complications.
Medication and Lifestyle Adjustments Before Surgery
Certain medications can interfere with surgical success, so preoperative adjustments are necessary. Blood thinners, nonsteroidal anti-inflammatory drugs (NSAIDs), and certain supplements may need to be discontinued to reduce bleeding risks. If you have hypertension or diabetes, medication regimens may be adjusted to maintain stability. Lifestyle modifications, including smoking cessation and improved nutrition, enhance bone healing and recovery. Your healthcare team will provide specific guidelines on dietary changes and physical activity restrictions to optimise your pre-surgical condition.
Understanding the Hospital Stay and Post-Surgical Care Plan
Being informed about your hospital stay and post-surgical care helps you prepare for recovery. You will be admitted on the day of surgery or the night before, depending on your condition. Postoperatively, you will spend time in a monitored setting to ensure stability. Pain management strategies, mobility restrictions, and physical therapy plans will be discussed in advance. Understanding what to expect allows you to make necessary arrangements and set realistic expectations for healing.
What Happens During the Procedure?
Occipito-cervical fusion is a meticulously planned surgical procedure that stabilises the upper cervical spine using specialised fixation techniques. The goal is to restrict excessive movement, promote natural bone fusion, and ensure long-term spinal support.
Surgical Approach and Techniques
The surgical approach is carefully chosen based on the severity and location of instability. A posterior approach is commonly used, with an incision at the back of the neck to access the craniovertebral junction. The affected area is then stabilised using titanium implants, which provide immediate structural support. Intraoperative neuromonitoring ensures spinal cord safety throughout the procedure.
Types of Implants Used (Plates, Screws, Rods)
To secure the occipito-cervical junction, specialized implants such as plates, screws, and rods are utilized. Occipital plates anchor the skull, while cervical screws are placed in the vertebrae to enhance fixation. Rods connect these implants, ensuring rigid stabilisation and allowing for optimal bone fusion over time. The choice of implants depends on the extent of instability and specific anatomical considerations.
Role of Bone Grafting and Spinal Fusion
Bone grafting plays a crucial role in achieving long-term fusion. Autografts (bone from your own body) or allografts (donor bone) are placed at the fusion site to promote new bone growth. Over time, this graft integrates with existing bone, creating a strong permanent connection. Synthetic bone substitutes or biological agents may help speed up the fusion process. This ensures that your spine remains stable after the implants do their job.
The Procedure: Step-by-Step
Occipito-cervical fusion follows a structured approach to ensure precision and safety. The procedure involves stabilising the craniovertebral junction using implants and bone grafts, preventing excessive movement that could compromise neurological function. A well-executed surgical plan minimises risks and optimises long-term spinal stability.
Administration of Anaesthesia and Patient Positioning
General anaesthesia ensures you remain unconscious and pain-free throughout the procedure. Once anaesthetised, you are positioned carefully to provide optimal surgical access while protecting spinal alignment. Depending on the approach, a prone or supine position may be used. Specialised headrests and support devices prevent unintended movement during surgery. Proper positioning is critical for minimising complications and ensuring precise implant placement.
Surgical Exposure and Stabilisation of the Craniovertebral Junction
A midline incision is made at the back of your neck to access the occipito-cervical region. Soft tissues and muscles are gently retracted to expose the bony structures requiring fusion. If spinal cord compression is present, decompression may be performed before stabilisation. The surgeon prepares the vertebral surfaces to enhance fusion and ensure secure implant fit. Meticulous technique at this stage is essential for a successful outcome.
Implant Placement and Spinal Fusion Techniques
Titanium screws are inserted into the occiput and cervical vertebrae to anchor the fusion construct. Connecting rods or plates provide additional stabilisation, restricting unwanted movement. Bone graft material from your own body (autograft) or a donor (allograft) is placed at the fusion site to promote new bone growth. Synthetic bone substitutes or biologic enhancers may accelerate fusion. This step is crucial for achieving long-term spinal stability and preventing future complications.
Closure and Post-Surgical Care
Once the implants and bone grafts are securely positioned, the surgical site is carefully closed in layers to promote healing. Sutures or staples seal the incision. A sterile dressing protects the area. Postoperatively, you will be monitored to assess neurological function, pain levels, and overall stability. Early mobilisation strategies are initiated under medical supervision to facilitate healing and reduce post-surgical complications.
How long does it take to recover from the surgery?
Recovery from occipito-cervical fusion is a gradual process requiring careful monitoring and rehabilitation. While initial healing occurs in the hospital, long-term recovery involves physical therapy, pain management, and functional rehabilitation. Understanding each recovery stage helps set realistic expectations and encourages active participation in your healing journey.
