When a stroke happens, the clock starts. Fast recognition and prompt medical care save lives and limit long-term disability. If you or someone you love is at risk, knowing the signs, understanding the types of stroke, and knowing what to do immediately will make the difference between full recovery and lasting impairment. This blog explains what a stroke is, how to spot it quickly using BEFAST, who is at risk, what modern stroke treatment looks like, and how you and your family can work on stroke prevention and stroke recovery after the event.
Synopsis
What is a Stroke?
Stroke is a medical emergency that demands fast recognition and prompt care. A stroke occurs when the blood supply to a part of the brain is blocked, or a blood vessel bursts. Without oxygen-rich blood, brain cells begin to die within minutes. This is what makes stroke a medical emergency. Being one of the leading causes of death and disability worldwide, strokes can strike anyone at any time, be it young or old, men or women.
Types of Stroke
-
An Ischemic Stroke is caused by a blood clot or blockage in the brain’s arteries. This is the most common type (about 80% of all strokes).
-
Hemorrhagic Stroke is caused by bleeding in the brain when a blood vessel breaks.
-
Transient Ischemic Attack (TIA) is often called a “mini-stroke”. Symptoms go away in minutes or hours, but it’s a serious warning sign for future strokes.
Signs & Symptoms of Stroke
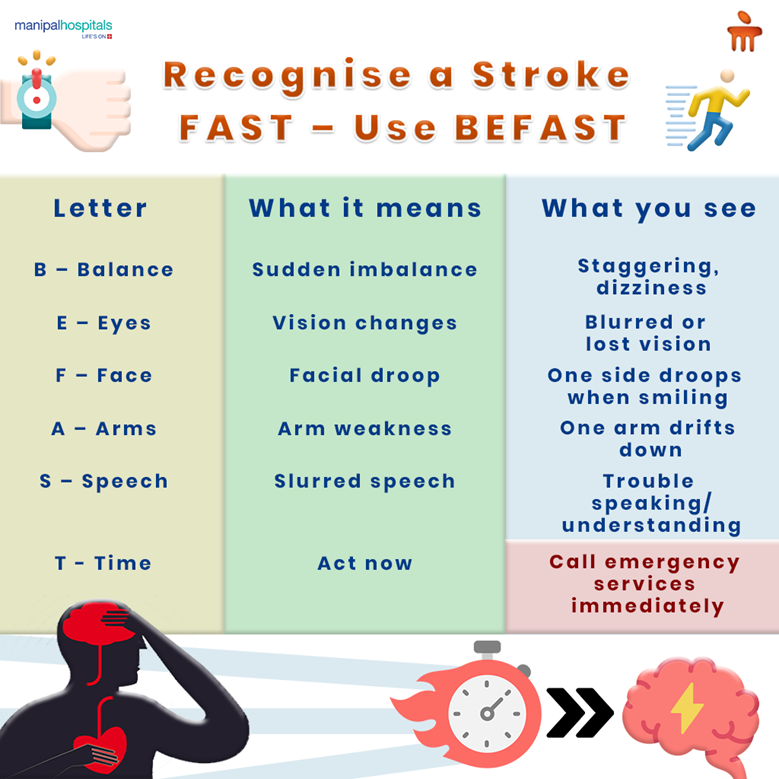
Use the BEFAST METHOD
|
B – Balance |
Sudden loss of balance or coordination |
|
E – Eyes |
Sudden trouble seeing in one or both eyes |
|
F – Face |
Drooping on one side of the face |
|
A – Arms |
Weakness or numbness in one arm (ask the person to raise both arms) |
|
S – Speech |
Slurred or strange speech |
|
T – Time |
Call emergency services right away – don’t wait! |
If you notice any of these signs in yourself or someone else, contact emergency services immediately and get help.
How to Know If I am at Risk of Stroke?
