Can a sudden, stabbing facial shock, weakening of the hand, or a stubborn low back pain signal a condition that needs specialist care?
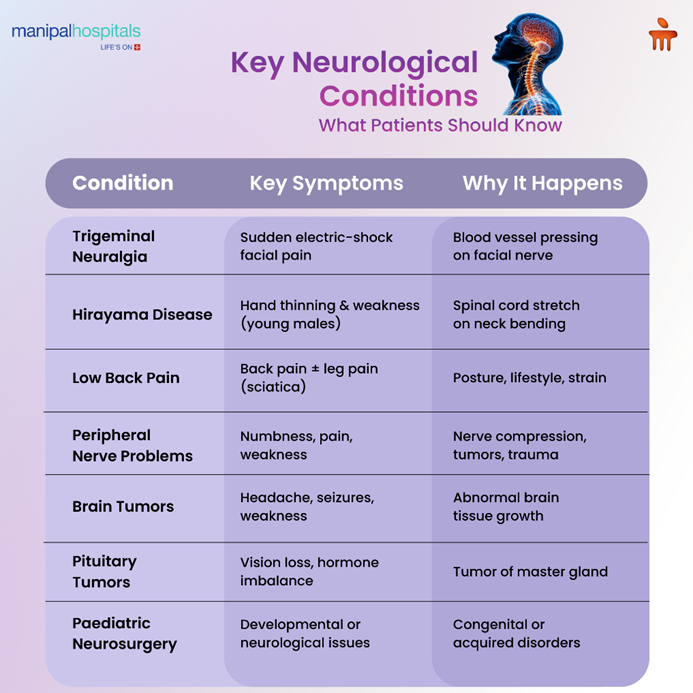
Neurosurgical problems present in many ways, from the electric jolts of trigeminal neuralgia to the progressive hand weakness of Hirayama disease, and from low back pain to complex brain and pituitary tumours. Early recognition, accurate diagnosis, and timely referral make a large difference to outcomes.
This blog highlights key features to watch for, how diagnoses are confirmed, and the realistic expectations for medical and surgical treatment so you and concerned families can make informed choices and plan practical next steps.
Synopsis
Common Neurological Problems
Neurological conditions can make life ‘a living hell’ because they strike at the very core of our ability to move, feel, and interact with the world. While some conditions develop slowly, others appear with a suddenness that is both terrifying and debilitating. Understanding these problems is the first step toward reclaiming your quality of life.
Below are some of the common neurological conditions that require medical and surgical intervention:
Trigeminal Neuralgia: The Zapper
Imagine your face being bombarded by a salvo of sudden, excruciating electric shocks while brushing your teeth, shaving, caressing your face, eating, or even feeling a gentle breeze. This is the reality for people with trigeminal neuralgia (TN), often described as one of the most severe pain conditions known to medicine and infamously called the “suicide disease”!
Trigeminal neuralgia (TN) is a debilitating, chronic pain disorder affecting the major sensory nerve of the face, the trigeminal nerve. When this nerve malfunctions, it sends intense pain signals to the brain.
Clinical features: Attacks are unpredictable, usually lasting a few seconds to 2 minutes, but can recur hundreds of times a day, making daily activities a source of fear and anxiety. The constant fear of the next pain episode can lead to significant physical and emotional anguish, social withdrawal, anxiety, and severe depression, profoundly affecting a person's quality of life.
Cause: The condition is most commonly caused by a blood vessel pressing on the nerve within the skull cavity. In rarer cases, it may be a symptom of multiple sclerosis or a tumour. Though not life-threatening, the relentless pain can be life-altering, leading to social withdrawal and depression.
Treatment:
The good news is that TN is safely treatable. A clinical evaluation by an expert neurologist or neurosurgeon is mandatory. Some patients present to the dentists with tooth pain and have undergone several tooth extractions before realising that they have TN and not dental issues. This incident underscores the importance of proper recognition of symptoms. Usually, a special sequence MRI (CIS3-D) is done to confirm the neural-vessel entanglement and also to rule out any other rare etiologies.
