Have you ever wondered what really controls a child’s growth, energy levels, mood, or even the start of puberty?
Well, the answer lies within a delicate network called the endocrine system. The body’s internal messaging service is made up of glands and hormones that keep everything in balance. When something goes wrong in this system, it can affect how a child grows, develops, and even feels. That’s where pediatric endocrinologists come in—doctors who specialize in understanding and treating hormone-related problems in children and teenagers. Let’s take a closer look at what they do and how early awareness can make a difference for a growing child.
Synopsis
- Hormones and Children’s Growth
- Early Detection Makes All the Difference
- The Role of a Paediatric Endocrinologist
- When Should You Visit a Paediatric Endocrinologist?
- How Hormone Testing Works
- What Makes Paediatric Endocrine Care Unique?
- The Bigger Picture: Collaboration and Long-term Care
- Empowering Parents: What to Watch For
- Conclusion
Hormones and Children’s Growth
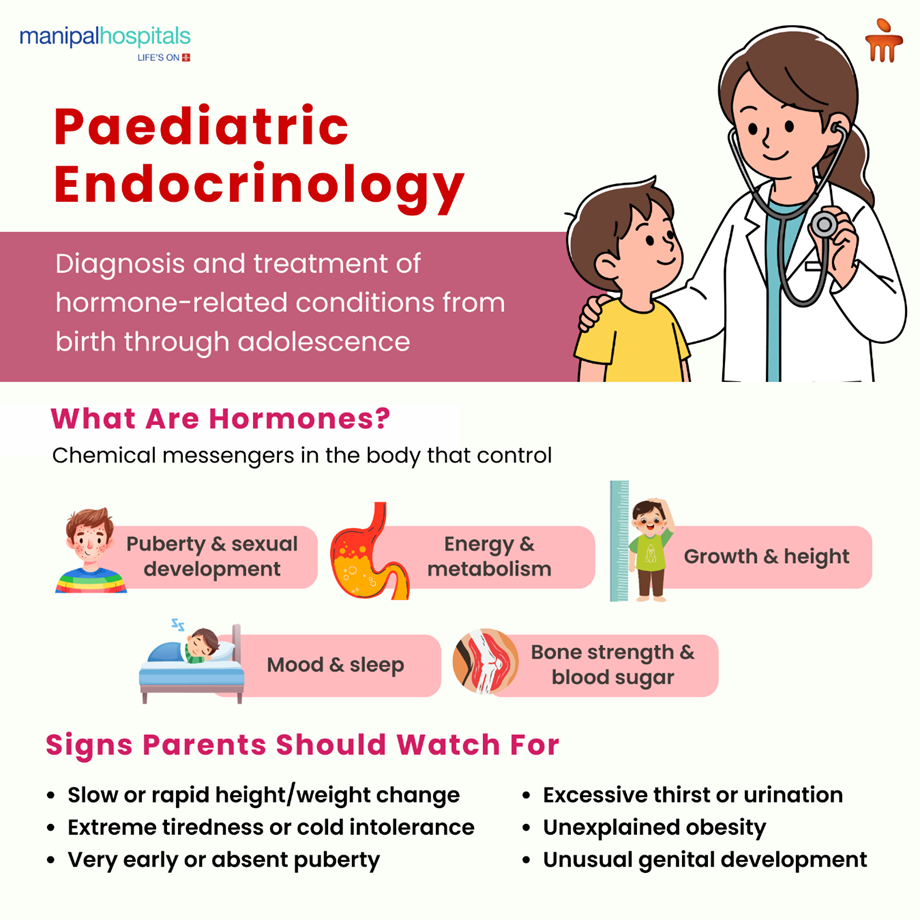
Hormones are like chemical messengers that travel through the bloodstream, telling different organs what to do and when to do it. They control every aspect of our body functions, from day-to-day metabolism to growth, puberty, appetite, sleep, mood, and so on.
In childhood, the most visible sign of healthy hormone function is steady growth. On average, a child reaches half of their adult height by 2 years of age and around 80% by age 10. The rest happens during puberty, when a sudden surge of hormones causes the final stretch of growth.
