Atlanto-axial instability refers to the abnormal movement or misalignment between the first (C1) and second (C2) cervical vertebrae (bones that make up the spinal column). It is often caused by traumatic or infectious conditions, inflammatory diseases, or neoplastic pathologies. When left untreated, it results in severe pain, neurological deficits and possible spinal cord compression.
Surgical intervention becomes necessary to prevent neurological damage when conservative treatment proves ineffective. The primary objectives of atlanto-axial surgeries involve spinal stabilisation and realignment restoration, with complication prevention. These procedures reduce the risk of spinal cord damage while improving mobility, providing pain reduction and better patient health outcomes.
What is Atlanto-Axial Instability?
C1 (Atlas) and C2 (Axis) vertebrae instability occurs primarily due to weak ligaments or fractures. An unstable spine can damage the spinal cord, causing pain, restricted movement and neurological problems, including weakness and numbness that could progress to complete paralysis in serious cases.
Almost half of the neck's rotational movement occurs through the C1-C2 vertebrae, which play a fundamental role in head stabilisation and rotational capabilities. The special structure enabling high flexibility also makes these vertebrae prone to instability when exposed to trauma or disease. Early diagnosis and appropriate treatment are the primary factors for preventing severe complications.
Causes of Atlanto-Axial Instability
Trauma:
-
High-impact injuries, such as those sustained in car accidents or falls, can fracture the odontoid process (dens) or disrupt the stabilising ligaments of the C1-C2 joint.
-
Ligamentous injuries, particularly to the transverse ligament, can lead to excessive movement and misalignment of the vertebrae.
Infection:
-
Conditions like tuberculosis (Pott's disease) or bacterial infections can erode the bone and ligaments of the atlanto-axial joint, resulting in instability.
-
Chronic infections may cause bone destruction, necessitating surgical stabilisation.
Inflammatory Conditions:
-
Rheumatoid arthritis commonly affects the atlanto-axial joint, leading to ligament weakening, erosion of the odontoid process, and progressive instability.
-
Other autoimmune disorders can also contribute to inflammatory damage in the cervical spine.
Neoplastic Pathologies:
-
Tumours affecting the C1-C2 vertebrae, whether primary (originating in the spine) or metastatic (spreading from other cancers), can weaken the bone structure and cause instability.
-
Surgical intervention may be required to remove the tumour and reconstruct the affected vertebrae for spinal stability.
Atlanto-axial instability significantly affects patients' quality of life, requiring prompt medical assistance. The combination of diagnostic medical imaging and clinical examinations allows physicians to determine the most suitable treatment approach, with surgical stabilisation prioritised for serious cases.
What is Atlanto-Axial Surgery?
Atlanto-axial surgery stabilises both C1 and C2 cervical vertebrae. Surgery becomes necessary when individuals suffer from trauma or develop instability due to infection, inflammatory diseases, or tumours. The main goals include preserving spinal cord function, reducing pain and preventing problematic compression of the spinal cord.
Is Atlanto-Axial Surgery a Major Procedure?
Yes, atlanto-axial surgery is considered a major surgical procedure due to its complexity and critical location near the spinal cord. The procedure typically involves:
-
Surgical Approach - Techniques such as posterior fixation and trans articular screw placement are used to stabilize the C1-C2 vertebrae.
-
Fusion Techniques - Bone grafts and implants may be utilised to promote long-term spinal stability and prevent further complications.
What Conditions are Treated with Atlanto-Axial Surgery at MIRSS?
Atlanto-axial surgery is performed to address various conditions that affect the stability of the C1-C2 vertebrae, including:
-
Trauma-Related Instability - Fractures, dislocations, or ligament injuries leading to spinal instability.
-
Infection-Induced Instability - Conditions like tuberculosis and osteomyelitis weaken the bone structure.
-
Rheumatoid Arthritis and Other Inflammatory Conditions - Chronic inflammation causes joint damage and instability.
-
Tumours or Neoplastic Lesions - Abnormal growths affecting the C1-C2 vertebrae that compromise stability.
Indications for Surgery
-
Traumatic Atlanto-Axial Instability – Severe fractures or dislocations resulting from accidents, falls, or high-impact trauma.