Medications, particularly anticonvulsants like carbamazepine, are typically the first line of treatment and are effective for many. For those who don't find relief with medication or have adverse reactions to it, neurosurgical procedures, such as microvascular decompression, can offer immediate and long-term effective solutions.
If you or a loved one is experiencing unexplained facial pain, it is crucial to consult a neurologist or neurosurgeon for a proper diagnosis and management.
Hirayama Disease: Light at the End of the Tunnel
Hirayama disease, also known as monomelic amyotrophy (MMA), is a rare and not so “benign” neurological disorder that primarily affects young males, typically between the ages of 15 and 25. Characterised by wasting, thinning of hands and forearms, and progressing to weakness and complete nonfunctionality of the hands. While most commonly observed in Asian countries like India and Japan, cases have been reported worldwide.
Clinical features: Weakness of one or both hands is the predominant symptom with no sensory loss (numbness or pain) or lower limb involvement. Symptoms like hand tremors and worsening weakness in cold temperatures are also common.
Aetiology: The exact cause is not known, but theories expound the disproportionate increase in growth of the spinal column during the juvenile growth spurt as compared to the spinal cord, resulting in stretching of the cord, especially while bending, resulting in cord damage and weakness.
Natural course: Hirayama disease progresses relentlessly over several years and later may stabilise, leaving in its wake significant weakness and functional disability of the hands.
Diagnosis:
A high index of awareness and clinical suspicion is key to early diagnosis and favorable outcomes in this disease. Otherwise, these conditions are commonly misdiagnosed as motor neuron disease and other neurodegenerative diseases, which have a bleak outcome. Investigations include nerve conduction studies, electromyography (EMG), and a dynamic MRI of the cervical spine taken in both neutral and flexed positions.
Management:
Once a diagnosis is made, treatment focuses on halting the progression of the disease and managing symptoms:
Surgery: If the symptoms are progressing, then immediate surgical intervention is warranted so as to stop further progression and, in some cases, improve the strength of the hands. It must be emphasised that the main aim of surgery is to halt the progression of the disease. The surgery is safe with a short duration of hospital stay and with a more than 98% success rate.
Historically, the management strategy was that of nihilism and expectant optimism, hoping that the disease would stabilise with a cervical collar and physiotherapy. However, a large number of studies have shown that the above strategies were not effective and are not recommended, especially if the disease is progressing.
Key message: Early diagnosis and surgical intervention is paramount for a good outcome. Surgery stops disease progression but cannot reverse the muscle loss and weakness.
Peripheral Nerve Surgeries
Peripheral nerves serve as conducting media, transmitting information from the nervous system to the muscles and various organs of the body. They play an equally important role in maintaining the neuromuscular harmony. Disruption of these nerves can result in pain, thinning, and muscle weakness. Being neurosurgeons gives us the added advantage of having an in-depth knowledge of the structural and functional aspects of the nerves. This helps us in managing the troubled nerves. Nerve pathologies are clinically diagnosed and supported by investigations like nerve conduction studies, ultrasound, and MRI.
Common Nerve Ailments Managed:
Entrapment neuropathies: At many places in the body, the nerves traverse narrow areas before reaching their targets. Due to wear and tear, trauma, diabetes, hypothyroidism, and obesity, to name a few, these nerves get compressed at the bottlenecks, resulting in numbness, tingling sensations, pain, muscle thinning, and weakness. Common entrapment neuropathies treated include carpal tunnel syndrome, cubital tunnel syndrome, tardy ulnar nerve palsy, posterior interosseous nerve entrapment, Guyon's tunnel entrapment, and tarsal tunnel syndrome. When medical management fails, delicate nerve release (freeing) surgeries are done using intraoperative neuromonitoring and high-end microscopes, which provide a highly magnified, pristine view of the surgical field.
Peripheral nerve tumours: These are not uncommon and arise from within the nerve. Most are benign, but some can be highly malignant. They present as a swelling along with pain and weakness. During the removal of these tumours, utmost care must be taken not to damage the delicate functioning nerve fibres, which will invariably be all around the tumour. If care is not taken, there will be a high risk of neurological deficit after surgery. Using intraoperative monitoring and high magnification microscopes, safe resection of tumours is done with excellent outcomes.
