What Are Herniated Discs?
A herniated disc occurs when the soft, gel-like centre of an intervertebral disc in the spine pushes out through a tear in its tougher outer layer. This displacement can irritate or compress nearby nerves, leading to pain, numbness, or muscle weakness. Herniated discs are most common in the cervical (neck) and lumbar (lower back) regions of the spine, though they can occur elsewhere. The condition can be caused by age-related degeneration, injury, or repetitive strain, and it may contribute to conditions such as sciatica or radiculopathy.
In some cases, when conservative treatments like physical therapy, medication, or lifestyle modifications don't provide sufficient relief, surgical options such as Anterior Cervical Discectomy and Fusion (ACDF) are considered, particularly for herniations in the cervical spine. This procedure involves removing the herniated disc to relieve nerve compression and restore spinal stability.
What is Anterior Cervical Discectomy and Fusion with Interbody Spacer and Plating?
Sometimes, pinched spinal nerves may become swollen and cause arm or neck pain. This pressure can be due to a herniated disc in the neck. ACDF is a preferred treatment when medicine and physical therapy fail to address this problem.
In the empty space of your spinal cord, the surgeon inserts an interbody spacer. This helps in maintaining your spinal alignment. Then, a metal plate is secured with screws to add more stability. This allows proper healing, pain reduction, and restoration of your neck function.
Benefits of the Procedure:
-
Relieves Nerve Compression: It removes the herniated or degenerated disc that's pressing on spinal nerves, reducing neck, shoulder, and arm pain.
-
Restores Spinal Stability: Fusion with an interbody spacer and plate helps stabilise the cervical spine, especially after disc removal.
-
Improves Mobility and Function: Many patients experience better neck function and reduced neurological symptoms like numbness or tingling.
-
Prevents Further Disc Degeneration: Fusing the affected vertebrae can help prevent instability or degeneration at that spinal level.
-
Shorter Recovery Time: Using interbody spacers and plating offers solid structural support, which can speed up healing compared to other fusion techniques.
-
Minimally Visible Scarring: Since the procedure is done through the front of the neck, the incision is small and typically heals with minimal visible scarring.
What Health Conditions Require Anterior Cervical Discectomy and Fusion with Interbody Spacer and Plating?
-
Herniated Disc: A condition where the soft inner part of a spinal disc pushes through a crack in the outer layer, pressing on nearby nerves.
-
Degenerative Disc Disease: Age-related wear and tear of spinal discs that can cause pain, stiffness, or nerve issues.
-
Cervical Spondylosis: Ageing-related changes in the neck vertebrae and discs leading to neck pain and stiffness.
-
Spinal Stenosis: Narrowing of the spinal canal that puts pressure on the spinal cord or nerves.
-
Cervical Radiculopathy: A pinched nerve in the neck that causes pain, numbness, or weakness in the arm or hand.
-
Cervical Myelopathy: Compression of the spinal cord in the neck, causing balance issues, weakness, and coordination problems.
-
Traumatic Spine Injuries: Sudden damage to the spinal cord or vertebrae due to accidents or falls.
-
Cervical Disc Prolapse: The bulging or slipping of a neck disc that can irritate or compress nearby nerves.
-
Osteoarthritis of the Cervical Spine: Breakdown of cartilage in the neck joints leading to pain, swelling, and reduced movement.
-
Fractures or Instability in the Cervical Spine: Breaks or abnormal movement between neck bones that can threaten spinal cord health.
Indications for Anterior Cervical Discectomy and Fusion with Interbody Spacer and Plating
This procedure is recommended for adults with cervical disc pathology or spondylotic disease causing neural compression. When non‑surgical treatments fail to provide relief and neurological function is compromised, ACDF with interbody spacer and plating is indicated. Below are the key clinical indications for considering this advanced cervical spine surgery:
-
Cervical Radiculopathy with Persistent Arm Pain: Radiating arm pain, numbness or motor weakness consistent with nerve‑root compression, unresponsive to conservative measures such as physiotherapy, analgesia or epidural injections.