-
Infectious Atlanto-Axial Instability – Conditions such as tuberculosis or bacterial infections causing vertebral destruction and instability.
-
Inflammatory Atlanto-Axial Instability – Autoimmune diseases like rheumatoid arthritis lead to joint erosion and instability.
-
Neoplastic Atlanto-Axial Instability – Tumours affecting the C1-C2 junction, either primary bone tumours or metastatic lesions, compromising structural integrity.
Atlanto-axial surgery plays a critical role in stabilising the cervical spine, alleviating pain, and preventing severe neurological complications. Patients with persistent symptoms or imaging evidence of instability should consult a specialist to determine the necessity of surgery.
Key Aspects of Atlanto‑Axial Surgery for Instability (Trauma, Infection, Inflammation, or Neoplasm)
-
Patient Selection & Preoperative Assessment: High‑resolution CT (for bony anatomy and screw trajectory) and MRI (for cord compression, abscess or tumour extent) are mandatory. Dynamic flexion–extension radiographs confirm instability. Vascular imaging (CT‑angiography) may be required to delineate a high‑riding vertebral artery or anomalous anatomy.
-
Anaesthesia & Neuromonitoring: General anaesthesia with continuous intra‑operative neuromonitoring (somatosensory and motor‑evoked potentials) safeguards spinal‑cord and brainstem function, particularly vital when manipulating the C1–C2 complex.
-
Patient Positioning: Prone on a radiolucent frame, head secured in a Mayfield clamp with slight flexion or neutral alignment. All pressure points are padded, and cervical traction can be applied via Gardner–Wells tongs to aid reduction of subluxation.
-
Posterior Midline Exposure: A midline incision from the occiput to C3 exposes the posterior elements. Subperiosteal dissection of the paraspinal muscles reveals the C1 posterior arch, C2 lamina, and lateral masses.
-
Pathology‑Specific Decompression & Debridement: Trauma: Removal of bone fragments or odontoid remnants. – Infection: Thorough debridement of purulent material and necrotic bone, with irrigation and antibiotic‑laden gel where indicated. – Neoplasm: Excision or curettage of tumour tissue to decompress the cord, often in conjunction with oncological planning.
-
Fixation Techniques: C1 Lateral‑Mass Screws & C2 Pedicle/Pars Screws (Harms/Goel Technique): Offers rigid segmental fixation with a low risk of vertebral‑artery injury. – C1–C2 Transarticular Screws (Magerl Technique): Provides strong biomechanical stability but requires precise reduction and favourable anatomy. – Rods are contoured to the native C1–C2 lordosis and secured to screw heads.
-
Reduction & Alignment: After screw placement, manual or instrument‑assisted compression/distraction across the rods achieves optimal C1–C2 alignment and restores the atlanto‑axial interval.
-
Bone Grafting & Fusion Bed Preparation: Decortication of the C1 posterior arch and C2 lamina creates a fusion bed. Autologous bone (local morselized or iliac crest graft) is placed over the decorticated surfaces to promote arthrodesis.
-
Closure & Drainage: Layered closure of fascia and skin is performed, often with a subfascial drain to prevent haematoma in the tight posterior cervical space.
-
Postoperative Immobilisation & Rehabilitation: A rigid cervical collar (or halo vest in cases of poor bone quality or extensive debridement) is worn for 8–12 weeks. Early mobilisation with physiotherapy focuses on maintaining head‑neck control and preventing deconditioning. Serial radiographs assess fusion and hardware position.
Benefits of the Procedure
-
C1-C2 Joint Stabilisation: By securing the unstable joint, the procedure stops additional movement that might worsen the condition.
-
Relief from Neck Pain and Neurological Symptoms: Patients frequently report reduced pain and improved motor and sensory abilities.
-
Prevention of Spinal Cord Compression: The surgery reduces the risk of spinal cord injury by stabilizing the joint, preventing potential paralysis or other serious consequences.
-
Better Range of Motion and Quality of Life: After surgery, patients typically report improved function and increased daily activities despite some movement restrictions.
Will I Need Any Pre-Procedure Investigations?
-
Imaging Studies: Surgical planning is facilitated by X-rays, MRIs, and CT scans that provide complete cervical spine imaging while assessing structural abnormalities and identifying potential instability. These imaging technologies help detect congenital defects, injuries, ligament damage, and fractures.