Trauma
Trauma is a major cause of peripheral nerve injury, especially the brachial plexus. This plexus is a network of nerves that supply the muscles of the entire upper limb. Brachial plexus injury usually occurs in young individuals involved in road traffic accidents or falls. It results in partial to complete paralysis of the upper limb. Initially, conservative medical management with optimistic expectation is done for a period of three months. If there is no improvement, then surgical intervention will be required. This includes a variety of nerve surgeries like exploration and neurolysis, grafting, and nerve and muscle transfers, followed by good physiotherapy.
Post-brachial plexus injury pain: Following injury to the brachial plexus, a significant number of patients suffer from varying degrees of pain in the affected limb.
This is managed with medications. However, a small group of patients has excruciating pain recalcitrant to any medication. For them, we perform a surgery called DREZotomy, where we operate on the spinal cord to reduce the transmission of pain impulses being sent to the brain, resulting in a significant reduction of pain.
Neuro-Oncology- Brain Tumours
Headache, seizures, unconsciousness, limb weakness, memory loss, impaired thinking, and judgment all could be features of the rapid growth of abnormal brain tissue within the cranial cavity, also known as brain tumours. It affects all age groups irrespective of race, culture, or gender. There are no known risk factors, though familial transmission and exposure to radiation are seen in a very small group of patients. Use of mobile phones and trauma to the head have not been linked with the occurrence of brain tumours, though there are a number of conflicting studies.
Diagnosis and Treatment:
The neurosurgeon first does a detailed clinical examination, following which neuroimaging is ordered. This includes CT/ MRI plain and contrast with special sequences as and when required.
A fairly accurate diagnosis is then made. Surgery is then planned. The goal of surgery is to achieve maximum, safe resection of the tumour using all the surgical expertise at hand and the latest tech gadgets to accomplish the task.
The excised tissue is then sent for histopathological examination, which takes about a week. Following this, the next step for management is taken. Brain tumours can be benign or malignant.
-
Benign tumours, if fully excised, require no further treatment. They are followed by regular OPD examination and neuroimaging.
-
For malignant tumours, however, radiation therapy and chemotherapy may be required.
Pituitary Tumours: The Malady of the Master Gland
Pituitary tumours, often called a "malady of the master gland," can have significant impacts on the body due to the pituitary gland's crucial role in regulating various hormones. Located at the base of the brain, this tiny gland controls vital functions like growth, metabolism, and reproduction. Most pituitary tumours are noncancerous (benign adenomas) and grow slowly, but their location and potential to secrete excess hormones can still cause serious health issues.
Understanding the Master Gland
The pituitary is also sometimes referred to as the "master gland" because it produces hormones that signal other glands, such as the thyroid, adrenals, and ovaries/testes, to produce their own hormones. When a tumour develops, this delicate system can be disrupted, leading to an over- or underproduction of essential hormones.
Common Types and Symptoms
Pituitary tumours can be broadly categorised into functioning (hormone-producing) and nonfunctioning (non-hormone-producing) types.
Functioning Tumours
These tumours cause symptoms due to the excessive hormones they release.
-
Prolactinomas: The most common type, these cause high levels of prolactin, leading to irregular periods, infertility, and milk production in non-pregnant individuals.
-
Growth hormone-producing tumours: These can cause acromegaly in adults (enlarged hands, feet, and facial features) or gigantism in children.
-
ACTH-producing tumours: These stimulate the adrenal glands to produce excess cortisol, leading to Cushing's disease, which involves weight gain (especially around the midsection and face), high blood pressure, and weakened bones.
-
TSH-producing tumours: While rare, these can cause hyperthyroidism symptoms like weight loss, rapid heartbeat, and anxiety.
Nonfunctioning Tumors
These tumours do not produce excess hormones. Symptoms usually arise from the tumour growing large enough to press on nearby structures, such as the optic nerves, causing headaches and vision problems. In some cases, a large tumour can compress the normal pituitary tissue, leading to a deficiency in one or more hormones, a condition known as hypopituitarism.
Diagnosis and Treatment
Diagnosing a pituitary tumour often involves blood tests to check hormone levels, imaging tests like an MRI of the brain, and a comprehensive eye exam to assess vision.
