What is Sacroiliac Joint Pathology?
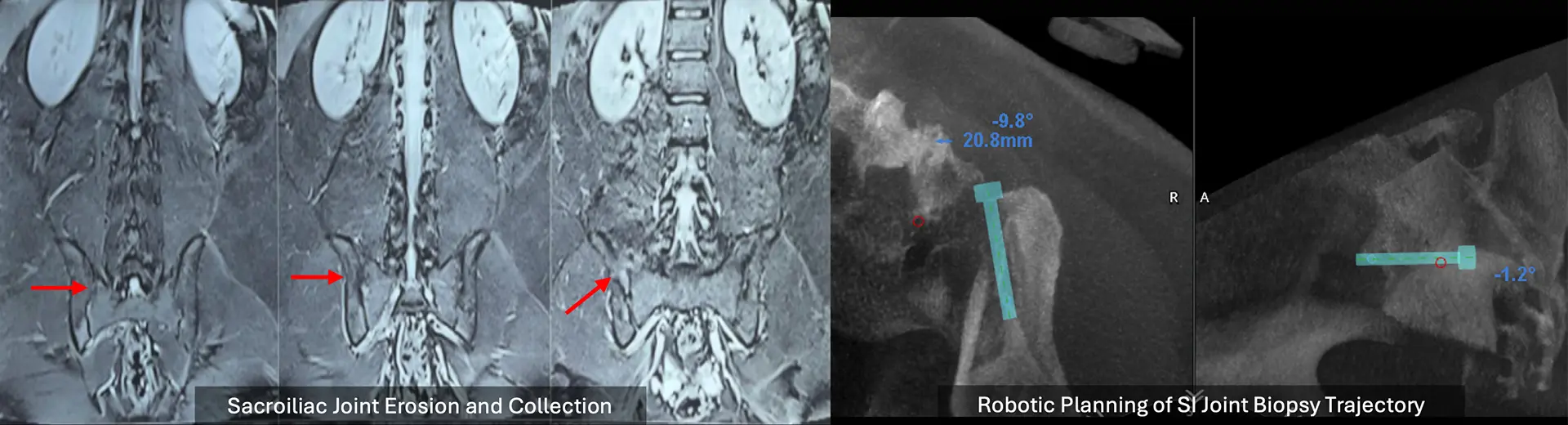
The sacroiliac (SI) joint becomes affected by infection, inflammation, or tumour formation, which is known as sacroiliac joint pathology. Infectious pathologies, such as septic arthritis or tuberculosis, cause joint destruction, severe pain, and mobility problems. People with inflammatory diseases like ankylosing spondylitis or psoriatic arthritis develop chronic pain and stiffness, as these conditions cause permanent fusion between joints over time.
Neoplastic diseases, whether primary or metastatic tumours, cause joint deterioration, resulting in pain and instability. Key indicators include pain in the lower back or buttock region, impaired walking ability, and, in significant cases, neurological problems. Diagnosis relies on medical testing and imaging, while severe conditions may require surgical intervention when medication proves insufficient.
What Is a Closed Sacro-Iliac Joint Biopsy?
A closed sacroiliac joint biopsy enables doctors to collect small tissue samples using minimally invasive techniques. This essential junction between the sacrum and the two iliac bones of the pelvis helps support body weight and maintain stability. The biopsy helps diagnose causes of sacroiliac joint pain and confirms the presence of inflammation or abnormal growths.
During the procedure, fluoroscopy or CT imaging guides a thin biopsy needle into the joint, allowing precise sampling while protecting surrounding tissues. The closed approach offers faster recovery with less discomfort than open biopsy due to its small puncture technique.
The collected tissue samples are sent to medical laboratories, helping doctors make accurate diagnoses and treatment decisions. This minimally invasive diagnostic technique provides reliable results for sacroiliac joint pain, autoimmune disorders, and neoplastic conditions.
What Health Conditions Require Closed Sacro-Iliac Joint Biopsy?
A closed sacro-iliac (SI) joint biopsy obtains tissue or fluid samples from the SI joint under fluoroscopic or CT guidance when imaging and clinical symptoms suggest joint pathology that cannot be confirmed through standard tests.
1. Suspected Infectious Sacroiliitis Tuberculous or bacterial infection of the SI joint may present with persistent buttock pain, fever, elevated inflammatory markers, and joint effusion or bone marrow edema on MRI. A biopsy confirms infection and identifies the causative organism, enabling targeted antimicrobial therapy.
