What Is Anterior Instrumented Scoliosis Correction?
Anterior instrumented scoliosis correction is a sophisticated surgical treatment approach that accesses the spine from the front of the body (through the chest or abdomen) to treat abnormal spinal curvatures. This method requires surgeons to carefully navigate through anatomical structures to reach the spine and perform direct stabilisation of affected vertebrae (the bones forming the backbone). During this procedure, surgeons install specialized hardware components—including precision-engineered screws, supportive rods, and biological bone grafts—to realign the spine, stabilize affected vertebrae, and promote bone fusion, effectively halting disease progression and preventing further curvature deterioration.
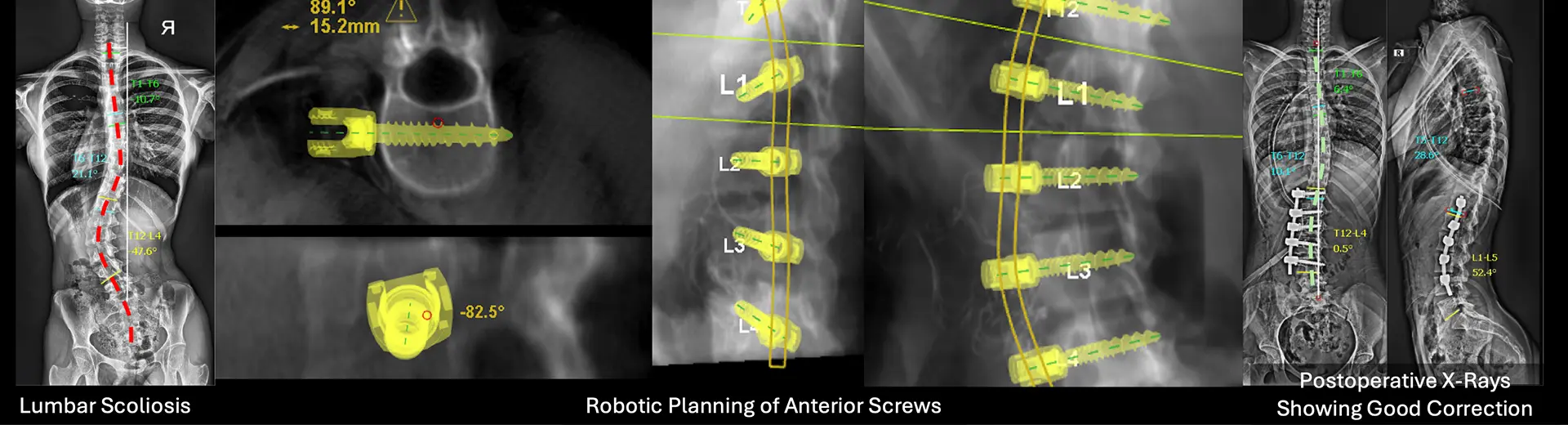
This front-access surgical approach provides excellent control over spinal deformities, making it particularly effective for patients with thoracolumbar and lumbar curves. The primary goals of anterior instrumented scoliosis correction are to rebuild and restore proper spinal balance, significantly improve posture, minimise patient discomfort and pain, and enhance overall quality of life through improved spinal function. Our specialised spine surgeons in Bangalore meticulously plan each surgical intervention based on the curvature severity level, comprehensive patient health status assessment, and age-related considerations to produce optimal outcomes with reduced postoperative complications and issues.
Benefits of Anterior Instrumented Scoliosis Correction
Anterior instrumented scoliosis correction offers several significant advantages over other surgical methods, making it a preferred choice for specific cases where maximum therapeutic benefit can be achieved with minimal invasiveness.
-
Preserved Spinal Motion: One of its primary benefits is the ability to achieve better correction with fewer fused vertebrae, preserving more natural spinal flexibility and mobility. By approaching the spine from the front, surgeons can directly access the affected vertebrae, allowing for more precise realignment and stabilisation with less extensive fusion requirements.
-
Direct Access: The anterior approach provides surgeons with unobstructed, direct visualisation of the affected vertebral segments, enabling more accurate instrumentation placement and deformity correction.
-
Less Tissue Disruption: This technique substantially reduces the need for extensive muscle dissection and disruption compared to traditional posterior approaches, resulting in significantly less postoperative pain and accelerated recovery times for many patients.
-
Enhanced Stability: The anterior method enables superior interbody fusion techniques, enhancing overall spinal stability and substantially improving fusion success rates through optimal graft placement.
-
Improved Cosmetic Results: Since incisions are strategically made on the side of the body rather than directly on the back, resulting scarring is often less noticeable, and the spine maintains a more natural-looking curvature with improved cosmetic outcomes.
-
Effective for Severe Cases: This approach is particularly beneficial for patients with severe or rigid scoliosis, as it allows for more aggressive and comprehensive correction. Furthermore, anterior correction has demonstrably decreased the risk of adjacent segment degeneration, a common long-term complication associated with posterior fusion surgeries.