Treatment approaches vary based on the tumour's type, size, and whether it's functioning. Options include:
-
Observation: For small, nonfunctioning tumours that aren't causing symptoms, doctors may recommend "watchful waiting" with regular monitoring.
-
Medication: Certain medications can shrink specific types of functioning tumours (like prolactinomas) or manage hormone imbalances.
-
Surgery: Transsphenoidal surgery, a minimally invasive procedure performed through the nose, is a common and effective way to remove most pituitary tumours.
-
Radiation Therapy: This may be used to shrink a tumour that cannot be completely removed by surgery or if it grows back after treatment.
Living with a pituitary tumour requires ongoing management and monitoring by a specialised healthcare team, typically including an endocrinologist and a neurosurgeon. For further information and resources, you can consult reputable sources such as the National Institute of Neurological Disorders and Stroke (NINDS) or the Pituitary Network Association.
Paediatric Neurosurgery
Pediatric neurosurgery is a specialised field dedicated to the surgical care of children with conditions affecting the brain, spine, and nervous system. From infancy through adolescence, a child's neurological system is still developing, making their needs vastly different from those of adults. This speciality requires a unique blend of highly advanced surgical skills, an in-depth understanding of developmental neurology, and a compassionate approach to treating children and supporting their families.
As trained pediatric neurosurgeons, we address a wide range of complex conditions. Common procedures involve treating congenital anomalies like spina bifida and tethered spinal cord, hydrocephalus (excess fluid in the brain), and Chiari malformations. We also perform delicate operations to remove brain and spinal cord tumours, manage traumatic head and spine injuries, and treat epilepsy or spasticity that hasn't responded to medication.
The primary goal of this speciality is not just to perform surgery but to ensure the child can develop and thrive to their full potential. Treatment plans are highly individualised and typically involve a multidisciplinary team of pediatric specialists, including oncologists, neurologists, radiologists, and rehabilitation therapists.
This holistic approach ensures comprehensive care that addresses both the medical and developmental needs of the child.
Ultimately, pediatric neurosurgery offers hope and healing to families facing some of life’s most challenging diagnoses. Through innovative techniques and dedicated expertise, we work to improve the quality of life for our young patients, helping them lead healthy, active lives.
Conclusion
Living with neurological symptoms can feel uncertain, especially when pain, weakness, or changes in daily function begin to interfere with routine life. Clear evaluation, the right investigations, and timely treatment help bring structure and confidence to the next steps. For comprehensive diagnosis, evidence-based treatment, and ongoing support, consult the experienced neurosurgeon team at Manipal Hospital Kanakapura Road, where care is planned around safety, clarity, and long-term recovery.
FAQ's
Trigeminal neuralgia causes sudden, electric-shock-like attacks triggered by light touch, chewing, shaving, or a breeze. Tooth pain is usually constant or worsens with biting and does not come in brief stabbing bursts. If dental checks are normal, a neurological review and an MRI with nerve-focused sequences are the next steps.
Look for gradual wasting and weakness of one or both hands in a young person (typically teens to mid-20s) without sensory loss. Symptoms often worsen with a cold and with neck flexion. A dynamic cervical MRI (neutral and flexed) plus EMG helps confirm the diagnosis.
Urgent review is required for sudden bowel or bladder changes, progressive leg weakness, history of cancer, unexplained weight loss, fever, or severe trauma. Most back pain is non-serious and improves with activity, education, and structured exercise, but red flags prompt immediate investigation.
No. Many entrapment neuropathies respond to conservative care—activity modification, splints, physiotherapy, and medical management. Surgery is considered when symptoms persist, progressive weakness appears, or nerve tests and imaging indicate compressive lesions that are unlikely to improve without release.
Diagnosis starts with a neurological exam and targeted imaging (MRI with contrast). Treatment depends on tumour type and location: observation for small nonfunctioning lesions, medical therapy for some hormone-producing pituitary tumours, surgical removal when safe, and radiotherapy or chemotherapy when needed. Multidisciplinary planning ensures the best balance between tumour control and preservation of function.





















 8 Min Read
8 Min Read



.png)