2. Atypical Presentation of Seronegative Spondyloarthropathy In cases of suspected ankylosing spondylitis or other spondyloarthritides with uncertain diagnosis (e.g., seronegative results with atypical imaging), biopsy helps distinguish inflammatory changes from infectious or neoplastic causes.
3. Suspected Neoplastic Infiltration Metastases, lymphoma, or primary tumors involving the sacrum or ilium near the SI joint can mimic infection or inflammatory arthritis. A biopsy differentiates these causes and guides appropriate oncological treatment.
4. Chronic, Unexplained Sacroiliac Pain with Abnormal Imaging If MRI or CT shows focal bone lesions, erosions, sclerosis, or bone marrow signal changes around the SI joint without a clear diagnosis, biopsy provides definitive histopathological insight.
Indications for a Closed Sacro-Iliac Joint Biopsy
Evaluating sacroiliac joint pain may require a closed sacroiliac joint biopsy to clarify an unfamiliar condition. This surgical examination provides important diagnostic information when clinical imaging proves insufficient. Doctors often use this method to evaluate sacroiliitis in patients with autoimmune diseases such as ankylosing spondylitis or psoriatic arthritis. The procedure is valuable for detecting septic sacroiliitis - an infection in the sacroiliac joint.
Delayed infection identification may result in disease progression, causing joint damage or systemic problems. Biopsies are necessary when imaging detects possible masses, tumors, or bony lesions inside the joint, as these require histopathological evaluation to confirm whether they are benign or malignant.
If you have unexplained sacroiliac joint pain, swelling, or stiffness that doesn't improve with standard treatments, or if your physician suspects an inflammatory, infectious, or neoplastic process, a closed sacroiliac joint biopsy can provide critical diagnostic information.
Key Aspects of the Closed Sacro-Iliac Joint Biopsy Procedure
-
Image-Guided Precision: Performed under CT or fluoroscopic guidance to ensure accurate placement of the biopsy needle into the narrow and deep SI joint space.
-
Minimally Invasive Approach: Done through a small skin incision under local anaesthesia with sedation, reducing risk and hospital stay.
-
Safe Anatomical Access: The needle is directed from the posterior or lateral approach to avoid injury to nearby neurovascular structures, particularly the sacral plexus and iliac vessels.
-
Tissue Sample Collection: Core or aspirate samples are obtained for histopathology, microbiology, AFB testing, TB-PCR, and sometimes fungal cultures, depending on the suspected diagnosis.
-
Day-Care Procedure with Minimal Recovery: Most patients can return home the same day with mild activity restrictions and minimal post-procedure discomfort.
-
High Diagnostic Yield: Especially effective in identifying infectious or granulomatous disease, with accuracy improved by real-time imaging and multiple core samples.
Benefits of a Closed Sacro-Iliac Joint Biopsy
Understanding the cause of sacroiliac joint pain or dysfunction is essential for effective treatment. A closed sacroiliac joint biopsy offers multiple advantages as a diagnostic tool.
-
Accurate Diagnosis for Targeted Treatment: A biopsy provides definitive evidence of infections, autoimmune disorders, or tumours, allowing your physician to create a precise treatment plan.
-
Minimally Invasive Approach: Unlike open surgical biopsies, this technique requires only a tiny puncture, reducing trauma to surrounding tissues and lowering complication risks.
-
Faster Recovery and Reduced Downtime: Since no large incisions are made, you can expect minimal post-procedure discomfort and a quicker return to daily activities.
-
Lower Risk of Infection and Complications: Imaging guidance ensures precise needle placement, minimising unnecessary tissue damage and reducing the likelihood of bleeding, infection, or nerve injury.
If you require a biopsy for diagnostic clarification, this minimally invasive approach provides a safer, more efficient alternative to traditional methods.
Will I Need Any Pre-Procedure Investigations?
Proper preparation ensures the success of a closed sacroiliac joint biopsy. Following pre-procedure guidelines minimises risks, enhances accuracy, and promotes smoother recovery. Your physician will provide specific instructions based on your medical history and condition. Key preparation aspects include imaging tests, medication review, dietary restrictions, and counselling about what to expect. These steps improve procedural safety and help you feel informed and confident.
-
Medical Evaluation and Imaging Tests: Before the biopsy, a thorough medical evaluation assesses your overall health and identifies conditions that might affect the procedure. This includes reviewing your symptoms, medical history, and previous treatments. Imaging tests such as X-rays, CT scans, or MRIs pinpoint the exact location of the abnormality, ensuring precise needle placement and reducing the likelihood of inconclusive results. Additional blood tests may be required if inflammatory markers or infections are suspected.
