What are Neoplastic or Traumatic Pathologies?
Neoplastic and traumatic pathologies refer to medical conditions caused by tumour formations or tissue injuries. Abnormal cell growth produces benign or malignant tumours that disrupt normal organ function. Malignant tumours can spread to different parts of the body, requiring treatment options including surgery, chemotherapy, or radiation. Physical injuries from accidents, falls, and impacts create traumatic pathologies, resulting in fractures and tissue damage.
Severe trauma can lead to prolonged disability without proper treatment. Diagnosis combines medical imaging and clinical evaluations. Effective management of both conditions requires early diagnosis and specialised treatment to prevent serious complications.
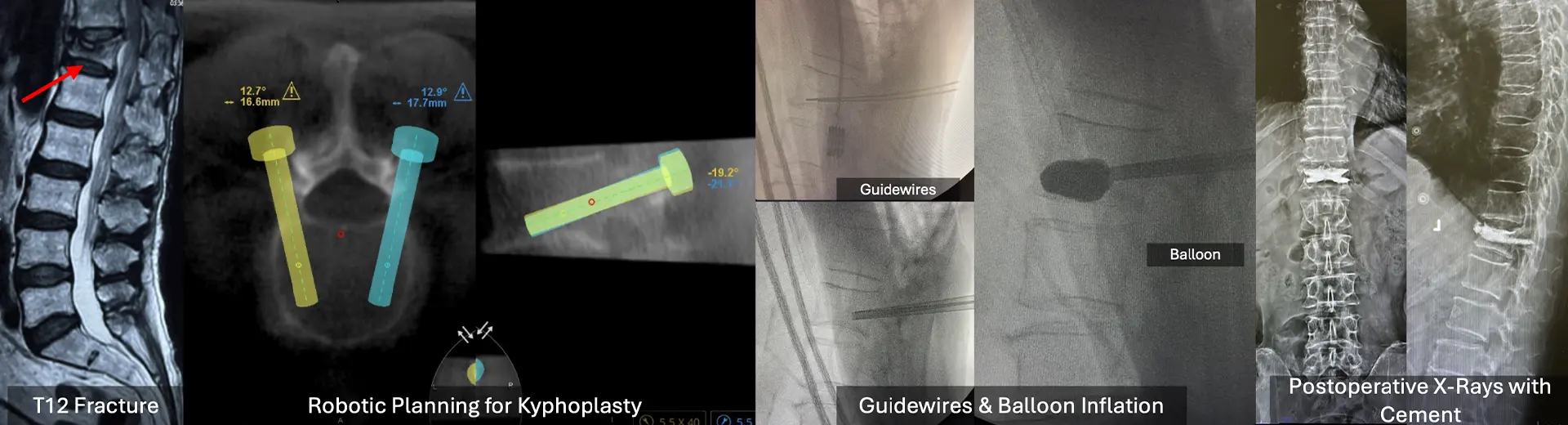
What Is Balloon Kyphoplasty for Neoplastic or Traumatic Pathologies?
Balloon kyphoplasty provides structural support for vertebral fractures caused by neoplastic diseases and traumatic injuries. This procedure is used when standard pain medications and braces are insufficient. A balloon catheter creates a cavity inside fractured vertebrae, allowing precise placement of bone cement to stabilise the structure and relieve pain.
This method effectively strengthens vertebrae weakened by metastases or myeloma disease. The technique restores height to the fractured vertebra while reducing spinal deformities, preventing further kyphosis progression.
Balloon kyphoplasty is ideal for patients with chronic pain and limited mobility who need spine stabilisation due to cancer or trauma. The treatment reinforces the spine with medical-grade bone cement while simultaneously improving quality of life.
Benefits of Balloon Kyphoplasty for Neoplastic or Traumatic Pathologies:
Balloon kyphoplasty offers numerous benefits for treating neoplastic or traumatic vertebral fractures. Unlike traditional surgery, this minimally invasive procedure provides rapid symptom relief while maintaining spinal integrity.
-
Rapid and Effective Pain Relief - The procedure directly addresses the cause of vertebral pain by stabilising the fracture, significantly reducing discomfort within hours.
-
Structural Stability and Spinal Alignment Restoration - Kyphoplasty minimises the risk of spinal deformities such as kyphosis by restoring vertebral height and reinforcing bone strength.
-
Improved Mobility and Functional Independence - Enhanced spinal support allows for more significant movement, reducing dependence on external bracing or assistive devices.
-
Minimally Invasive with Shorter Recovery Time - With only tiny incisions, the procedure minimises surgical trauma and expedites post-operative recovery.
-
Reduced Risk of Further Vertebral Collapse - Bone cement reinforcement reduces the likelihood of recurrent fractures.
-
Improved Quality of Life and Psychological Well-Being – With reduced pain and enhanced mobility, patients experience an overall improvement in daily activities and emotional well-being.