But growth can easily be disrupted by nutritional deficiencies, chronic illness, or lack (or excess) of specific hormones such as thyroid or growth hormone. Since growth stops once puberty ends (around 14 years in girls and 16 years in boys), early recognition and treatment are critical.
If a parent notices that their child’s height isn’t increasing as expected, or puberty seems unusually early or delayed, it’s always worth consulting a paediatric endocrinologist rather than waiting it out.
Early Detection Makes All the Difference
Hormones play vital roles long before a baby is even born. In fact, some hormone-related disorders begin in the womb. Detecting them early can be life-saving or brain-saving.
Take congenital hypothyroidism, a condition where the thyroid gland doesn’t produce enough hormone. A baby with this condition might look perfectly healthy at birth, yet if untreated, it can lead to severe, irreversible intellectual disability and poor growth. That’s why most hospitals perform a simple newborn screening test to check thyroid function soon after birth. Early diagnosis and treatment with thyroid hormone tablets ensure completely normal development.
Another example is congenital adrenal hyperplasia (CAH), where a baby’s adrenal glands cannot make essential hormones properly. With early detection through newborn screening, doctors can start treatment immediately and prevent potentially life-threatening crises.
The message is simple: when it comes to hormones, time matters. The earlier the problem is found, the better the outcome.
The Role of a Paediatric Endocrinologist
A paediatric endocrinologist is a doctor who has first trained in paediatrics and then undergone additional years of specialised training in hormones and metabolism. Their focus is on children, from tiny newborns to young adults, because hormone patterns in children are very different from those in adults.
In children, hormone levels are constantly changing: they drive height gain, bone development, puberty, and even sleep and appetite. So, when these delicate balances are disturbed, the effects can be dramatic but also reversible with the right care. These specialists don’t just treat illness; they support healthy growth and development, helping children reach their full potential.
When Should You Visit a Paediatric Endocrinologist?
Pediatric endocrinology covers a wide range of conditions, some common, others rare, but all potentially life-changing if missed. Here are a few common concerns parents have when they bring their kids to a pediatric endocrine doctor in Kanakapura Road:
|
Childhood Diabetes |
Type 1 diabetes is common in children and requires careful monitoring of blood glucose, insulin therapy, and family education. Newer tools like insulin pumps and continuous glucose monitoring (CGM) make management much easier. |
|
Growth Concerns |
When a child’s height is well below (or above) the expected range for their age, further evaluation is warranted. Some children may need growth hormone therapy if a deficiency is found. |
|
Puberty Problems |
Some children start puberty too early, while others have a significant delay. Both situations can cause emotional and physical stress, but most are treatable once the underlying cause is identified. |
|
Thyroid Disorders |
Both underactive and overactive thyroid glands can affect growth, learning, and energy levels. |
|
Childhood Obesity |
It can be associated with comorbidities, which can lead to chronic diseases such as diabetes, hypertension, heart disease, etc., if not detected early. Sometimes, weight gain can be out of proportion to diet and activity, which may indicate an underlying hormonal abnormality |
|
Adolescent PCOS (Polycystic Ovary Syndrome) |
Irregular periods, acne, or excessive hair growth in teenage girls may indicate a hormonal imbalance. |
|
Calcium and Bone Problems |
Conditions like rickets (soft bones) or early osteoporosis sometimes stem from endocrine causes. |
Beyond these, paediatric endocrinologists also manage rarer and more complex issues, such as adrenal gland disorders, pituitary hormone deficiencies, disorders of sex development (DSD), and hormonal side effects of chronic illnesses or cancer treatments.
Because many of these conditions overlap with other medical systems, paediatric endocrinologists often work in multidisciplinary teams, alongside paediatricians, dietitians, geneticists, psychologists, and surgeons, to deliver coordinated, child-centred care.
How Hormone Testing Works
When you visit a paediatric endocrinologist, the first step is usually a detailed history and examination. Depending on the child’s symptoms, the doctor may recommend specific hormone tests.
Most hormones can be measured through blood samples, though some are checked in urine. Timing is crucial: many hormones vary throughout the day or with sleep, food, or stress. For example:
-
Thyroid hormones (T3 and T4) are controlled by the pituitary hormone TSH. Low T3/T4 with high TSH suggests an underactive thyroid, while low values of all three might point to a pituitary problem.