-
Cervical Myelopathy with Neurological Deficits: Signs of spinal‑cord compression—including gait disturbance, hand dexterity impairment, hyperreflexia or bladder dysfunction—accompanied by MRI evidence of cord compression.
-
Symptomatic Disc Herniation with Neurological Deficit: Acute disc prolapse causing significant motor weakness or sensory loss in the upper limbs, confirmed on imaging and refractory to non‑operative care.
-
Degenerative Cervical Spondylosis with Canal Stenosis: Multiple levels of bone spurs, collapsed disc spaces, and thickened ligaments causing spinal canal narrowing and neurological symptoms.
-
Ossification of the Posterior Longitudinal Ligament (OPLL): Focal or diffuse OPLL resulting in anterior cord compression and progressive myelopathy when conservative measures are ineffective.
-
Segmental Instability or Disc‑Space Collapse: Excessive motion on flexion–extension radiographs or marked loss of disc height causing mechanical neck pain and predisposing to neural compression.
-
Recurrent Cervical Disc Herniation: Symptomatic re‑herniation at a previously operated level requiring repeat decompression and stabilisation.
-
Pathological Conditions Requiring Decompression: Vertebral infection (discitis, osteomyelitis), neoplasm, or trauma leading to anterior‑column compromise and neural‑element compression.
Key Aspects of the Surgical Procedure
Here are the key aspects of Anterior Cervical Discectomy and Fusion (ACDF) with Interbody Spacer and Plating:
-
Anterior Approach: The surgery is performed through the front of the neck to access the cervical spine with minimal disruption to the muscles.
-
Disc Removal: The herniated or damaged disc is carefully removed to relieve pressure on the spinal cord or nerves.
-
Nerve Decompression: The main goal is to relieve nerve compression that causes pain, numbness, or weakness.
-
Interbody Spacer Placement: A spacer (often made of PEEK, titanium, or bone) is inserted into the disc space to restore disc height and alignment.
-
Spinal Fusion: The vertebrae above and below the removed disc are fused together using a bone graft or synthetic material to create long-term spinal stability.
-
Plating for Stability: A small metal plate and screws are often used to secure the fused vertebrae and aid in the healing process.
-
Improved Alignment: Helps correct spinal alignment and maintain the natural curve of the cervical spine.
-
Postoperative Recovery: Patients are often up and moving within a day, with significant relief from nerve-related symptoms.
Will I Need Any Pre-Procedure Investigations?
Your surgeon will examine you physically and ask about your medications and supplements during your initial visit. Imaging tests like MRI and X-ray are needed to identify what's causing your symptoms. Based on these findings, your surgeon will plan your treatment approach.
Your surgeon may give you the following instructions:
-
Prescribe any additional tests, like an electrocardiogram.
-
Consult your primary care physician or cardiologist in some cases.
-
Restrict the use of nicotine and alcohol before the day of your surgery.
-
Not taking blood thinners before the surgery.
-
Make sure someone can drive you home after the surgery.
What Happens During the Procedure?
The procedure includes several steps that generally take 1 to 3 hours.
Preparing the Patient
The surgeon will ask you to lie on your back on the operating table. After giving anaesthesia, your neck area will be cleansed and prepped for surgery. If the surgeon is planning to use your bone for fusion, then your hip area is also prepped. In the case of donor bone, the hip incision is not necessary.
Making An Incision
Your surgeon will make a 1- to 2-inch incision on one side of the front of your neck, usually vertically, after you have gone unconscious. After that, your trachea (breathing tube) and oesophagus (swallowing tube) will be moved aside. The surgeon will lift the muscle that supports the front of the spine to clearly see the bony vertebrae and discs.
Finding the Herniated Disc
After locating the disc with the help of a special X-ray, the surgeon will spread apart the vertebrae bones above and below the herniated disc. To separate them, the surgeon will use a special retractor.
Removing the Disc
Using small grasping tools, the surgeon will remove ⅔ of your disc and any associated bone spurs.
