Let’s understand in detail. At its simplest, liver cirrhosis means the liver has developed severe scarring. That scar tissue replaces healthy liver cells and slowly robs the organ of its ability to work properly. Because the liver does so many vital jobs, filtering toxins, helping digestion, making proteins and clotting factors, the effects of liver cirrhosis ripple through the whole body.
Not everyone with liver scarring feels ill at first. In fact, many people are surprised when liver cirrhosis is discovered during tests for something else. That’s why recognising the causes, spotting early warning signs of worsening disease, and acting promptly are so important. With timely care, you can slow progression, treat complications, and, in selected cases, be offered a lifesaving liver transplant. Through this blog, a leading hepatologist and liver transplant specialist in Kanakapura Road, Bangalore, walks you through what causes liver cirrhosis, what are the symptoms of liver cirrhosis, the complications to watch for, and practical steps you or someone you care for can take now.
Synopsis
What Is Liver Cirrhosis?
Liver cirrhosis is the end result of long-standing liver injury. When the liver is injured repeatedly, by alcohol, chronic viral infection, metabolic dysfunction leading to fatty liver, autoimmune attack, or genetic disorders, it tries to repair itself. Over time, that repair process creates bands of scar tissue. Initially, this scarring is called fibrosis; when it becomes extensive and disrupts liver architecture and function, we call it liver cirrhosis.
There are 2 clinical stages that matter for you and your doctor:
|
Compensated cirrhosis |
The liver is scarred but still managing its job well enough that the person has few or no obvious symptoms. Life can feel normal. |
|
Decompensated cirrhosis |
The liver can no longer cope and clear signs of liver failure appear. These complications are serious and need urgent attention. |
Common Causes of Liver Cirrhosis in India
Various problems can damage the liver and, if untreated, lead to liver cirrhosis. The most frequent causes you will see are:
-
Alcohol-related liver disease. Heavy, prolonged drinking causes inflammation (hepatitis) that progresses to fibrosis and then cirrhosis in some people.
-
Metabolic dysfunction–related fatty liver (MASLD/NAFLD). Even in people who do not drink alcohol, excess calories, being overweight, and insulin resistance can lead to fat accumulation in the liver, then inflammation (steatohepatitis), fibrosis and liver cirrhosis.
-
Viral hepatitis. Chronic hepatitis B and C infections cause ongoing liver inflammation and are important causes of liver cirrhosis.
-
Autoimmune liver disease. The immune system sometimes attacks the liver, producing silent inflammation that can progress. These conditions are more common in women but can affect anyone.
-
Genetic and metabolic liver disorders. Several inherited conditions slowly damage the liver over the years.
Understanding the root cause matters because treatment focuses both on managing complications and on stopping or reversing the underlying process where possible.
What is “Metabolic Dysfunction” and Why Does it Matter?
In India, metabolic dysfunction is a major driver of fatty liver and cirrhosis. When your body stores excess fat, especially around the belly, that visceral fat interferes with how your liver handles fats and sugars. Over time, this leads to fatty change and inflammation. Clinically, metabolic dysfunction is signalled by one or more of the following features (you’ll see these used by doctors when they assess risk):
-
Body mass index (BMI) greater than 23 or increased waist circumference (men > 90 cm, women > 80 cm)
-
Diabetes or prediabetes
-
High blood pressure
-
Raised triglycerides (the “bad” fat)
-
Low HDL cholesterol (the “good” cholesterol)
If you have any one of these, your risk of fatty liver and later fibrosis rises. The good news: many of these factors respond well to lifestyle change.
What are the Symptoms of Liver Cirrhosis?
Liver cirrhosis doesn’t develop overnight. There is usually a long period of inflammation and fibrosis before severe scarring sets in. Crucially, the liver can compensate for a long time, so you may not notice symptoms until complications appear.
When liver cirrhosis progresses to decompensation, several key problems may occur:
-
Fluid accumulation (ascites and oedema). Fluid may collect in the belly (ascites) or legs, causing discomfort and breathlessness.
-
Jaundice. Yellowing of the eyes or skin and darker urine happen when bilirubin rises because the liver cannot clear it.