-
Medication Review and Adjustments: Certain medications can affect bleeding risk or interfere with the biopsy. Your physician will review your current prescriptions, including blood thinners, anti-inflammatory drugs, and immunosuppressants. If necessary, adjustments will be made before the procedure. You should disclose all medications, including over-the-counter drugs and supplements, to ensure safety and effectiveness.
-
Fasting and Hydration Recommendations: Depending on the type of anaesthesia or sedation planned, you may need to fast for a specific period before the biopsy. Typically, you'll be asked to avoid food for six to eight hours before the procedure to prevent adverse reactions to sedation. You may be allowed to drink clear fluids up to a few hours before the biopsy. Following these instructions helps ensure a smooth, complication-free procedure.
-
Pre-Procedure Counselling and Preparation: Understanding the biopsy process can ease anxiety and set clear expectations. Your physician will explain the procedure, potential risks, and expected outcomes. This session allows you to ask questions and clarify concerns. You'll receive instructions on what to wear, how to arrange transportation afterwards, and whether additional precautions are necessary. Preparing in advance ensures a seamless experience and promotes stress-free recovery.
How Does a Closed Sacro-Iliac Joint Biopsy Work?
A closed sacroiliac joint biopsy involves carefully guided, needle-based tissue extraction. The procedure relies on imaging assistance to ensure precision, allowing accurate sample collection while minimizing risks.
-
Imaging-Guided Precision: Real-time imaging techniques, such as fluoroscopy or CT scans, guide the biopsy needle. These imaging modalities provide a clear view of the sacroiliac joint's anatomy, ensuring the needle reaches the targeted area without damaging surrounding structures. Fluoroscopy offers continuous X-ray visualisation, while CT scan provides high-resolution cross-sectional images for superior accuracy. This approach minimizes the chances of missing abnormal tissue and enhances diagnostic reliability.
-
Needle Biopsy Technique: Once the biopsy site is identified, a specialized biopsy needle is inserted through a small skin puncture. The needle advances carefully into the sacroiliac joint under imaging guidance. Local anesthesia reduces discomfort, and in some cases, mild sedation ensures a pain-free experience. Unlike an open biopsy, this technique doesn't require large incisions or extensive tissue disruption, making it safer and less invasive.
-
Tissue Sample Collection and Analysis: Once the needle reaches the targeted site, a small tissue sample is extracted using suction or a cutting mechanism. This sample is carefully preserved and sent for laboratory analysis. In cases where infection is suspected, additional fluid samples may be collected for microbiological cultures. The sample adequacy is immediately assessed, ensuring enough tissue is available for accurate diagnosis.
-
Role of Pathology in Diagnosis: A specialist examines the extracted tissue histopathologically. Microscopic analysis identifies abnormal cell structures, inflammatory markers, infectious organisms, or cancerous changes. Additional tests, such as immunohistochemistry or molecular studies, may refine the diagnosis. The final pathology report provides crucial insights that guide treatment decisions, ensuring targeted and effective management.
What Happens During the Procedure?
Step-by-Step Guide
A closed sacroiliac joint biopsy is performed with precision to ensure accurate diagnosis while minimizing discomfort. The procedure involves anesthesia administration, imaging-guided needle insertion, tissue sample extraction, and post-procedure care. Understanding each step helps you feel more prepared and comfortable.
-
Administration of Local or Conscious Sedation: Before the biopsy, local anesthesia numbs the biopsy site, preventing pain during the procedure. In some cases, conscious sedation helps you relax while remaining responsive. The anesthesia choice depends on your medical condition and comfort level. Conscious sedation reduces anxiety, ensuring a calm and controlled experience without requiring general anesthesia.
-
Positioning and Sterilization of the Biopsy Site: Proper positioning ensures accurate needle placement and procedural success. You'll lie face down or on your side, depending on the approach used. The biopsy site is cleaned with an antiseptic solution to eliminate infection risks. A sterile drape maintains a clean environment. Careful skin preparation prevents contamination and ensures a safe biopsy.
-
Imaging-Guided Needle Insertion: Once the biopsy site is sterilized, a specialized biopsy needle is carefully inserted under real-time imaging guidance. Fluoroscopy or CT scan visualizes the needle's path and ensures precise placement within the sacroiliac joint. Imaging guidance significantly reduces complication risks by preventing needle misplacement and unnecessary tissue damage.
-
Tissue Sample Extraction: After the needle reaches the target area, a small tissue sample is collected using suction or a cutting mechanism. This sample is carefully retrieved and preserved for laboratory analysis. For suspected infections, additional fluid samples may be taken for microbial culture. The biopsy needle is removed after securing the sample, ensuring minimal trauma to surrounding tissues.