Preparing a Bone Graft Fusion
The surgeon prepares the top and bottom of the disc space by drilling the outer bone layer to expose the blood-rich inner bone. This creates a "bed" for the bone graft material you and your surgeon selected:
-
Transplant of bone from your hip: Over the crest of your hipbone, an incision is created in the skin and muscles. The hard outer layer (cortical bone) is then chipped away with a chisel to reveal the underlying layer (cancellous bone). The inner layer contains proteins and osteogenic cells that promote bone growth. After that, the bone graft is formed and inserted into the "bed" that exists between the vertebrae.
-
Fusion cage or bone bank: The remaining bone shavings, which contain proteins and cells that create new bone, are placed in a bioplastic cage or cadaver bone transplant. The shelf space is then tapped with the graft.
The surgeon can choose an alternate option, including artificial disc replacement. An artificial disc device is placed into the empty disc area in place of a bone graft or fusion cage. Preserving motion may be advantageous for certain patients.
Closing the Incision
They take out the spreader retractors. Together, the skin and muscle incisions are sutured. The incision is covered using biological glue or Steri-Strips.
How Is the Bone Collected from the Donor for ACDF Surgery?
Preparation for the Donor
Sometimes, the surgeon may use donor bone to perform ACDF surgery. The donor bone, or allograft, aids in the appropriate healing and fusion of the spine. Usually, this bone is obtained from a deceased donor who has opted to donate their tissues. Doctors thoroughly examine the donated bone to look for any infections or illnesses. After the examination, they may proceed to clean and sterilise the bone to guarantee its safety for use in surgery. After that, it is kept in a bone bank until surgery is required.
The surgeon chooses a donor bone to prevent more pain for the patient. The donor eliminates the need for an extra cut to remove bone from the patient's body. This approach also allows for less recovery time. Because of the allograft's robust support, the neck's bones can properly merge. This technique promotes quicker healing and less intrusive surgery. The safety and efficacy of donor bone for spinal fusion can be guaranteed for patients receiving it.
How Is the Bone Collected from the Donor?
Spine surgeons follow strict medical protocols to obtain bone from the donor. The examination is then performed on this bone to make sure it is healthy and appropriate for transplantation. Doctors usually extract the bone from the ribs, hip, or leg.
After examination, doctors sterilise the bone to get rid of any bacteria and illness. After that, it is kept in a bone bank until surgery is required.
How long does it take to recover from an ACDF surgery?
For the ACDF surgery, the recovery period differs from patient to patient. Usually, it may take six months to a year to heal the fused bone in your neck.
The surgeon will advise you on self-care and activities to engage in while you're healing. You can engage in mild daily activities but refrain from anything physically demanding. To strengthen your neck muscles, your surgeon could suggest physical therapy. For faster healing, your physical therapist will ask you to add some exercises to your routine. However, he may restrict you from doing some activities:
Restrictions
-
Avoid bending or twisting your neck and lifting anything heavier.
-
No strenuous activity that can increase pressure on your neck and back area.
-
Avoid smoking or using nicotine products. Nicotine prevents new bone growth and may cause your fusion to fail.
-
Don't drive until after your follow-up visit.
-
Drinking alcohol can thin the blood and increase the risk of bleeding.
How do I know if I Am Eligible for ACDF surgery?
If non-surgical treatment options fail, the doctor may recommend you for an ACDF surgery. You may experience the following symptoms:
-
Pain going down your arms.
-
Weakness and numbness in your hands and arms.
-
Trouble with balance and walking.
-
Severe neck pain.
Nonsurgical treatment options could include:
-
Physical therapy.
-
Over-the-counter medications.
-
Injections (epidural steroid injections).
Risks or Side Effects of ACDF Surgery
Side effects are common for any kind of surgery. You may experience some side effects after your ACDF surgery. To help you heal, your surgical team will take precautions against them. Some of the side effects of ACDF surgery are:
-
Difficulty Swallowing: This is a common temporary side effect after surgery.
-
Hoarseness: Voice changes can occur if the surgery affects the nerves that control the vocal cords. It may take several months to resolve.
