What is Anterior Cervical Corpectomy and Fusion?
Anterior cervical corpectomy and fusion (ACCF) is a surgery that removes vertebral bone and intervertebral disc material (decompression) in the cervical spine. It is recommended for patients suffering from severe pain due to pressure on their spinal cord and nerves. The procedure involves removing damaged vertebrae and discs and replacing them with a special expandable cage. This cage provides better spinal support and stability. For additional support, surgeons typically add a metal plate.
What is an Anterior Cervical Corpectomy and Fusion with Expandable Cage and Plating? When is it recommended?
Anterior Cervical Corpectomy and Fusion addresses cervical spine issues to relieve pressure on the spinal cord and nerves. Surgeons choose corpectomy when discectomy is insufficient. Corpectomy is not necessarily a second-line procedure after a failed discectomy. Rather, it is preferred for cases involving multilevel compression, severe spinal stenosis, or vertebral body pathology (like tumours or fractures). Corpectomy is typically chosen over discectomy to effectively decompress the spinal cord and injured nerve roots. While discectomy removes parts of a disc and some bone spurs, corpectomy removes the entire damaged vertebral body and discs.
To manage your pain, your surgeon may first suggest non-surgical methods like medication and physical therapy. When these options fail, ACCF surgery may be recommended.
ACCF surgery is typically recommended for patients with trauma, tumours, or deformities affecting the vertebrae. In such cases, ACCF surgery ensures better treatment.
Non-surgical methods for treating spinal cord compression often prove more effective with fewer risks. When these non-operative approaches fail to relieve pain, your surgeon may recommend ACCF surgery.
The ACCF surgery is recommended if you are experiencing:
-
Numbness or weakness in your legs and arms, usually caused by a progressive neurologic deficit
-
Loss of bladder and/or bowel control
-
Difficulty walking
-
Impairment of hand coordination, including tying shoelaces and buttoning your shirt
Is Anterior Cervical Corpectomy and Fusion a surgical procedure?
Several factors, including spinal stenosis, tumours, or fractures, can cause pressure on your spinal cord, resulting in severe pain. Doctors typically recommend Anterior Cervical Corpectomy and Fusion surgery when non-surgical treatments are ineffective. The procedure aims to reduce pressure on the nerves and spinal cord.
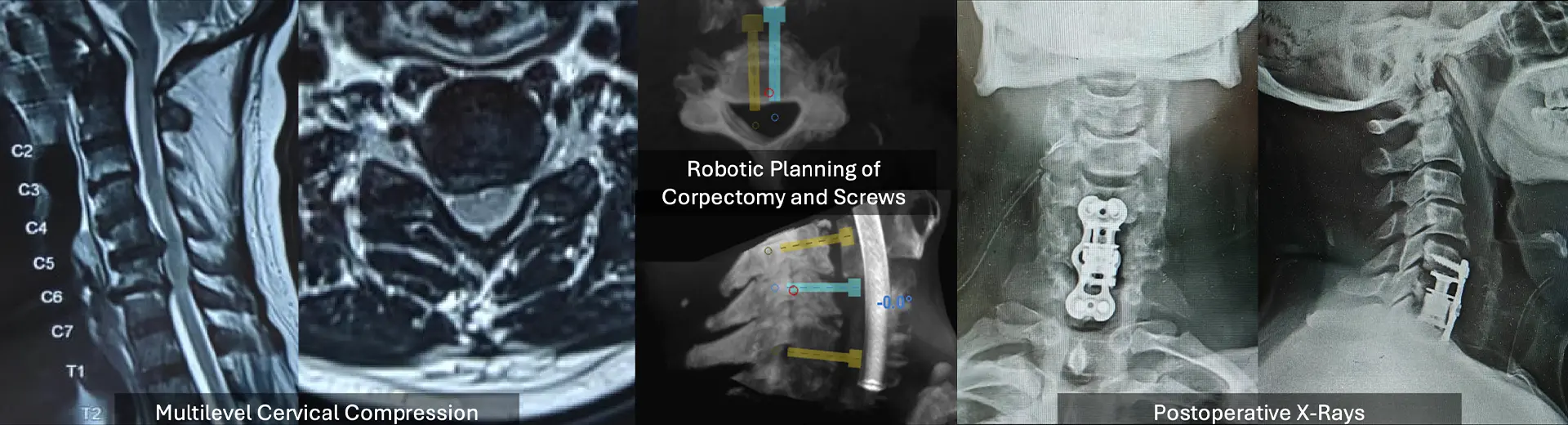
Our robotic spine surgeon begins the surgery by removing the damaged portion of your vertebrae. Doctors typically use a bone graft or implant to replace it and stabilise the spine. A metal plate and screws hold everything in place while your bone heals. This procedure helps relieve pain, restore mobility, and prevent further spinal damage. ACCF surgery is an important treatment option for severe neck and spine issues.
