If you’ve ever experienced urine leakage while coughing, sneezing, or exercising, it might be a sign of urinary incontinence. Though common, it’s not something you have to live with. Effective treatments can help you regain comfort and confidence. In this blog, we discuss what it is, the causes and how to seek help.
Synopsis
What is Urinary Incontinence?
Urinary incontinence is the involuntary leakage of urine because of the loss of bladder control. It can occur when the bladder muscles contract suddenly or when the pelvic floor muscles, which also affect the bladder, become weak because of age or other forms of damage. Urinary incontinence can come in different forms; for some, it may be a few drops during coughing or exercise. For others, it can be more frequent or unpredictable and even the discharge of more urine. It can occur in both men and women and can become a cause for embarrassment and silent suffering.
Why Urinary Incontinence Happens
There are many different causes for urinary incontinence. In each case, it can depend on which part of the urinary system is affected. To store and release urine, the bladder, urethra, and pelvic muscles must work together. When any of these become weak, overactive, or damaged, control over holding the urine can be lost. Here are the main types of urinary incontinence and what causes them.
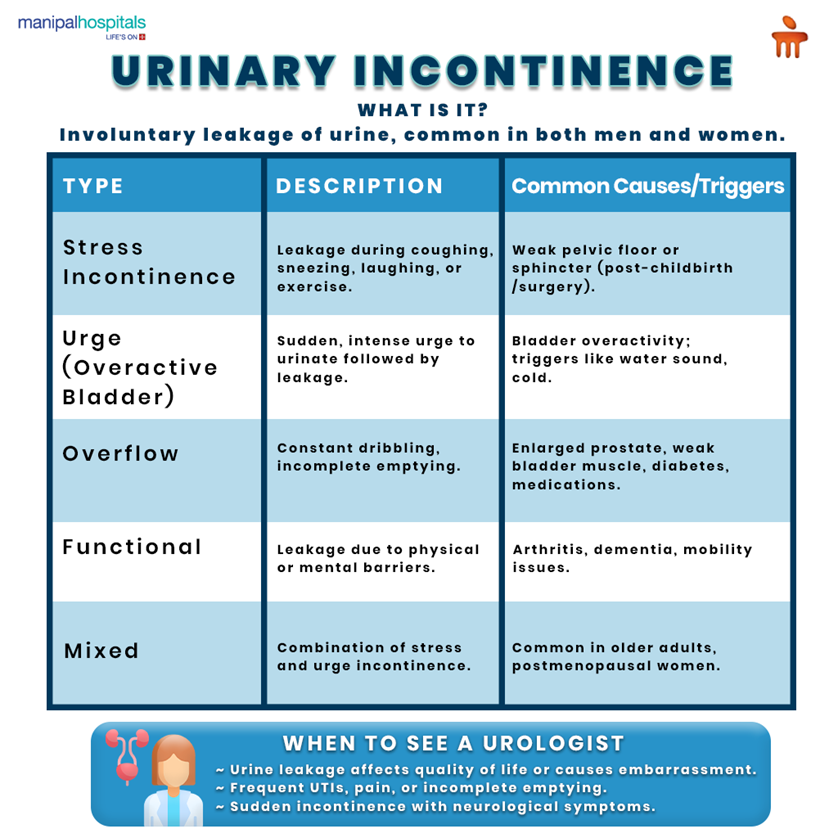
1. Stress Incontinence
This type happens when small amounts of urine leak during coughing, sneezing, laughing, or exercise. When the pelvic floor muscles or the urethral sphincter become weak and cannot hold pressure inside the bladder, it can cause tiny leaks during exertion.
Common causes include:
-
Vaginal childbirth or pelvic surgery that stretches or damages muscles
-
Hormonal changes after menopause
-
Obesity or chronic coughing that increases abdominal pressure
2. Urge Incontinence (Overactive Bladder)
In this case, the bladder muscles contract suddenly without warning. The contraction causes a strong urge to urinate, followed by leakage, and can happen even if the bladder is not full. The condition is usually caused by an overactive bladder, where nerve signals to the bladder misfire. Some people also notice leakage when hearing running water or unlocking their door. It is an indication that the brain and bladder signals have become overly sensitive. Triggers and causes:
-
Nerve-related conditions like Parkinson’s disease, stroke, or multiple sclerosis
-
Urinary tract infections that irritate the bladder
-
Caffeine, alcohol, or cold temperatures
3. Overflow Incontinence
This condition happens when the bladder doesn’t empty fully, which can lead to constant dribbling or small leaks. As a result, the bladder remains overfilled, and pressure builds up until urine escapes. It’s more common in men due to an enlarged prostate, which blocks urine flow, but it can also affect women. Other causes include:
-
Weak bladder muscles from diabetes or spinal cord injury
-
Nerve damage that affects bladder contraction
-
Certain medications that slow urine flow
-
People often feel a weak stream, need to urinate frequently, or wake up often at night.
4. Functional Incontinence
In the case of functional incontinence, the physical or mental barriers prevent a person from reaching the toilet in time. It can also happen if the bladder or the urinary system is healthy. Elderly people or those with mobility or cognitive issues can face this issue. Typical contributing factors:
-
Arthritis or joint pain that slows movement
-
Dementia or confusion
-
Limited access to toilet in a timely manner
5. Mixed Incontinence
Mixed incontinence means a combination of stress and urge incontinence symptoms. The bladder may contract suddenly, and the pelvic muscles may also be too weak to hold urine. It’s often seen in older adults and postmenopausal women. Causes include:
-
Age-related loss of muscle tone
-
Pelvic floor injury or nerve dysfunction
-
Hormonal changes that reduce tissue support
How to Treat Urinary Incontinence?