-
Bleeding, Infection, Blood Clots, or Nerve damage (arm weakness, change in voice, or difficulty holding your eyelid up)
-
Failure of Vertebrae to Fuse: There are numerous explanations for why bones do not unite. Obesity, malnutrition, smoking, and osteoporosis are common ones.
-
Bone Graft Movement: Rarely, 1–2% of the time, shortly after surgery, the bone graft may shift from its proper location between the vertebrae. This is more likely to happen if many vertebral levels are fused or if hardware (plates and screws) is not used. A second surgery may be needed if this happens.
Why Choose MIRSS for ACDF Surgery?
Choosing the right medical centre for spinal surgery is crucial for achieving the best outcome. MIRSS offers world-class expertise, cutting-edge technology, and comprehensive post-surgical care to ensure a safe and successful recovery. If you are in search of the best spine surgery hospital in Bangalore, choose MIRSS for these reasons.
1. Expert Multidisciplinary Team
-
Highly experienced spine surgeons, spine care specialists, anaesthesiologists, and physiotherapists collaborate for successful outcomes.
-
Extensive experience in complex spinal deformity correction.
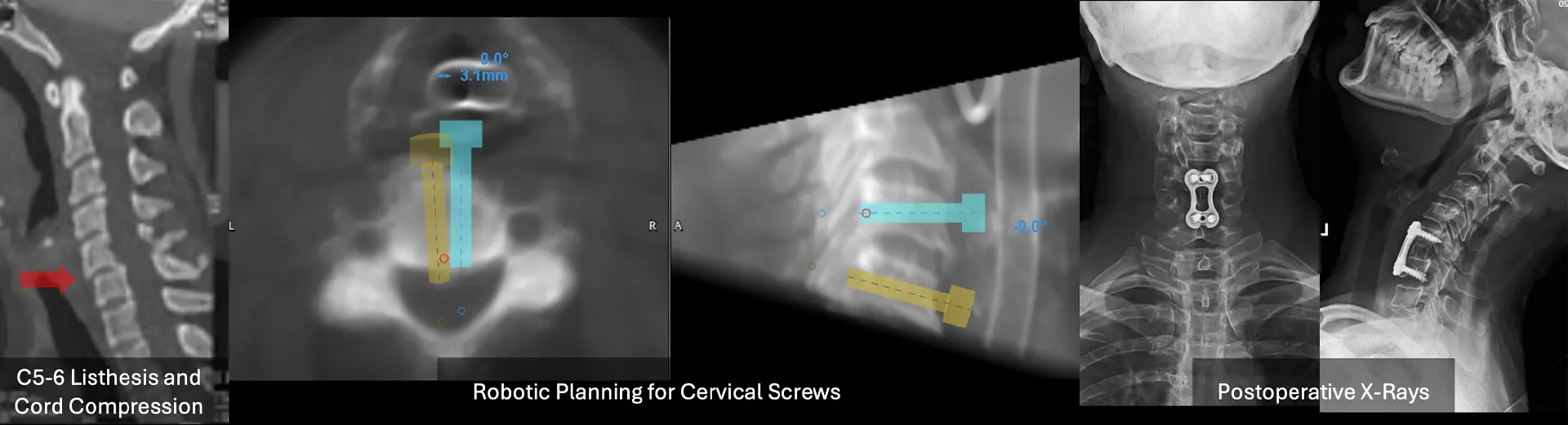
2. Cutting-Edge Surgical Technology
-
Intraoperative navigation systems for precise screw placement.
-
3D imaging and robotic-assisted surgery for enhanced surgical accuracy.
-
Neuro-monitoring technology to prevent neurological complications.
3. Comprehensive Pre- and Post-Operative Care
-
Pre-surgery evaluations, including X-rays, MRI scans, and physical assessments, ensure a well-prepared surgical approach.
-
Personalised rehabilitation programs involving physiotherapy and mobility training accelerate recovery.
4. Proven Track Record
-
Successfully treated numerous adult degenerative scoliosis cases, improving both function and aesthetics.
-
High success rates and patient testimonials highlight excellence in spinal corrective surgeries.