-
Post-Procedure Dressing and Immediate Care: Following the biopsy, a small dressing is applied to the puncture site. Since the procedure is minimally invasive, sutures are not required. You'll be monitored briefly to check for immediate complications, such as bleeding or discomfort. If sedation was used, you may need a short recovery period before discharge.
How long does it take to recover from the surgery?
Recovering from a closed sacroiliac joint biopsy is generally quick, with most individuals resuming daily activities within a short period. Proper post-procedure care ensures optimal healing and reduces complication risks.
-
Immediate Post-Biopsy Monitoring: After the biopsy, you'll be monitored briefly to assess for immediate side effects, such as dizziness, mild bleeding, or discomfort at the biopsy site. Vital signs are checked, and unusual symptoms are addressed before discharge. If conscious sedation was used, you may need additional recovery time before leaving the hospital.
-
Managing Pain and Discomfort: Mild soreness or discomfort at the biopsy site is common but usually resolves within a few days. Over-the-counter pain relievers or prescribed medications may help manage discomfort. Ice packs can reduce swelling, while avoiding excessive movement prevents irritation at the biopsy site.
-
Resuming Daily Activities: and Mobility Most individuals can return to routine activities within 24 to 48 hours. However, strenuous exercise, heavy lifting, and high-impact movements should be avoided for a few days. Following mobility guidelines prevents unnecessary strain on the biopsy site, promoting faster healing. Your physician will provide specific instructions based on your condition.
-
Follow-Up Care and Next Steps: A follow-up appointment is scheduled to discuss the biopsy results and plan further treatment. If additional tests or interventions are required, they will be outlined during this consultation. Understanding your biopsy results is essential for determining the next steps in managing your condition.
How Do I Know If I Am Eligible for Closed Sacro-Iliac Joint Biopsy?
You may be eligible for a closed SI joint biopsy if you have persistent SI joint pain and imaging or blood tests suggest infection, inflammation, or tumor that cannot be diagnosed with certainty through routine investigations.
You're likely a candidate if:
-
Imaging (MRI/CT) shows suspicious SI joint changes such as joint space widening, erosion, sclerosis, or marrow edema.
-
Blood tests indicate infection or inflammation, such as high ESR, CRP, or leukocytosis, but cultures and serology are inconclusive.
-
You have systemic symptoms such as fever, weight loss, or night sweats in addition to localized pelvic pain.
-
You have a known history of cancer, and imaging suggests sacral or iliac involvement.
-
You are medically fit for a percutaneous procedure under sedation or local anesthesia.
-
You've failed conservative treatment (NSAIDs, physiotherapy, biologics) and need a definitive diagnosis to guide treatment.
Potential Risks and Limitations of a Closed Sacro-Iliac Joint Biopsy
While a closed sacroiliac joint biopsy is safe and effective, it's essential to be aware of potential risks and limitations. Following post-procedure guidelines can significantly reduce these risks.
-
Mild Pain or Soreness: Temporary discomfort at the biopsy site is common but resolves with proper care and medication.
-
Minimal Bleeding or Bruising: Significant bleeding is rare since the procedure is minimally invasive. Applying gentle pressure and keeping the area clean can help.
-
Risk of Infection: Although rare, infection can occur without proper sterilisation. Following hygiene guidelines prevents this risk.
-
Possibility of Inconclusive Results: Sometimes, the sample may not provide definitive answers, requiring repeat testing or alternative diagnostic approaches.
Why Choose MIRSS for Closed Sacro-Iliac Joint Biopsy?
Selecting the right medical centre for a sacroiliac joint biopsy ensures accurate diagnosis and comprehensive care. At MIRSS, you receive expert care backed by advanced technology and a patient-centred approach.
-
Experienced Spine Specialists: The procedure is performed by highly skilled spine care specialists, robotic spine surgeons, spine anaesthesiologists, and physiotherapists with extensive experience in sacroiliac joint evaluations.
-
State-of-the-Art Imaging Technology: Advanced imaging techniques, including high-resolution CT scans and fluoroscopy, ensure precise needle placement and accurate sample collection.
-
Minimally Invasive Approach for Faster Recovery: The closed biopsy technique reduces downtime, allowing you to return to normal activities with minimal discomfort.
-
Comprehensive Post-Procedure Support: From biopsy interpretation to follow-up consultations, a dedicated team ensures you receive the proper treatment based on biopsy findings.
MIRSS remains committed to excellence in musculoskeletal diagnostics, ensuring you receive precise, effective, and compassionate care.