Some risk factors you cannot change, but many you can control. Knowing your risks helps you act before a stroke happens. Non-modifiable factors include:
-
Age (risk increases as we get older)
-
Family history or previous stroke/TIA
-
Being male (men have a slightly higher risk)
But many risk factors are modifiable, such as:
-
High blood pressure & high cholesterol
-
Diabetes
-
Smoking and alcohol consumption
-
Obesity and a sedentary lifestyle
-
Stress and poor diet
Golden Hour in Stroke: Why Every Minute Counts
The term ‘Golden Hour’ holds high relevance in stroke care as it refers to the critical time frame during which administering treatment brings the best results. The first 6 hours from the time of unwell is known as the “golden hour”. During this period, maximum interventions can be carried out, leading to higher chances of recovery.
Treatment for Stroke
The right treatment depends on the type of stroke and how quickly you arrive at the hospital. Quick, targeted care can dramatically improve outcomes.
Ischemic Stroke Treatment:
-
Clot-busting medicines are given through a vein when you arrive within the treatment window and meet criteria.
-
Mechanical thrombectomy, a procedure to remove the clot from the blocked artery using advanced endovascular tools, for selected patients.
Hemorrhagic Stroke Treatment:
-
Measures to control bleeding and reduce pressure in the brain.
-
Surgical or radiological procedures to repair ruptured vessels when indicated.
Rehabilitation and Recovery:
-
Early and intensive stroke recovery programmes that include physiotherapy, speech therapy, and occupational therapy help you regain function and independence.
-
Multidisciplinary teams tailor rehab to your needs so you can return to daily life as fully as possible.
Can Strokes Be Prevented?
Yes. Many strokes are preventable through sustained lifestyle changes and medical care. Prevention reduces the chance you will need emergency treatment.
-
Eat a healthy diet (low in salt, sugar, and unhealthy fats)
-
Exercise regularly
-
Quit smoking and limit alcohol
-
Keep blood pressure, cholesterol, and blood sugar under control
-
Take your doctor’s prescribed medicines regularly
-
Include a carotid Doppler study in your routine annual health check-ups after 50 years or if you have a strong family history of stroke
Life After a Stroke
Recovery doesn’t stop at the hospital. Many people need ongoing rehabilitation and emotional support. This may include:
-
Physiotherapy for strength and mobility
-
Speech therapy for communication challenges
-
Occupational therapy for everyday activities
-
Support groups for patients and caregivers
-
Mental health support for depression or anxiety
Caregivers play a vital role and should remember to care for their own health and well-being, too.
We Are A Stroke Ready Hospital.
Manipal Hospital Kanakapura Road is a 24×7 stroke‑ready hospital equipped with all essential facilities, cutting‑edge technology and diagnostics. We have a dedicated team of specialist doctors in Interventional Neuroradiology, who ensure faster and effective minimally invasive treatment for stroke patients under one roof. Through our dedicated stroke care unit, we offer continuous monitoring and personalized care to help patients achieve better recovery and maximize their chances of a good outcome.
FAQ's
BEFAST is a quick checklist to spot stroke signs: Balance, Eyes, Face, Arms, Speech, Time. Use it immediately; rapid action improves survival and reduces long-term disability.
Call emergency services right away, note when symptoms began, keep the person safe and calm, do not give food or medicines, and get them to a hospital offering acute stroke treatment.
Many strokes are preventable through stroke prevention: control blood pressure, manage diabetes, stop smoking, eat a balanced diet, exercise, and consider carotid Doppler screening after age 50 or with a strong family history.
An ischemic stroke requires urgent care within a narrow treatment window, often hours. Early clot-busting drugs or mechanical thrombectomy greatly improve outcomes. Go to a centre with a 24/7 stroke care unit.
Stroke recovery includes physiotherapy, speech and occupational therapy, psychological support, and secondary prevention. Recovery varies, but consistent rehabilitation, caregiver involvement, and medical follow-up improve independence and quality of life.





















 8 Min Read
8 Min Read