-
Variceal bleeding. Scarring increases pressure in the portal blood vessels. Tiny swollen veins (varices) in the throat or stomach can rupture and cause vomiting of blood or black stools; this is life-threatening.
-
Hepatic encephalopathy. The liver can no longer clear toxic substances like ammonia; this can cause confusion, sleepiness, poor concentration or “brain fog.”
-
Risk of liver cancer (hepatocellular carcinoma). Patients with liver cirrhosis need regular surveillance because the risk of liver cancer is higher.
The number and severity of these decompensations determine how unwell someone becomes. Early treatment can often control complications and improve quality of life; in some cases, liver transplant becomes the best option.
How Doctors Approach Treatment
When a patient presents with liver cirrhosis or risk factors, the hepatologist (liver specialist) will do two things in parallel: find and treat the root cause, and manage the complications.
1. Treat the cause
-
If alcohol is responsible, stopping alcohol is essential.
-
Viral hepatitis is treated with modern antiviral medicines that can halt progression and sometimes clear the virus.
-
Metabolic dysfunction is addressed with weight loss, diet and exercise and control of diabetes and lipids.
-
Autoimmune or genetic conditions are treated as appropriate with immunosuppression or specialist therapies.
2. Manage complications and support the liver
-
Ascites: Low salt intake and diuretics are first-line measures. In some cases, procedures to drain fluid or place a shunt are needed. Adequate protein intake (about 1.5 g/kg/day) is usually recommended for those with ascites to prevent malnutrition, alongside salt restriction.
-
Variceal bleeding: Endoscopic techniques (banding) and medicines to reduce portal pressure are used to prevent and treat bleeding.
-
Hepatic encephalopathy: Controlling constipation, using medications that reduce ammonia production, and dietary measures help prevent brain fog episodes.
-
Surveillance for liver cancer: Regular ultrasound and blood tests (as advised by your hepatologist) to detect cancer early.
-
Liver transplant: For patients with repeated or severe decompensation, transplantation is a definitive option. Outcomes are good when performed by experienced teams
Every plan is individualised. The hepatologist balances treating the liver, controlling symptoms, maintaining nutrition and planning surveillance or transplant when needed.
Practical Steps You Can Take Now
If you are worried about liver cirrhosis, or you have risk factors, these practical steps help reduce risk and detect problems early:
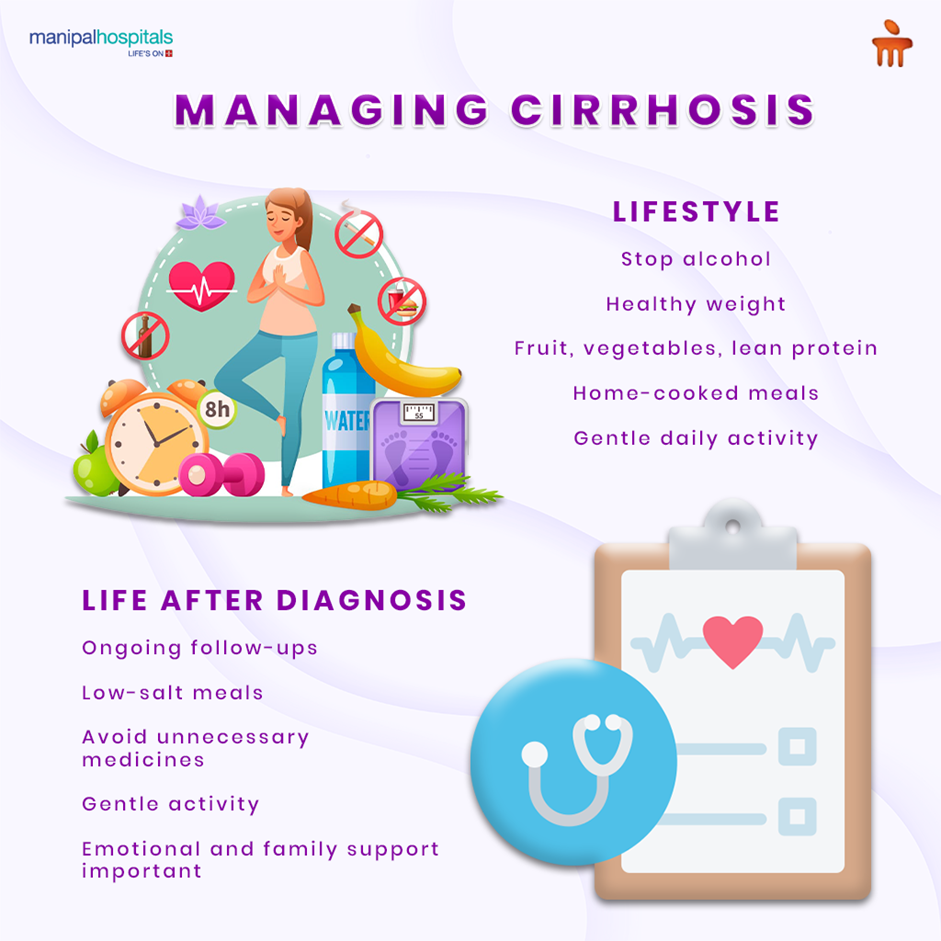
- See your hepatologist if you have long-standing liver disease, persistent abnormal liver tests, or any risk factors described above.