What are the different types of Anterior Cervical Corpectomy and Fusion?
Anterior Cervical Corpectomy and Fusion surgery is performed using different techniques based on the patient's condition and surgical needs. The main types include:
-
ACCF with Expandable Cage and Plating – In this advanced technique, the surgeon places a special expandable cage to replace the removed vertebra, providing better spinal support and stability. For extra reinforcement, a metal plate is added.
-
ACCF with Bone Graft and Plating – Here, the surgeon uses a bone graft to fill the gap, with a metal plate holding the spine in place while the bones heal. Bone grafts may come from the patient or a donor.
-
ACCF with Titanium Mesh Cage (TMC) – This approach uses a strong mesh cage with a bone graft to restore spinal height and support fusion.
For what health conditions is treatment with Anterior Cervical Corpectomy and Fusion available in MIRSS?
When pain medications fail and non-surgical options prove ineffective, surgical intervention may be necessary despite potential risks.
At MIRSS, ACCF surgery is advised for patients with:
-
Intense discomfort is preventing daily activities
-
Arm and leg numbness or weakness due to gradual or significant neurological disability
-
Loss of bladder and/or bowel control from spinal cord compression
-
Walking difficulties due to impaired coordination and balance
-
Inability to coordinate hand movements, such as when tying shoelaces or buttoning shirts
Your surgeon may also recommend ACCF surgery if your spinal cord is significantly affected.
Indications for Anterior Cervical Corpectomy and Fusion with Expandable Cage and Plating
This procedure is recommended for patients with extensive anterior cervical pathology requiring removal of one or more vertebral bodies for adequate decompression and reconstruction. When non-surgical measures fail and neurological function is at risk, anterior cervical corpectomy with expandable cage and plating provides robust decompression, alignment restoration, and stabilisation. Key clinical indications include:
-
Multilevel Cervical Spondylotic Myelopathy: Severe degenerative disc disease with osteophytic encroachment spanning two or more levels, causing spinal-cord compression and myelopathy unresponsive to conservative treatment.
-
Ossification of the Posterior Longitudinal Ligament (OPLL) Across Multiple Levels: Diffuse or segmental OPLL producing rigid anterior compression of the cord, particularly when confined to the anterior column.
-
Vertebral Body Tumours: Primary or metastatic lesions destroying vertebral bodies and compressing the spinal cord, necessitating corpectomy for tumour resection and anterior column reconstruction.
-
Traumatic Cervical Fracture-Dislocations: Unstable burst fractures or fracture-dislocations with retropulsed fragments impinging on the cord, requiring anterior decompression and structural support.
-
Infective Spondylodiscitis with Vertebral Collapse: Tuberculous or pyogenic infection causing vertebral body destruction, kyphotic deformity, and instability, where anterior debridement and reconstruction are essential.
-
Revision after Failed Anterior Cervical Surgery: Pseudarthrosis, cage subsidence, or recurrent compression following prior ACDF, where corpectomy permits removal of failed implants and restoration of alignment.
-
Segmental Instability with Disc-Space Collapse: Excessive motion and loss of disc height at multiple levels leading to mechanical neck pain and neurological deficits, best addressed by vertebral body resection and rigid reconstruction.
Key Aspects of the Surgical Procedure
-
Anaesthesia and Patient Positioning: Performed under general anaesthesia with intra-operative neuromonitoring. The patient lies supine on a radiolucent table, head secured in slight extension to optimise lordosis and fluoroscopic visualisation.
-
Anterior Cervical Exposure: A transverse or oblique skin crease incision is made. The platysma is divided, and the carotid sheath is retracted laterally while the tracheoesophageal complex is mobilised medially to expose the vertebral bodies.
-
Corpectomy Technique: Sequential resection of the targeted vertebral bodies and adjacent discs is carried out using high-speed burrs and rongeurs. Care is taken to protect the dura and neural elements, with thorough removal of pathological tissue.
-
Expandable Cage Insertion: Trial spacers determine the optimal height and lordotic angle. The expandable titanium cage—packed with autograft or bone substitute—is inserted into the corpectomy defect and gradually expanded to restore vertebral height and cervical alignment.