-
Cortisol, a stress hormone, is highest in the early morning and lowest at night, so blood tests are timed accordingly.
-
Growth hormone (GH) is secreted in bursts, mostly during sleep. Because it’s not continuously released, a single blood test often shows a “low” value even in healthy children. To diagnose GH deficiency accurately, a test that stimulates growth hormone is performed, measuring hormone levels after giving a medication that triggers GH release.
Other “dynamic tests,” such as the ACTH stimulation test (for adrenal function) or the GnRH test (for puberty evaluation), help doctors understand how well a child’s hormone systems respond to challenge.
These investigations sound complex, but they’re carefully done in hospital settings under expert supervision, and the results guide precise treatment plans.
What Makes Paediatric Endocrine Care Unique?
Children are constantly growing and changing. A hormone imbalance can therefore affect not just current health but also future height, bone strength, fertility, and emotional well-being.
This is why children with hormonal conditions need specialists who understand these differences. Managing diabetes in a 10-year-old, for instance, is not the same as in an adult; the goals, lifestyle, and growth factors are all different. Similarly, puberty-related issues require not just medical treatment but sensitive guidance for both the child and the parents.
Pediatric endocrinologists also spend time educating families, helping them understand lab results, medication routines, and the importance of follow-up. Because many endocrine disorders are chronic, continuity of care and trust are essential.
The Bigger Picture: Collaboration and Long-term Care
Modern paediatric endocrinology is increasingly team-based. For example, a child with obesity might be seen in a comprehensive clinic with a nutritionist, physiotherapist, and psychologist. A cancer survivor may need ongoing hormonal follow-up after chemotherapy or radiotherapy.
Children born with DSD or genetic endocrine syndromes are supported by coordinated teams including surgeons, counsellors, and genetic experts.
This collaborative approach ensures that every aspect of a child’s growth, health, and self-esteem is cared for, not just their lab numbers.
Empowering Parents: What to Watch For
While not every growth variation means a serious problem, parents often notice subtle signs first. Here are a few red flags worth discussing with your paediatrician:
-
Unexplained slowing or acceleration of height or weight gain
-
Excessive tiredness, constipation, or feeling unusually cold (possible thyroid concerns)
-
Early or absent puberty changes
-
Excessive thirst or frequent urination (could signal diabetes)
-
Persistent weight gain despite a reasonable diet and activity
-
Ambiguous genitalia in a newborn or unusual body hair patterns in older children
Trust your instincts; early evaluation can rule out serious issues or catch them while treatment is most effective.
Conclusion
Paediatric endocrinology is an ever-evolving field. Advances in genetic testing, continuous glucose monitoring, and telemedicine are transforming how doctors diagnose and treat hormonal disorders. What remains constant is the goal: helping children grow, thrive, and live full, healthy lives.
Behind every height chart and lab report lies a story of a child learning to manage diabetes, a teen gaining confidence through balanced hormones, or a newborn saved by early diagnosis. For parents, knowing that such specialised care exists is reassuring. Hormones may be invisible, but their impact is everywhere, and with the right support, every child can reach their best potential.If you want expert guidance for your child, consult a paediatric endocrinologist at Manipal Hospital on Kanakapura Road.
FAQ's
If growth slows, drops off the growth chart, or doesn’t match family height patterns, it’s worth checking. A paediatric endocrinologist looks at growth over time, not just one measurement, and can tell if it’s normal variation or something treatable.
Sometimes yes, but not always. Early or delayed puberty can affect both physical and emotional health. An evaluation helps identify whether hormones are driving the change and whether reassurance, monitoring, or treatment is needed.
Yes, ongoing fatigue, poor concentration, or low energy can sometimes signal thyroid or other hormone issues. A paediatric endocrinologist can check whether hormones are involved or if there’s another underlying cause needing attention.
Most tests involve simple blood samples. Some specialised “dynamic tests” take longer but are done under close medical supervision. They are safe, carefully planned, and provide important information to guide accurate treatment.
Not necessarily. Some conditions need short-term treatment, others long-term monitoring. Many visits result in reassurance alone. The goal is always to support healthy growth and development, using the least intervention needed.





















 7 Min Read
7 Min Read