Hospital Stay and Immediate Post-Surgical Care
After surgery, you will be closely monitored in a post-anaesthesia care unit (PACU) before transfer to a specialised recovery ward. Regular neurological assessments ensure intact spinal cord function. Pain management strategies, including intravenous medications, keep you comfortable. A cervical brace may provide additional support during initial healing. Hospital discharge typically occurs within a few days once stability and mobility goals are met.
Pain Management and Rehabilitation
Post-surgical pain is managed through analgesics and muscle relaxants. As healing progresses, strong pain relievers are gradually reduced. Rehabilitation begins with gentle range-of-motion exercises and breathing techniques to prevent complications. A structured pain management plan ensures comfort while promoting mobility and recovery.
Physical Therapy and Long-Term Recovery Milestones
Physical therapy strengthens muscles, improves posture, and restores functionality. Initial activities focus on essential mobility and preventing stiffness. As healing advances, rehabilitation includes strength training, balance exercises, and gradual return to daily activities. Complete recovery may take several months, but adherence to physical therapy enhances long-term success.
Expected Outcomes and Functional Improvements
Occipito-cervical fusion significantly improves stability, reduces pain, and enhances quality of life. Many individuals experience restored mobility and reduced neurological symptoms. While some movement restrictions may persist, the primary goal is to prevent further spinal damage and maintain overall health. Long-term follow-ups ensure continued success and monitor spinal fusion progress.
How Do I Know If I Am Eligible for Occipito‑Cervical Fusion?
You may be considered for occipito‑cervical fusion if your symptoms, imaging and clinical history indicate instability or neurological compromise at the craniocervical junction that cannot be managed conservatively.
You're likely a candidate if:
-
Documented Instability at the Occiput–C1 or C1–C2 Junction: Dynamic flexion–extension radiographs or CT demonstrate excessive motion (>2 mm translation or >10° angulation) between the occiput and atlas or atlas and axis.
-
Neurological Deficits from Compression or Instability: Signs such as myelopathy (gait disturbance, hand dexterity loss, hyperreflexia), lower cranial nerve palsies, or persistent pain attributed to atlanto‑occipital or atlanto‑axial instability.
-
Rheumatoid or Inflammatory Arthropathy: Rheumatoid involvement of the atlanto‑axial joints causes pannus formation, odontoid erosion, or subluxation with risk of cord injury.
-
Traumatic Ligamentous Injury or Fracture: High‑grade occipital condyle, atlas, or axis fractures, or ligamentous disruption (e.g., transverse ligament tear) leading to craniocervical instability.
-
Congenital or Syndromic Anomalies: Conditions such as Down's syndrome, os odontoideum or basilar invagination where anatomical abnormality predisposes to instability and neural compression.
-
Failure of Conservative Management: Persistent pain or neurological symptoms despite bracing, immobilisation, and physiotherapy over an appropriate trial period.
-
Good Overall Health and Surgical Fitness: Sufficient cardiopulmonary reserve and absence of active infection to tolerate a major posterior cervical procedure.
Potential Risks and Limitations of Occipito-Cervical Fusion for Instability
While occipito-cervical fusion is highly effective, it carries certain risks. A thorough preoperative evaluation helps minimise complications and optimise surgical outcomes.
-
Infection Risk - Despite sterile precautions, surgical site infections can occur, requiring antibiotic treatment or additional intervention.
-
Implant-Related Complications - Rarely, hardware failure or loosening may necessitate revision surgery.
-
Nerve Damage - Precision in surgical technique reduces the risk of nerve injury, but neurological monitoring is crucial.
-
Limited Range of Motion - Some head and neck movement restrictions may persist after fusion.
-
Delayed Bone Fusion - Inadequate healing may require additional bone grafting or extended bracing.
Why Choose MIRSS for Occipito-Cervical Fusion for Instability?
At MIRSS, expertise, advanced technology, and patient-centric care define the approach to robotic spinal surgery. Choosing a trusted institution ensures comprehensive, high-quality treatment tailored to your needs.
-
Expert Spine Surgery Team - A team of highly experienced spine care specialists and surgeons, spine anaesthesiologists, and physiotherapists, who collaborate to ensure each surgical outcome is successful at the hospital.
-
State-of-the-Art Technology and Surgical Precision - Advanced imaging, intraoperative monitoring, and robotic-assisted techniques enhance safety and accuracy.
-
Comprehensive Pre- and Post-Surgical Care - From detailed evaluations to long-term rehabilitation, every aspect of your journey is carefully managed.
-
Proven Success in Complex Spinal Surgeries - With a strong track record in spinal stabilization, Manipal Hospitals remains a leader in neurosurgical excellence.
By choosing MIRSS, you receive the highest expertise and compassionate care, ensuring the best possible outcome for your spinal health.