Treatment for urinary incontinence depends on the type and the cause. For most people, doctors begin with simple steps like lifestyle changes, pelvic floor exercises, and bladder training. If these do not help enough, medications or procedures are added. The goal is to strengthen bladder control and improve quality of life.
1. Lifestyle Modifications
Making small changes in daily habits can help manage leakage and improve bladder control. These are always the first steps in treatment.
-
Reduce intake of bladder irritants like caffeine, alcohol, and spicy foods.
-
Plan timed voiding every 2–4 hours to train the bladder.
-
Maintain a healthy weight to ease pressure on the bladder.
-
Stop smoking, as coughing and nicotine both worsen leakage.
2. Pelvic Floor Exercises (Kegels)
Pelvic floor exercises build strength and control in the muscles that control urination. They are recommended as the main treatment for stress urinary incontinence and mixed types.
-
Kegels involve tightening the muscles you use to stop urinating midstream.
-
A physiotherapist or urologist can guide you using biofeedback techniques.
-
Regular practice can reduce leaks and build long-term control.
3. Medications
Medicines are useful when bladder muscle activity needs control, especially in urge incontinence or an overactive bladder. Different types of drugs are prescribed specifically to the person, depending on their health and other medications.
-
Anticholinergics like oxybutynin and tolterodine relax bladder muscles.
-
Beta-3 agonists such as mirabegron help the bladder hold more urine.
-
Topical vaginal oestrogen improves tissue strength in postmenopausal women.
-
For men, alpha-blockers or 5-alpha-reductase inhibitors treat prostate-related blockage.
4. Bladder Training
Bladder training helps teach the bladder to store urine for longer periods. It is effective for urge and mixed incontinence. Training requires patience, but over time, the bladder learns to respond and is able to hold more urine comfortably.
-
Gradually increase the time between bathroom visits.
-
Avoid rushing when you feel an urge; use relaxation or distraction.
-
Keep a bladder diary to track improvement.
5. Devices and Products
Medical devices can support bladder control when exercises or medication are not enough.
-
Pessaries are small silicone rings inserted into the vagina to support the bladder and urethra.
-
Men may use urethral clamps or temporary inserts to prevent leakage.
-
Absorbent pads or protective garments help manage daily comfort and prevent embarrassment.
6. Advanced Treatments
If symptoms remain despite standard care, doctors may suggest specialised procedures like:
-
Posterior tibial nerve stimulation (PTNS) and sacral neuromodulation help calm an overactive bladder through mild electrical impulses.
-
Botulinum toxin (Botox) injections relax bladder muscles for those who don’t respond to medication.
-
Sling procedures or bulking agents provide support for stress incontinence.
-
In men after prostate surgery, an artificial urinary sphincter can restore control.
When to See a Urologist?
You should see a urologist when urine leakage starts to interfere with daily life or comfort. Ignoring symptoms for too long can delay treatment that could easily help. A specialist can assess the bladder, muscles, and nerves to find out what’s causing the problem and guide the right treatment.Seek medical help if you notice:
-
Leakage that affects your confidence or quality of life
-
Frequent urinary tract infections or burning while passing urine
-
Pain, straining, or difficulty emptying the bladder completely
-
Sudden incontinence after a stroke or spinal injury
-
Persistent symptoms despite basic exercises or medicines
-
Older adults with mixed symptoms or suspected prostate enlargement
Conclusion
Urinary incontinence is completely treatable with the right care. You don’t have to suffer in silence or feel embarrassed about seeking help. With early diagnosis, the cause can be identified and treatment can be started before symptoms worsen. Even simple steps like pelvic floor exercises, bladder training, and medical guidance can bring real improvement in the majority of cases. Hence, it’s important to seek help when you experience any of the conditions we have discussed above.
If you notice frequent leakage, urgency, or difficulty controlling urine, it’s time to speak with a doctor. Visit Manipal Hospital Kanakapura Road to consult a urology specialist and get a clear plan to manage symptoms and regain control over your bladder health.
FAQ's
'Urinary incontinence' is the term used when there is a loss of control over the bladder. It causes you to leak urine when you don’t intend to. It has many factors, such as ageing, or due to medical conditions like diabetes or prostate problems.
There are several forms, and each has its own reason. Stress urinary incontinence happens when pressure on the bladder causes leaks during a cough, sneeze, or exercise. Urge incontinence comes from an overactive bladder that contracts suddenly, creating a strong urge to urinate. Some people have both types together, called mixed incontinence. Knowing which one you have helps your doctor plan the right treatment.
You can start with pelvic floor exercises every day to strengthen the muscles that support the bladder. Cut down on caffeine and alcohol, as they irritate the bladder. Try bladder training by slowly increasing the gap between your bathroom visits. It takes patience, but over time, the bladder learns better control. Even small changes, like maintaining a healthy weight, can make a difference.
If leakage begins to interfere with daily activities or confidence, it’s time to see a urologist. Also, if you’re having pain, repeated urinary infections, or sudden leakage after a stroke or surgery, don’t wait. When simple steps don’t help, a specialist finds the cause and suggests personalised treatments that fit your situation.
For many, it can improve or even stop completely with the right care. Treatments like pelvic floor exercises, bladder training, and medicines work well when started early. Some chronic cases need long-term support, but the condition can be managed effectively.





















 8 Min Read
8 Min Read