-
Quicker Recovery: Patients undergoing anterior instrumented scoliosis correction frequently experience shorter hospital stays and quicker return to normal daily activities and functions compared to traditional approaches.
-
Lower Long-term Complication Rates: This method significantly reduces the risks of long-term complications such as hardware failure, implant prominence, or pseudoarthrosis (failed fusion).
Why Is Anterior Instrumented Scoliosis Correction Performed?
Patients require anterior instrumented scoliosis correction to treat serious degenerative spinal curves that fail to respond appropriately to non-surgical approaches such as bracing or physical therapy. Medical experts perform this sophisticated procedure when scoliosis advances beyond certain clinical thresholds, causing:
-
Significantly disrupted standing posture and alignment
-
Substantially compromised breathing capacity and pulmonary function
-
Severely limited movement and mobility restrictions
-
Persistent, chronic pain that affects daily activities and quality of life
Scoliosis patients who receive no treatment will typically develop increasingly serious issues that create noticeable differences in shoulder heights while also causing abnormal rib cage formation and enduring back pain that worsens over time. The abnormal spinal shape frequently creates enough pressure on internal body structures to cause serious respiratory and cardiovascular illnesses that can significantly impact overall health and longevity.
The anterior correction procedure provides spine surgeons with a precise, direct method to stabilise the thoracic and lumbar spine through careful surgical intervention, which entails utilising fewer spinal segments than traditional posterior approaches—an important consideration for maintaining spinal mobility. This procedure is often specifically recommended for younger patients whose bones are still growing and developing, as it allows for better preservation of natural spinal motion while ensuring effective correction of the deformity. It is also particularly beneficial for adult scoliosis cases where previous posterior surgeries may not be viable due to anatomical or technical limitations, or when a more direct approach to the affected vertebrae is needed for optimal correction and stabilisation outcomes.
What Health Conditions Require Anterior Instrumented Scoliosis Correction?
This surgical intervention is primarily used for moderate to severe scoliosis cases where conservative management proves ineffective. Conditions that may require this approach include:
-
Idiopathic Scoliosis: The most common form, typically diagnosed in adolescents, with no identifiable cause
-
Congenital Scoliosis: Spinal deformities present at birth due to vertebral development malformations
-
Neuromuscular Scoliosis: Curvatures caused by conditions like cerebral palsy or muscular dystrophy
-
Degenerative Scoliosis: Age-related spinal curvature and instability in older adults
-
Thoracolumbar and Lumbar Curves: Abnormal curvatures primarily in the lower spine
-
Failed Previous Posterior Surgery: Cases requiring additional stabilisation or revision
Indications for Anterior Instrumented Scoliosis Correction
This procedure is recommended when:
-
Spinal curvature progresses beyond 40–50 degrees, making conservative treatments ineffective
-
The curvature primarily affects the thoracolumbar or lumbar spine
-
Scoliosis causes chronic pain and reduced mobility
-
The curvature compresses organs, causing breathing difficulties or cardiovascular strain
-
Previous posterior spinal correction was unsuccessful
-
The patient is younger and has not reached full skeletal maturity, requiring controlled correction while preserving motion
How Does Anterior Instrumented Scoliosis Correction Work?
The procedure involves accessing the spine through the front of the body via an incision in the chest or abdomen. Surgeons remove intervertebral discs, correct the curvature, and stabilise the spine using specialised instrumentation. Bone grafts are placed to promote new bone growth, ensuring long-term stability.
Pre-Procedure Guidelines
Before surgery, patients must follow specific preparation steps:
-
Comprehensive Imaging: X-rays, MRI scans, and CT scans to assess curvature severity and determine the optimal surgical approach
-
Blood Tests: To identify any underlying health conditions that might affect surgery
-
Pulmonary Function Tests: To evaluate respiratory health, especially important since the procedure involves chest access
-
Medication Review: Certain medications, particularly blood thinners, may need to be temporarily discontinued
-
Fasting Requirements: No food or drink for a specified period before surgery to prevent anaesthesia complications
-
Smoking Cessation: Strongly recommended as smoking can impair bone fusion and delay recovery layers to minimise scarring. A drainage tube may be inserted to prevent fluid buildup.
The patient is then transferred to recovery for close monitoring of vital signs and neurological function.
Recovery and Post-Procedure Guidelines
Recovery after anterior instrumented scoliosis correction is a carefully managed, gradual process that requires diligent post-operative care, structured physical rehabilitation, and regular follow-up evaluations. While most patients experience significant improvements in spinal alignment and mobility, proper healing and long-term success depend on strict adherence to medical guidelines and rehabilitation protocols. This section outlines what patients can realistically expect after the procedure and provides essential post-operative care recommendations for optimal recovery outcomes.