What Health Conditions Require Balloon Kyphoplasty?
Balloon kyphoplasty is considered for vertebral conditions where fracture stabilisation is necessary to prevent further spinal compromise. This procedure is particularly effective when non-surgical treatment fails to provide adequate pain control or structural support.
-
Osteoporotic Vertebral Compression Fractures (VCFs) - While typically managed conservatively, severe osteoporotic fractures causing debilitating pain or progressive deformity can be treated with kyphoplasty.
-
Metastatic Spinal Tumours and Myeloma-Related Fractures - Cancer-related vertebral fractures from primary or secondary tumours weaken bone integrity, requiring kyphoplasty for stabilisation.
-
Spinal Trauma with Vertebral Collapse - High-impact injuries leading to vertebral compression or burst fractures may necessitate surgical intervention to restore spinal alignment.
-
Pathological Fractures Due to Primary Bone Tumours - In cases where primary bone malignancies compromise vertebral stability, balloon kyphoplasty provides structural reinforcement.
-
Post-Surgical Vertebral Instability - Patients experiencing vertebral weakening after previous spinal surgeries may benefit from kyphoplasty to restore support and reduce pain.
Indications for Balloon Kyphoplasty
Patients with unstable spinal fractures that cause significant pain or impair mobility need balloon kyphoplasty. The surgery should be considered only after conservative methods using pain medication and bracing fail to provide appropriate recovery. The procedure is commonly performed on patients with neoplastic spinal fractures that weaken vertebrae or those with tumour-induced bone destruction.
Tumours invading vertebral structures often cause severe pain and functional limitations that require prompt surgical stabilisation in cases of metastatic spinal disease.
Traumatic vertebral compression fractures from high-impact injuries also qualify for balloon kyphoplasty if they cause progressive spinal deformity or persistent discomfort. Patients with osteolytic lesions from primary or secondary malignancies are excellent candidates, as kyphoplasty reinforces fragile vertebrae while reducing pain caused by tumour-induced bone loss.
Additionally, individuals with recurrent fractures or those at risk of adjacent vertebral collapse may benefit from this procedure. The decision for balloon kyphoplasty is based on thorough imaging assessments, ensuring proper patient selection for long-term spinal stability and pain relief.
Key Aspects of the Surgical Procedure:
How Does Balloon Kyphoplasty Work?
Balloon kyphoplasty restores vertebral height and reinforces structural integrity through a controlled, minimally invasive procedure. The process follows precise steps to ensure safe and effective fracture stabilisation.
The procedure uses fluoroscopic guidance for accurate positioning and controlled cement placement. A small incision allows introduction of a balloon catheter into the fractured vertebra. The balloon is carefully inflated, creating a cavity that restores vertebral height while preparing space for cement injection.
Once the desired expansion is achieved, the balloon is deflated and removed, leaving a well-formed cavity for stabilisation. Medical-grade bone cement is injected into the space, solidifying rapidly to reinforce the vertebra. The entire procedure takes approximately 30 to 45 minutes per treated vertebra, with minimal blood loss and reduced surgical trauma.
The Role of Bone Cement in Stabilising Fractured Vertebrae
Bone cement, typically polymethylmethacrylate (PMMA), is a biocompatible material that reinforces the treated vertebra. Once injected, the cement quickly hardens, providing immediate structural support and pain relief. The polymerisation process generates heat, which may have some effect on tumour cells in neoplastic fractures. By filling the cavity created during kyphoplasty, the cement restores vertebral strength, minimizes movement at the fracture site, and prevents further collapse. Proper cement placement is critical, and advanced imaging techniques ensure precise distribution within the vertebral body to optimise outcomes.
Pre-Procedure Guidelines
Preparing for balloon kyphoplasty involves essential steps to ensure a smooth procedure and optimal outcomes. Comprehensive pre-procedure guidelines include diagnostic assessments, medication adjustments, and lifestyle modifications. Following these recommendations minimises potential complications and enhances surgical precision. Your medical team will provide personalised instructions based on your health status, underlying conditions, and specific vertebral pathology.
Diagnostic Imaging and Medical Evaluations
Accurate diagnosis is critical for determining the suitability of balloon kyphoplasty. Advanced imaging techniques such as MRI, CT scans, and X-rays assess the extent of vertebral fractures, tumour involvement, and spinal alignment. Blood tests may be required to evaluate coagulation status and overall health. A thorough medical history review helps identify pre-existing conditions that could affect the procedure.
Medications to Avoid Before the Procedure
Certain medications, such as anticoagulants and nonsteroidal anti-inflammatory drugs (NSAIDs), may increase the risk of bleeding and should be temporarily discontinued under medical supervision. If you are on medications for chronic conditions, your physician will adjust dosages accordingly. Herbal supplements and blood-thinning agents should also be avoided before surgery.