-
Stop alcohol; if alcohol is a factor, continued drinking accelerates damage.
-
Manage weight and metabolic health. Aim for gradual, sustainable weight loss through a balanced diet and regular activity.
-
Control diabetes and blood pressure. Good control reduces liver stress.
-
Avoid unnecessary medicines and toxins. Use medicines only as advised and be cautious with over-the-counter drugs.
-
Follow medical surveillance. If you have liver cirrhosis, keep scheduled tests to watch for complications and liver cancer.
-
Ask about vaccination. If you are not immune to hepatitis A or B, vaccination can prevent new infections that would further damage the liver.
When to Seek Urgent Care
Some symptoms mean you should get immediate medical attention:
-
Vomiting blood or passing black stools
-
Sudden worsening of confusion or drowsiness
-
Rapidly increasing belly swelling or severe abdominal pain
-
Yellowing of the eyes or skin that develops quickly
These can be signs of life-threatening decompensation and need emergency evaluation.
Can Liver Cirrhosis be Reversed?
The answer depends on the stage. Early fibrosis and the beginning of liver cirrhosis may stabilise and even improve when the cause is treated and lifestyle changes are made. Once advanced cirrhosis with architectural distortion and repeated decompensations is established, complete reversal is unlikely. However, modern treatments can slow progression, treat complications effectively, and in many cases again return you to a good quality of life. For those with end-stage disease, liver transplantation offers a real chance of long-term survival.
Conclusion
Liver cirrhosis is a serious condition, but it is not a sudden death sentence. Understanding the causes, alcohol, metabolic dysfunction, viruses, autoimmune or genetic disorders, and acting early changes everything. If your liver is scarred but still compensated, you have the greatest opportunity to stabilise and protect what remains of liver function. If decompensation occurs, modern care can manage complications, and transplantation offers hope for many.
If you have risk factors such as heavy alcohol use, fatty liver on imaging, diabetes, abdominal obesity, or chronic viral hepatitis, consult an experienced hepatologist. Early diagnosis, targeted treatment, and sensible lifestyle changes together make the difference between progressive decline and long, healthy years ahead.
FAQ's
Fibrosis is the early scarring that follows liver injury. When scarring becomes severe enough to disrupt normal liver structure and function, it is called cirrhosis.
Not necessarily. Fatty liver is common and reversible in many people who lose weight and improve their metabolism. However, if it progresses to steatohepatitis (inflammation) and is left untreated, fibrosis and later liver cirrhosis can develop. Early action matters.
Yes. Even in early liver cirrhosis, stopping alcohol, losing excess weight, controlling blood sugars and blood pressure, and following medical advice reduces complications and slows disease progression.
Not always. Many complications can be controlled medically or with procedures. Transplant is considered when decompensation is severe or recurrent despite the best medical care. Discuss candidacy and timing with your hepatologist.





















 7 Min Read
7 Min Read


_Causes_Risks_and_Treatment.png)




.png)