-
Neurological Assessment: Medical evaluation of spinal cord conditions requires assessment of muscle strength, nerve function tests, and reflex assessments. Nerve compression evaluation may require electromyography (EMG) and nerve conduction studies. During this phase, doctors ensure treatment specifically targets the prevention of neurological damage.
-
Blood Tests & General Health Evaluation: General health assessment includes essential blood testing with renal function tests, coagulation profiles, and complete blood counts (CBC). These tests allow healthcare professionals to diagnose potential medical conditions that would impact surgical safety and recovery by evaluating for anaemia, coagulation abnormalities, and kidney impairment.
-
Cardiac and Anaesthesia Clearance: A thorough examination of heart function with ECG testing and echocardiography ensures cardiac stability for surgical candidates. The perioperative assessment includes anaesthesia consultation to determine how a patient will tolerate anaesthesia and to detect potential safety concerns.
Explanation of the Surgical Procedure
Achieving stabilization during this surgery requires the application of screws combined with rods and bone grafts. During the procedure:
The immediate mechanical stability comes from placing screws inside the C1 and C2 vertebrae. Structural support is strengthened through rods that connect the screws to perform alignment. Bone grafting enables the long-term fusion of C1 and C2 vertebrae for stability. Additional fixation methods, including plates and interbody spacers, may be used when circumstances require them.
Step-by-Step Breakdown of the Procedure
-
Anaesthesia & Patient Positioning: General anaesthesia maintains patient unconsciousness while blocking pain before surgery begins. Proper positioning prevents complications caused by pressure. Head-holding devices stabilise the skull by maintaining alignment when patients are placed in supine or prone positions for treatment.
-
Incision & Access to C1-C2 Vertebrae: To expose the C1-C2 area, a precise incision is made at the back of the neck. Muscles and soft tissues are carefully retracted to minimise damage to nearby structures and create a clear surgical field.
-
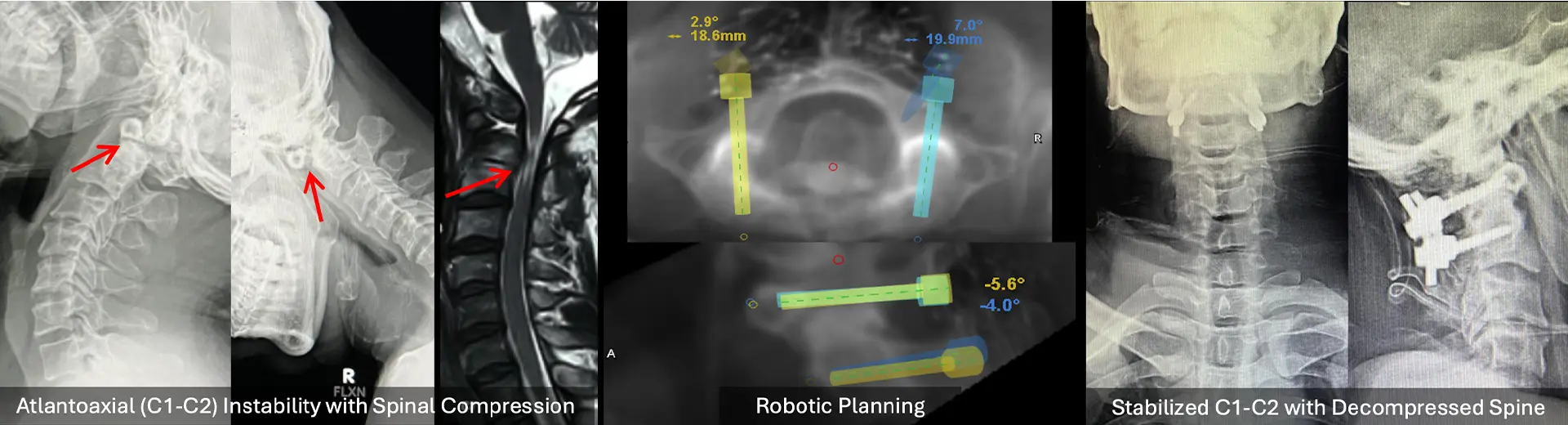
Placement of Screws and Rods: Specialized screws are driven into the pedicles of C2 and the lateral masses of C1 to add stability. Rods are then attached to join the screws, strengthening the vertebrae's alignment. Real-time imaging techniques and robotic assistance guide the placement of these implants to ensure accuracy and avoid complications.