What to Expect After the Procedure
After surgery, the patient is closely monitored in the dedicated recovery room for several hours before being transferred to a hospital room specifically equipped for post-spinal surgery care. Comprehensive pain management strategies, including specialised medication regimens and early physical therapy interventions, are implemented to enhance comfort and begin the rehabilitation process. Some patients may require temporary oxygen support, particularly if the surgical approach involved a thoracotomy, to ensure optimal oxygenation during the initial recovery phase.
Most patients typically stay in the hospital for approximately 4 to 7 days, depending on their individual condition and overall progress with recovery milestones. During this critical hospitalisation period, the medical team continuously assesses spinal alignment, neurological function, and progressive mobility levels. Patients are gradually encouraged to sit, stand, and walk with appropriate assistance, following a carefully designed mobilisation protocol that balances recovery needs with spinal protection.
Follow-up and Further Evaluation
Regular follow-up appointments are crucial to properly monitor the healing process and ensure the spinal fusion progresses correctly according to expected timelines. These structured follow-ups typically include:
-
Comprehensive X-rays and Advanced Imaging Tests: To thoroughly assess spinal alignment stability, and monitor bone fusion progression at regular intervals
-
Specialised Physical Therapy Sessions: Customised rehabilitation programs to systematically restore strength, flexibility, and balance through targeted therapeutic exercises
-
Detailed Activity Restrictions: Patients receive specific guidelines to avoid heavy lifting, strenuous physical activities, and excessive bending or twisting movements for several months post-surgery
-
Structured Long-Term Monitoring: Scoliosis correction patients typically require annual check-ups for several years to ensure continued spinal stability and to address any potential concerns promptly
With proper comprehensive care and dedicated rehabilitation, the vast majority of patients experience substantial improvements in posture, functional mobility, and overall quality of life following anterior instrumented scoliosis correction. This sophisticated surgical approach remains a highly effective treatment option for those with progressive spinal deformities, offering lasting results with minimised long-term complications.
Potential Risks and Limitations of Anterior Instrumented Scoliosis Correction
While anterior instrumented scoliosis correction is generally considered a safe and effective procedure when performed by experienced surgical teams, patients and their families should be aware of certain potential risks and limitations associated with this specialised surgical intervention:
-
Surgical Complications: As with any major operation, there are inherent risks, including potential infection at the surgical site, excessive bleeding during or after the procedure, or adverse reactions to anaesthesia medications.
-
Nerve Damage: There exists a small but significant risk of nerve injury during the operation, which could potentially lead to temporary or permanent weakness, numbness, tingling sensations, or functional loss in certain body areas innervated by the affected nerves.
-
Respiratory Issues: If the surgical approach involves a thoracotomy (chest opening), there is an associated risk of lung deflation or post-operative breathing difficulties that may require extended respiratory support or specialised pulmonary rehabilitation.
-
Bone Fusion Failure: In some cases, the bone graft material may not completely integrate and fuse as expected, potentially resulting in pseudarthrosis (failed fusion) that might necessitate revision surgery to achieve proper stabilisation.
-
Visible Scarring: The anterior surgical approach inherently leaves a visible scar on the chest or abdomen, which may be a cosmetic concern for some patients, particularly adolescents who are often more conscious about body image.
-
Prolonged Recovery Time in Some Patients: While most patients follow an expected recovery timeline, individual healing responses vary considerably, and some patients may require significantly longer periods to regain full mobility and return to normal activities.
Why Choose MIRSS for Anterior Instrumented Scoliosis Correction?
MIRSS is widely renowned for its advanced spine care services and exceptional surgical expertise in complex spinal procedures. Patients considering anterior instrumented scoliosis correction can benefit from our comprehensive approach:
-
Highly Experienced Spine Surgeons: MIRSS houses a distinguished team of skilled spine care consultants and specialized robotic spine surgeons with extensive experience in complex scoliosis deformity corrections and revision procedures.
-
State-of-the-Art Technology: Our facilities utilise cutting-edge diagnostic imaging and sophisticated surgical techniques, including computer-assisted navigation systems, to ensure precise spinal correction with optimal safety profiles.
-
Minimally Invasive Surgical Options: Where clinically appropriate, our surgical teams employ less invasive approaches designed to reduce recovery time, minimise postoperative discomfort, and lower the risk of surgical complications.
-
Comprehensive Pre- and Post-Surgical Care: Patients receive thorough preoperative evaluations, personalised rehabilitation programs tailored to individual needs, and structured long-term follow-up care to ensure optimal outcomes.
-
Multidisciplinary Collaborative Approach: A coordinated team of orthopaedic specialists, neurosurgeons, physiotherapists, pain management experts, and dedicated nursing staff collaborates to provide truly holistic treatment addressing all aspects of patient care.
-
Documented High Success Rates: MIRSS maintains a strong track record of successful scoliosis surgeries with excellent patient outcomes, supported by comprehensive outcome measurements and patient satisfaction metrics.