Preoperative Lifestyle Modifications
Maintaining optimal health before the procedure can improve recovery. Smoking cessation is strongly recommended, as nicotine impairs bone healing. A balanced diet rich in calcium and vitamin D supports bone strength. Staying hydrated and engaging in light physical activity can enhance circulation and overall well-being before surgery.
The Procedure: Step-by-Step
Balloon kyphoplasty follows a structured surgical protocol to restore vertebral stability and alleviate pain. Each step is performed under image guidance, ensuring safety and accuracy.
Anaesthesia and Patient Positioning
Depending on your medical condition, the procedure is typically performed under local anaesthesia with sedation or general anaesthesia. You will be positioned face-down on a specialised surgical table to allow optimal access to the affected vertebra. Proper positioning is crucial for ensuring a safe and effective intervention.
Fluoroscopic Guidance and Needle Insertion
A fluoroscopic X-ray system provides real-time imaging to guide needle placement with precision. A small incision and a specialised trocar are inserted into the fractured vertebra through a transpedicular or parapedicular approach. This step ensures accurate access to the affected bone while minimising tissue disruption.
Balloon Inflation to Restore Vertebral Height
A deflated balloon catheter is introduced through the trocar into the vertebral body. Once positioned correctly, the balloon is slowly inflated, creating a controlled cavity within the bone. This process gently restores vertebral height and corrects spinal misalignment caused by the fracture.
Bone Cement Injection and Vertebral Stabilisation
After the balloon is deflated and removed, the cavity is filled with medical-grade bone cement. This biocompatible material quickly hardens, reinforcing the vertebral structure and preventing further collapse. The cement provides immediate stabilisation, reducing pain and restoring spinal integrity.
Closure and Immediate Post-Procedure Monitoring
The incision is closed with a small bandage, and no sutures are required. You will be closely monitored in the recovery unit for vital signs, neurological function, and comfort levels. Most individuals are discharged on the same day, and the medical team provides post-procedure care instructions.
What to Expect After Balloon Kyphoplasty?
Following balloon kyphoplasty, a structured recovery plan is essential for long-term spinal stability and functional improvement. Understanding what to expect and following prescribed guidelines will optimise healing and minimise complications.
Mild soreness at the incision site is normal but typically resolves within a few days. Most patients experience significant pain relief within 24 to 48 hours. Light activities can be resumed within a day, but strenuous physical exertion should be avoided for a few weeks.
Pain Management and Mobility Support
Post-procedure discomfort is minimal and can be managed with prescribed pain relievers if necessary. While you may feel immediate relief, a gradual return to activity is advised. Avoid prolonged sitting or standing in one position, and use ergonomic support to maintain spinal alignment.
Physical Therapy and Follow-Up Care
Physical therapy may be recommended to enhance mobility and strengthen spinal muscles. Follow-up imaging assessments ensure that the cement placement is stable and that there are no complications. Regular bone health evaluations help prevent future fractures and maintain spinal integrity.
Potential Risks and Limitations of Balloon Kyphoplasty
Balloon kyphoplasty is a well-established procedure with a high success rate, but like any surgical intervention, it carries certain risks and considerations. Understanding these factors helps you make an informed decision.
-
Cement Leakage - Although rare, bone cement may extravasate beyond the vertebral body, potentially affecting adjacent structures.
-
Infection - Any surgical procedure carries a minimal risk of infection, which is mitigated by strict aseptic techniques.
-
Adjacent Vertebral Fractures - Strengthening one vertebra may increase stress on neighbouring bones, necessitating ongoing monitoring.
-
Neurological Risks - Though uncommon, improper cement placement or procedural trauma could affect nearby nerves, requiring corrective intervention.
-
Incomplete Pain Relief - While most experience significant pain reduction, underlying conditions such as tumour progression may influence long-term outcomes.
Why Choose MIRSS for Balloon Kyphoplasty for Neoplastic or Traumatic Pathologies?
MIRSS is a leading healthcare facility in India for advanced spinal interventions, offering expertise in minimally invasive procedures like balloon kyphoplasty. Our specialised team ensures precise treatment tailored to individual needs, prioritising safety and effectiveness.
-
Expert Multidisciplinary Team - Our spine surgeons, spine care surgeons, consultants, and anaesthesia team collaborate to deliver the best care.
-
State-of-the-Art Imaging and Surgical Technology - Advanced fluoroscopic guidance ensures precision and minimises procedural risks.
-
Personalised Patient Care and Rehabilitation Support - Our comprehensive approach includes preoperative counselling, post-procedure monitoring, and structured rehabilitation programs.
-
Proven Track Record of Successful Outcomes - Our high success rates and patient satisfaction underscore our commitment to excellence in spinal procedures.
-
Focus on Safety and Comfort - From pre-procedure evaluations to post-surgical recovery, our protocols prioritise safety, comfort, and long-term well-being.