-
Bone Grafting for Fusion: A bone graft is placed between the C1 and C2 vertebrae to promote long-term spinal stability. This graft may be obtained from the patient's own bone (autograft) or from a donor (allograft). Over time, the graft facilitates fusion between the two vertebrae, forming a solid structure.
-
Closure & Post-Operative Care: After the implants and bone graft are securely in place, the incision is carefully closed in layers to promote proper healing. Post-operative care includes pain management, infection prevention strategies, and early physical therapy to aid recovery. The patient is monitored for any signs of complications.
How long does it take to recover from the surgery?
-
Hospital Stay (1-2 Days): Initial recovery involves pain management, infection monitoring, and supervised physiotherapy. Patients are observed for any neurological changes and gradually encouraged to mobilise under guidance.
-
Early Recovery (4-6 Weeks): During this period, patients should avoid strenuous activities and maintain neck support if recommended. Light activities such as walking are encouraged to promote circulation and healing. Follow-up appointments help track progress and detect any early complications.
-
Full Recovery (6-12 Months): Complete vertebral fusion typically takes several months. Through planned rehabilitation, patients gradually regain strength and range of motion. Recovery outcomes depend on healing capacity, compliance with post-operative instructions, and adherence to physical therapy.
In cases of trauma, congenital abnormalities, or degenerative diseases, atlanto-axial surgery is essential for stabilising the cervical spine and preventing further complications. This complex procedure requires precise surgical technique and post-operative rehabilitation. At MIRSS, patients receive advanced care, state-of-the-art surgical methods, and structured recovery plans for optimal outcomes, benefiting from the hospital's expertise in treating complex spinal disorders
How do I know if I Am Eligible for the surgery?
Determining eligibility for atlanto-axial surgery involves a thorough evaluation of various factors, including:
-
Severity of Instability - Radiological assessments, including X-rays and MRIs, help determine the degree of vertebral misalignment.
-
Neurological Symptoms - Presence of weakness, numbness, or signs of spinal cord compression.
-
Pain and Functional Limitations - Assessment of how the condition impacts daily activities, mobility, and overall quality of life.
-
Underlying Health Conditions - Evaluation of bone quality, cardiovascular health, and other medical factors to ensure the patient's fitness for surgery.
At MIRSS, our experts tailor treatment plans to each patient's unique needs, ensuring optimal safety and recovery outcomes.
Potential Risks and Side Effects of Atlanto-Axial Surgery
-
Infection risks and prevention measures: Strict sterile protocols are followed during surgery, and antibiotics may be administered to reduce the risk of infections.
-
Risk of spinal cord or nerve injury: The proximity of the spinal cord makes precision crucial. Surgeons use intraoperative imaging and neuromonitoring to minimise risks.
-
Bleeding and potential clot formation: Blood loss is carefully controlled during surgery, and patients may receive anticoagulants post-operatively to prevent clot formation.
-
Possible loss of neck mobility: Some degree of restriction in neck movement may occur, depending on the extent of fusion and individual healing responses. Physiotherapy can help in optimising post-operative mobility.
Why Choose MIRSS for Atlanto-Axial Surgery?
MIRSS is a leader in advanced spine care, offering cutting-edge treatments for atlanto-axial conditions. Here’s why patients choose us:
-
Expert Multidisciplinary Team: Our team consists of highly experienced spine care specialists, robotic spine surgeons, spine anaesthesiologists, and physiotherapists dedicated to providing world-class care.
-
Advanced Surgical Technology: We utilise real-time intraoperative navigation and robotic-assisted spine surgery to ensure precision and safety.
-
Comprehensive Pre- and Post-Operative Care: Our approach includes personalised rehabilitation programs and advanced imaging techniques for accurate diagnosis and recovery monitoring.
-
Proven Track Record: With high success rates in managing complex atlanto-axial conditions, we provide patients with the best possible outcomes.