-
Anterior Plating: A pre-contoured cervical plate is affixed to the vertebral bodies above and below the cage using locking screws, providing immediate stability and preventing cage migration.
-
Bone Grafting and Fusion Augmentation: Autologous bone (local morselised bone or iliac crest graft) is packed around the cage and along decorticated endplates to promote arthrodesis and long-term fusion.
-
Wound Closure and Postoperative Care: Layered closure of platysma and skin, with optional drain placement to prevent haematoma. Postoperatively, patients wear a cervical collar as indicated, begin early mobilisation, and follow a structured physiotherapy programme to optimise fusion and functional recovery.
Will I need any Pre-surgery investigations?
Before ACCF surgery with expandable cage and plating, doctors typically request important tests to assess your suitability for the procedure. These results help your surgeon plan the procedure effectively:
-
Blood tests: These check for infections and blood clotting ability, and determine your overall health.
-
Imaging tests: X-rays, CT scans, or MRIs help your surgeon design the procedure.
-
Electrocardiogram: ECG helps physicians evaluate heart function.
-
Pulmonary function tests: These assess whether you have any respiratory disorders.
Inform your doctor about your current medications, as they may need to be adjusted before surgery.
What happens in the Anterior Cervical Corpectomy and Fusion procedure?
ACCF with expandable cage and plating relieves spinal cord and nerve compression in the neck caused by problems with the intervertebral discs.
During this procedure, the surgeon makes a small incision on the front of your neck to access the injured vertebrae. They then carefully remove the damaged intervertebral disc or vertebral body to relieve pressure on the spinal cord and nerves. An expandable cage is inserted to provide support after decompression, with a bone graft placed inside to promote fusion.
Metal plates and screws ensure stability and proper healing. Over time, this arrangement allows the bones to join, restoring strength and functionality. ACCF surgery helps manage pain, improves mobility, and prevents further spinal degeneration.
How long does it take to recover from an Anterior Cervical Corpectomy and Fusion?
Doctors use a patient-centred approach for recovery. After surgery, your surgeon creates a personalised recovery plan to help you recover faster and improve daily functioning. Some symptoms may improve almost immediately after ACCF surgery, while others may take weeks or months to resolve.
Your hospital stay depends on your health and treatment plan. Recovery time is determined by your general health and the degree of spinal damage. Your doctor may advise against activities requiring significant physical strength and may recommend a structured rehabilitation program for faster recovery.
Regular follow-up visits help monitor your healing and address complications. The success of the procedure depends on following your doctor's instructions, your body's response to treatment, and the severity of your condition.
How will the doctor(s) decide if I am an eligible candidate for Anterior Cervical Corpectomy and Fusion?
A spine specialist will carefully evaluate your condition before recommending ACCF surgery. Factors that help determine your eligibility include:
-
Your age and general health, as well as your medical history to assess surgical risks
-
The degree of spinal injury or compression caused by conditions like stenosis, tumours, or fractures
-
Your response to non-surgical therapies, such as physical therapy or medication
-
Your spinal stability and bone quality, which affect successful fusion
-
Your ability to tolerate the surgery and healing process
Are there any risks or side effects of Anterior Cervical Corpectomy and Fusion?
Serious surgeries like ACCF involve certain risks and side effects. Results vary between patients, so carefully consider all risks before making an informed decision. Anaesthesia-related complications are the most common risks in ACCF surgery. Other potential risks include:
-
Infection
-
Blood loss
-
Blood clots
-
Nerve damage
-
Bowel and bladder problems
Fusion failure is the most common complication in spinal fusion, occurring when vertebral bones fail to fuse with the bone graft. Additional surgery may be necessary in such cases.
To minimise complications, follow your physician's instructions carefully and become informed about the ACCF procedure through clinical results and medical information.
Why should I get my Anterior Cervical Corpectomy and Fusion done at MIRSS?
ACCF surgery requires advanced medical infrastructure and skilled surgical teams. At MIRSS, we ensure the best possible care with:
-
Precisely guided spinal operations with 3D imaging, intraoperative navigation systems, and robotic-assisted surgery in state-of-the-art operation theatres
-
A team of highly experienced spine care specialists and robotic spine surgeons, spine anaesthesiologists, and physiotherapists, with years of expertise to handle complex surgeries like ACCF
-
Comprehensive pre- and post-surgical care, right from detailed evaluations to long-term rehabilitation
-
With a strong track record in spinal stabilisation, MIRSS remains a leader in spinal care.
With state-of-the-art equipment and teams of skilled professionals, MIRSS is an excellent choice for your surgery. Our patient-centred approach helps yield the best results for you.